Abstract
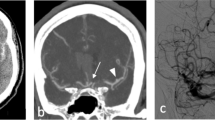
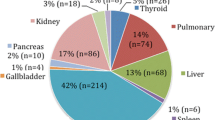
The purpose of this study was to determine the discrepancy rates of radiology residents interpreting emergent neck and Circle of Willis magnetic resonance angiography (MRA) studies and to detect any adverse clinical outcomes. Three hundred seventeen MRA studies given preliminary reading by radiology residents were retrospectively reviewed over a 2-year period. Discrepancies were classified as either false negatives (failure to diagnose abnormalities) or false positives (misinterpreting normal scans as abnormal). The overall discrepancy rate was 12.1% for Circle of Willis MRA and 7.9% for neck MRA. Fourth-year residents had the lowest discrepancy rates (7.7%), but this was not statistically significant. The most common misses were stenosis greater than 70% (n = 9) and aneurysm (n = 12). No adverse clinical outcome was detected mainly due to rapid turnaround time for final reporting.



Similar content being viewed by others
References
Wysoki MG, Nassar CJ, Keonigsberg RA et al (1998) Head trauma: CT scan interpretation by radiology residents versus staff radiologists. Radiology 208:125–128
Funaki B, Szymski GX, Rosenblum JD (1997) Significant on-call misses by radiology residents interpreting computed tomographic studies: perception versus cognition. Emerg Radiol 4:290–294. doi:10.1007/BF01461735
Roszler MH, McCarroll KA, Rashid T et al (1991) Resident interpretation of emergency computed tomographic scans. Invest Radiol 26:374–376. doi:10.1097/00004424-199104000-00016
Lal NR, Eldevik OP, Murray UM et al (2000) Clinical consequences of misinterpretations of neurologic CT scans by on-call radiology residents. AJNR Am J Neuroradiol 21:124–129
Erly WK, Berger WB, Krupinski E et al (2002) Radiology resident evaluation of head CT scan orders in the emergency department. AJNR Am J Neuroradiol 23:103–107
Le A, Licurse A, Catanzano TM (2007) Interpretation of head CT scans in the emergency department by fellows versus general staff non-neuroradiologists: a closer look at the effectiveness of a quality control program. Emerg Radiol 14:311–316. doi:10.1007/s10140-007-0645-6
Strub WM, Vagal AA, Tomsick T et al (2006) Overnight resident preliminary interpretations on CT examinations: should the process continue? Emerg Radiol 13:19–23. doi:10.1007/s10140-006-0498-4
Filippi CG, Schneider B, Burbank HN et al (2008) Discrepancy rates of radiology resident interpretations of on-call neuroradiology MR imaging studies. Radiology 249(3):972–979. doi:10.1148/radiol.2493071543
Ruchman RB, Jaeger J, Wiggins EF et al (2007) Preliminary radiology resident interpretations versus final attending radiologist interpretations and the impact on patient care in a community hospital. AJR 189:523–526. doi:10.2214/AJR.07.2307
Strub WM, Leach JL, Ying J et al (2007) First year radiology residents not taking call: will there be a difference? Emerg Radiol 13:231–235. doi:10.1007/s10140-007-0571-7
Seltzer SE, Hessel SJ, Herman PG et al (1981) Resident film interpretation and staff review. AJR 137:129–133
Erly WK, Ashdown BC, Lucio RW et al (2003) Evaluation of emergency CT scans of the head: is there a community standard? AJR 180:1727–1730
Velmahos GC, Fili C, Vassiliu P et al (2001) Around-the-clock attending radiology coverage is essential to avoid mistakes in the care of trauma patients. Am Surg 67:1175–1177
Yoon LS, Haims AH, Brink JA et al (2002) Evaluation of an emergency radiology quality assurance program at a level I trauma center: abdominal and pelvic CT studies. Radiology 224:42–46. doi:10.1148/radiol.2241011470
Wechsler RJ, Spettell CM, Kurtz AB et al (1996) Effects of training and experience in interpretation of emergency body CT scans. Radiology 199:717–720
Herman PG, Hessel SJ (1975) Accuracy and its relationship to experience in interpretation of chest radiographs. Invest Radiol 10:62–67. doi:10.1097/00004424-197501000-00008
Branstetter BF, Morgan MR, Nesbit CE et al (2007) Preliminary reports in the emergency department: is a subspecialist radiologist more accurate than a radiology resident? Acad Radiol 14(2):201–206. doi:10.1016/j.acra.2006.11.001
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Filippi, C.G., Meyer, R.E., Cauley, K. et al. The misinterpretation rates of radiology residents on emergent neuroradiology magnetic resonance (MR) angiogram studies: correlation with level of residency training. Emerg Radiol 17, 45–50 (2010). https://doi.org/10.1007/s10140-009-0820-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-009-0820-z