Abstract
Background
Intraperitoneal administration of paclitaxel had been considered a promising option to treat peritoneal metastasis, the most frequent pattern of recurrence in gastric cancer after D2 gastrectomy, but its safety and efficacy after gastrectomy had not been fully explored.
Methods
A phase II randomized comparison of postoperative intraperitoneal (IP) vs. intravenous (IV) paclitaxel was conducted. Patients with resectable gastric linitis plastica, cancer with minimal amount of peritoneal deposits (P1), or cancer positive for the peritoneal washing cytology (CY1) were eligible. After intraoperative confirmation of the above disease status and of resectability, patients were randomized to be treated either by the IP therapy (paclitaxel 60 mg/m2 delivered intraperitoneally on days 0, 14, 21, 28, 42, 49, and 56) or the IV therapy (80 mg/m2 administered intravenously using the identical schedule) before receiving further treatments with evidence-based systemic chemotherapy. The primary endpoint was 2-year survival rate.
Results
Of the 86 patients who were randomized intraoperatively, 83 who actually started the protocol treatment were eligible for analysis (n = 39, IP group; n = 44, IV group). The 2-year survival rate of the IP and IV groups was 64.1% (95% CI 47.9–76.9) and 72.3% (95% CI 56.3–83.2%), respectively (p = 0.5731). The IP treatment did not confer significant overall or progression-free survival benefits, and was associated with particularly poor performance in patients with residual disease, including the CY1 P0 population.
Conclusions
We were unable to prove superiority of the IP paclitaxel over IV paclitaxel delivered after surgery to control advanced gastric cancer with high risk of peritoneal recurrence.
Similar content being viewed by others
Introduction
Peritoneal metastasis is one of the most frequent causes of recurrence and death among patients with advanced gastric cancer and often occurs after D2 gastrectomy which is considered to confer excellent local control [1]. Disseminated nodules can only be detected at laparotomy or laparoscopy as minute deposits adhered to the peritoneal surface, and are often preoperatively undetectable even with the states of the arts modalities such as computed tomography, ultrasound, and positron emission tomography [2]. These minute deposits, nevertheless, deem the disease oncologically unresectable, because they are usually accompanied with numerous other metastatic foci on the peritoneal surface that remain too small to be macroscopically detectable. Moreover, response to the chemotherapeutic agents is generally reported to be poor, at least partially owing to the insufficient transition of the drugs into the peritoneal cavity [3].
The origin of peritoneal metastasis is considered to be free cancer cells which are either shed from the gastric serosa in case of T4-stage disease or disseminated through surgical manipulation [4]. Detection of free cancer cells by cytological examination of the peritoneal washes is designated as CY1 in the Japanese Classification of Gastric Carcinoma [5], and denotes poor prognosis even in the absence of macroscopic peritoneal deposits [4]. Therefore, a treatment strategy designed to directly make contact with the free cancer cells through intraperitoneal (IP) administration of anticancer drugs may serve as an effective approach for prevention or treatment of the peritoneal disease [6].
Intravenous (IV) paclitaxel has been approved for treatment of gastric cancer, and is currently a standard of care in the second line setting [7, 8]. Paclitaxel is known to exhibit high intraperitoneal concentration even when administered IV [3]. When delivered IP, however, the intraperitoneal concentration of paclitaxel reportedly rises to 1000-folds that reached by IV and maintains the high values for several days [9]. Moreover, repeated IP administration of paclitaxel has been proven to be safe and effective for treating disseminated ovarian cancer [10]. A phase III trial eventually proved efficacy of intraperitoneal paclitaxel in combination with platinum in ovarian cancer [11]. However, little evidence in support of the IP treatment was available for gastric cancer.
Before embarking on exploring more complex treatment regimens in combination with other drugs and systemic therapy, we aimed to make a head-to-head comparison of IP vs. IV paclitaxel as a single agent for gastric cancer with high risk of peritoneal disease [12]. IP paclitaxel was found to be safe and feasible in the current multi-institutional randomized phase II trial (INPACT trial), and these results have been published [13]. Here, we report on the final analyses including survival outcomes of the trial.
Patients and methods
Ethics
This randomized, open-label multicenter phase II trial was approved by the institutional review boards of the 12 participating institutes after review of the scientific and ethical validity of the protocol. This study fully complied with the Declaration of Helsinki (2008) and is registered with the University Hospital Medical Information Network (UMIN) Clinical Trial Registry (UMIN000002957; http://www.umin.ac.jp/ctr/index.htm). Written informed consent was obtained from all patients before enrollment. Because IP administration of paclitaxel has not been approved by the insurance system in Japan, the current trial was conducted as Advanced Medical Treatment B scheme under approval of the Ministry of Health, Labor and Welfare.
Inclusion and exclusion criteria
The primary target population of the study was comprised with individuals with potentially resectable advanced gastric cancer at particularly high risk of peritoneal metastasis. Patients were registered preoperatively if they met all of the inclusion criteria following preoperative examination which included computed tomography of the neck, chest and whole of the abdominal cavity:
-
(1)
Histologically proven adenocarcinoma of the stomach.
-
(2)
Either macroscopically type-3 cancer with a tumor diameter ≥ 8 cm estimated by the endoscopic examination or barium swallow, type-4 (linitis plastica) cancer, suspected to have small quantities of peritoneal deposits, or confirmed to be positive for the peritoneal-wash cytology.
-
(3)
Without metastases in the cervical, mediastinal, paraaortic, or other distant lymph nodes, to the distant organs such as the liver and lung, or with a large amount of ascites overflowing beyond the pelvic cavity.
-
(4)
Absence of clinical manifestations indicating distant metastases.
-
(5)
Absence of a history of chemotherapy or radiotherapy.
-
(6)
Eastern Cooperative Oncology Group performance status 0–1.
-
(7)
Age ≥ 20 years.
-
(8)
Sufficient organ functions indicated by laboratory data acquired within 7 days before surgery.
-
(9)
Absence of severe arrhythmia.
Key exclusion criteria were as follows: severe comorbidity, gastrointestinal bleeding requiring repeated blood transfusions, and bowel obstruction preventing treatment with oral drugs, active synchronous cancer or disease-free metachronous cancer within 5 years from the onset of gastric cancer, peripheral neuropathy, and also patients who were otherwise considered inappropriate for inclusion by the physicians.
Intraoperative randomization
Patients were randomized during laparotomy to the IP or IV group after confirmation by the surgeons that (1) gastrectomy is possible, (2) patient has risk factors for peritoneal metastasis/recurrences (either with small quantities of peritoneal disease that did not discourage surgeons from performing gastrectomy, fulfills to the type 3/4 criterion written above, or is positive for the peritoneal washing cytology), and (3) placement of the indwelling catheter is possible. The randomization was performed by centralized dynamic weighting method. Upon randomization, patients were stratified by the following factors: the macroscopic type (type 3/4 or others), curability of surgery (R0 or R1/R2), age (< 75 years or ≥ 75 years), and institution.
In the IP group, placement of the indwelling catheter was performed according to the method of Markman and Walker to avoid catheter-associated adverse events [14].
Postoperative treatment and patient follow-up
Seven cycles of paclitaxel administration on the same postoperative days were planned for both treatment groups. The IP group received 60 mg/m2 of paclitaxel on the day of surgery (day 0) and on days 14, 21, 28, 42, 59, and 56 after surgery. Paclitaxel was dissolved in 1000 mL saline and delivered to the abdominal cavity via the indwelling catheter except on day 0 when the drug was administered through the transient catheter which was introduced through the small opening that remained at either end of the midline incision and was retrieved as the last suture of the wound closure was tied. The dose had been decided based on a phase II trial of paclitaxel monotherapy through IP administration conducted in ovarian cancer patients (11). In the IV group, patients received 80 mg/m2 of paclitaxel on the day of surgery (day 0) and on days 14, 21, 28, 42, 49, and 56. These treatment regimens were to be followed 2–3 weeks later by standard systemic chemotherapy for advanced gastric cancer which, at the time the trial started, was either S-1 monotherapy [15] or a combination of S-1 and cisplatin [16]. S-1 was recommended for Stage III cancer and S-1/cisplatin for Stage IV, but these treatments were outside of the study protocol and the choice was left to the discretion of the physicians.
Endpoints and statistical analysis
The primary endpoint was the 2-year survival rate. The secondary endpoints were safety, progression-free survival (PFS), and overall survival (OS). The sample size was calculated according to the hypothesis that the 2-year survival rate of the IV group, estimated as 30–40%, could be improved by 10% in the IP group. The selection probability was approximately 82–83% when the sample size was 80 patients and 84–85% when the sample size was 100. Thus, the randomized sample size was designated as 90 patients. Qualitative variables were compared between the two groups using the χ2 test, with the exception of comparison of the chemotherapeutic regimens used in the subsequent treatment where Fisher’s exact test was used. To compare quantitative data, we used the Wilcoxon signed-rank test for between-patient comparisons. The Kaplan–Meier method was used to calculate survival curves, and the stratified log-rank test was used for comparisons. p < 0.05 indicates statistical significance.
Results
Patients’ characteristics
Between June 2011 and November 2014, 177 patients were registered from the 12 participating institutions. A CONSORT diagram is presented in Fig. 1. Several candidates who had been registered were found to be ineligible at surgery due to lack of macroscopic peritoneal deposits and/or negative result in the peritoneal washing cytology, and 86 patients eventually went through to be randomly allocated to either of the treatment arms. Three patients were excluded, of which two patients refused treatment after the randomization. In another patient, surgeons changed their decision after the randomization through finding several additional peritoneal deposits while operating and decided not to perform gastrectomy after all. Thus, 83 patients who underwent the protocol treatment were eligible for analysis. When we compared baseline characteristics between the IP (n = 39) and IV (n = 44) groups, there were no differences in patient demographics and prognostic factors (Table 1).
Details on treatment after the IP or IV paclitaxel were available for all patients except one patient in the IV group. Chemotherapy was delivered after the protocol treatment in 24 of 39 patients in the IP group and 27 of 43 patients in the IV group. There was no difference in the percentage of patients who underwent the subsequent treatment (p = 0.907). The regimen selected by the physicians was 5FU-based, taxane-based, and others in 16, 5, and 3 patients in the IP group and 20, 3, and 4 patients in the IV group, respectively (p = 0.679).
Safety
We previously reported on the feasibility and safety of the protocol treatment [13]. In brief, the incidence of surgical complications was similar between the two groups, except for the fact that transient bowel obstruction was observed exclusively in the IP group. All of these patients were cured without surgical intervention. The treatment completion rates and the relative dose intensities of paclitaxel for the IP and IV groups were 74.4 and 72.7%, and 81.4 and 76.3%, respectively (Table 1). One death occurred because of pulmonary thrombosis in the IV group. Other adverse events were mild and manageable.
Survival
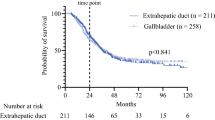
The median PFS and OS of all 83 patients were 658 days (95% confidence interval (CI), 476–844 days) and 1269 days (95% CI, 855 days and upper margin not reached). The 2-year PFS rates of the IP and IV groups were 38.4% (95% CI, 23.1–53.6%) and 46.6%, (95% CI, 30.2–61.3%), respectively (p = 0.5309). The 2-year survival rate, the primary endpoint, was 64.1% (95% CI, 47.0–76.9%) in the IP group and 72.3% (95% CI, 56.3–83.2%) in the IV group, respectively, and was without significant difference (p = 0.5731). The median PFS time of the IP and IV groups were not significantly different at 604 days (95% CI, 321–940 days) and 685 days (95% CI, 426–1134 days), respectively (hazard ratio: 1.148, 95% CI 0.666–1.977, p = 0.6195, Fig. 2a). The median survival time of the IP group was 1270 days (95% CI, 661 days ~ not reached) and that of the DIV group was 1132 days (95% CI, 786 days–not reached). Again, there was no difference between the groups (hazard ratio: 1.157, 95% CI, 0.640–2.091, p = 0.6285, Fig. 2b).
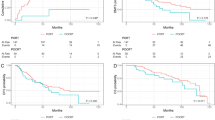
Subgroup analyses
We performed subgroup analyses to further evaluate the influence of drug-administration routes (Table 2 for PFS and Table 3 for OS). Although there was no statistically significant determinant of the PFS or OS (Fig. 3), the effect of IP treatment on PFS was particularly disappointing among patients with residual disease (hazard ratio: 1.848, 95% CI 0.767–4.452). The overall incidence of disease recurrences between the two groups was similar only in the P0CY0 population. Disappointingly, the IP treatment resulted in higher incidences of recurrence and progression in the P0CY1 and P1 cohorts even in the form of peritoneal disease, although not statistically significantly so (Fig. 4).
Incidence of the site of initial recurrence or progression stratified by the treatment arms for the subsets with P0CY0 status, P0CY1 status and P1 status. Although no statistical difference between the arms was observed, recurrence as peritoneal disease tended to be more frequent in the IP group for the P0CY1 and P1 cohorts
Discussion
Efficacy of a combination chemotherapy that includes IP paclitaxel has been proven by a phase III trial in the treatment of ovarian cancer [11], another cancer type with high incidence of peritoneal metastasis, but the evidence have not yet been robust for gastric cancer. Sporadic case reports postulating the efficacy of IP paclitaxel for gastric cancer had been presented in domestic meetings, but the dosage and treatment schedules had been varied. Moreover, no prospective trial result was available at the time preparations for the current study had been in progress. Before embarking on combining IP paclitaxel with other anticancer agents, we sought to establish safety and efficacy of a single agent IP paclitaxel at a dosage that had been decided by a phase II trial for ovarian cancer in the US [10]. Co-resection of the bowel had been reported as a risk factor for major adverse events in the postoperative IP treatment of ovarian cancer [14]. Thus, safety of delivering IP paclitaxel immediately after gastrectomy was an important issue. In the INPACT trial, we could prove safety of IP paclitaxel on the day of radical gastrectomy for the first time in a multi-institutional setting, along with feasibility of the weekly IP treatment [13]. However, we were unable to demonstrate survival benefits of the IP administration over IV.
The IP paclitaxel was developed to enhance antitumor activity against peritoneal metastasis by maintaining a high and persistent concentration of the drug in the peritoneal cavity [9]. On the other hand, a high proportion of paclitaxel that remains in the peritoneal cavity means poor absorption of the drug into the blood stream. Moreover, despite the high concentration in the peritoneal cavity, paclitaxel has been reported not to penetrate deep into the peritoneal wall, and intra-tumoral uptake only from the peritoneal surface may not be sufficient to treat a bulky tumor [6]. IP paclitaxel as a single agent is, therefore, estimated to be suboptimal as a systemic therapy. These facts resulted in dispute when considering the eligibility criteria for this trial, given that an evidence for postoperative adjuvant chemotherapy for advanced gastric cancer already existed [15]. However, the investigators considered a head-to-head comparison between IP and IV paclitaxel as an essential first step before moving on to establishment of the combination therapies. Thus, (i) the target population had to have a high likelihood of developing into peritoneal carcinomatosis and (ii) duration of treatment by IP paclitaxel had to be kept short and was eventually decided to be 8 weeks so as to be able to start the evidence-based systemic treatment without overt delay. On the other hand, a treatment by IV paclitaxel was considered acceptable since feasibility of delivering IV paclitaxel before initiation of oral fluoropyrimidines postoperatively had already been proven [17]. The sequential treatment was actually explored in a large-scale phase III trial and, although that trial failed to prove its superiority, the sequential treatment was eventually observed not to be inferior to the evidence-based treatment in terms of long-term outcome [18].
Gastrectomy for patients with cytology-positive status and those with small amount of peritoneal deposits that could be co-resected had been justified by the Japanese Gastric Cancer Treatment Guidelines pending adequate postoperative chemotherapy [19], based on a prospective phase II study [20] and other retrospective case series [21]. On the other hand, palliative R2 resection for patients with metastatic disease is not indicated except in case of stenosis or hemorrhage. We estimated that a large amount of residual disease after R2 resection would call for a powerful systemic chemotherapy, in which case the patient may not benefit from IP paclitaxel. After much discussion, patients who underwent R2 resection were nevertheless deemed eligible for this trial so as to facilitate the patient accrual. However, as had been feared, the subset analysis denied efficacy of IP paclitaxel to treat patients after R2 resection. Even more disappointingly, IP paclitaxel was unable to control the peritoneal disease even after R1 resection that denotes P0CY1 cases.
The current trial was conducted as Advanced Medical Treatment B scheme in which participating institutions had to be accredited by the government. This process was rather complex and time-consuming, and the study had to be started off with a small number of institutions and the study group never actually grew large enough for a prompt patient accrual. While concept of the study had been under debate by the steering committee of our study group, Ishigami et al. successfully combined IP paclitaxel with systemic chemotherapy and conducted a successful phase II trial, in which they achieved promising outcomes of the 2-year OS at 46% and the median-survival time at 22.5 months among patients with overt peritoneal metastasis [22]. Phase II trials to combine IP paclitaxel with other drug combinations are also under progress [23]. However, to improve outcomes further, they have been emphasizing the importance of conversion surgery where patients undergo gastrectomy following response to their combination chemotherapy [24]. Our findings revealed safety and feasibility of postoperative IP paclitaxel that begins on the day of surgery in a multi-institutional setting, and this could support their promising treatment modality, although prolonged treatment by IP paclitaxel alone cannot be recommended for patients with peritoneal disease.
There are several limitations in the current study. Gastric cancer is a heterogenous disease, and it was not possible to select patients with the risk only of peritoneal metastasis for this study although we attempted to do so through the complex eligibility criteria. Consequently, several patients had recurrences in the form of hematogenous or nodal metastasis, to which the preventive effect of IP paclitaxel was expected to have been weak. Due to a complex nature of the study and case volume expected from the small study group under strict regulations of the Advanced Medical Treatment B scheme, the planned sample size had to be kept small and the study was not designed to provide definite conclusions. Furthermore, although there were recommendations on the treatment regimens to be administered after the brief protocol treatment, actual content, duration and compliance to the subsequent chemotherapy had not been recorded in detail for analyses. However, there were no significant differences in the proportion of patients who underwent subsequent chemotherapy and the regimens selected between the two treatment arms, and it is unlikely that the post-protocol treatment had significant influence on the results of this study.
In summary, we were unable to prove the superiority of single-agent IP paclitaxel over IV paclitaxel to control advanced gastric cancer after surgery, particularly when R0 resection was not performed. If IP paclitaxel were to be explored further in the treatment of gastric cancer patients with peritoneal metastases, it should be combined with systemic chemotherapy.
References
Chang JS, Kim KH, Yoon HI, Hyung WJ, Rha SY, et al. Locoregional relapse after gastrectomy with D2 lymphadenectomy for gastric cancer. Br J Surg. 2017;104:877–84.
Burbidge S, Mahady K, Naik K. The role of CT and staging laparoscopy in the staging of gastric cancer. Clin Radiol. 2013;68:251–5.
Kobayashi M, Sakamoto J, Namikawa T, Okamoto K, Okabayashi T, Ichikawa K, et al. Pharmacokinetic study of paclitaxel in malignant ascites from advanced gastric cancer patients. World J Gastroenterol. 2006;12:1412–5.
Kodera Y. Gastric cancer with minimal peritoneal metastasis: is this a sign to give up or to treat more aggressively? Nagoya J Med Sci. 2013;75:3–10.
Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–12.
Ohashi N, Kodera Y, Nakanishi H, Yokoyama H, Fujiwara M, Koike M, et al. Efficacy of intraperitonreal chemotherapy with paclitaxel targeting peritoneal micrometastasis as revealed by GFP-tagged human gastric cancer cell lines in nude mice. Int J Oncol. 2005;27:637–44.
Hironaka S, Ueda S, Yasui H, Nishina T, Tsuda M, Tsumura T, et al. Randomized, open-label, phase III study comparing irinotecan with paclitaxel in patients with advanced gastric cancer without severe peritoneal metastasis after failure of prior combinatino chemotherapy using fluoropyrimidine plus platinum: WJSO4007 trial. J Clin Oncol. 2013;31:4438–44.
Wilke H, Muro K, Van Cutsem E, et al. Ramucirumab plus paclitaxel versus placebo plus paclitaxel in patients with previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (RAINBOW): a double-blind, randomised phase 3 trial. Lancet Oncol. 2014;15:1224–35.
Kodera Y, Ito Y, Ito S, Ohashi N, Mochizuki Y, Yamamura Y, et al. Intraperitoneal paclitaxel: a possible impact of regional delivery for prevention of peritoneal carcinomatosis in patients with gastric carcinoma. Hepatogastroenterology. 2007;54:960–3.
Markman M, Brady MF, Spirtos NM, Hanjani P, Rubin SC. Phase II trial of intraperitoneal paclitaxel in carcinoma of the ovary, tube, and peritoneum: a Gynecologic Oncology Group Study. J Clin Oncol. 1998;16:2620–4.
Armstrong DK, Bundy B, Wenzel L, Huang HQ, Baergen R, Lele S, et al. Intraperitoneal cisplatin and paclitaxel in ovarian cancer. N Engl J Med. 2006;354:34–43.
Kodera Y, Imano M, Yoshikawa T, Takahashi N, Tsuburaya A, Miyashita Y, et al. A randomized phase II trial to test the efficacy of intra-peritoneal paclitaxel for gastric cancer with high risk for the peritoneal metastasis (INPACT trial). Jpn J Clin Oncol. 2011;41:283–6.
Kodera Y, Takahashi N, Yoshikawa T, Takiguchi N, Fujitani K, Ito Y, et al. Feasibility of weekly intraperitoneal versus intravenous paclitaxel therapy delivered from the day of radical surgery for gastric cancer: a preliminary safety analysis of the INPACT study, a randomized controlled trial. Gastric Cancer. 2017;20:190–9.
Markman M, Walker JL. Intraperitoneal chemotherapy of ovarian cancer: a review, with a focus on practical aspects of treatment. J Clin Oncol. 2006;24:988–94.
Sakuramoto S, Sasako M, Yamaguchi T, Kinoshita T, Fujii M, Nashimoto A, et al. Adjuvant chemotherapy for gastric cancer with S-1, and oral fluoropyrimidine. N Engl J Med. 2007;357:1810–20.
Koizumi W, Narahara H, Hara T, Takagane A, Akiya T, Takagi M, et al. S-1 plus cisplatin versus S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): a phase III trial. Lancet Oncol. 2008;9:215–21.
Kobayashi M, Tsuburaya A, Nagata N, Miyashita Y, Oba K, Sakamoto J. A feasibility study of sequential paclitaxel and S-1 (PTX/S-1) chemotherapy as postoperative adjuvant chemotherapy for advanced gastric cancer. Gastric Cancer. 2006;9:114–9.
Tsuburaya A, Yoshida K, Kobayashi M, Yoshino S, Takahashi M, Takiguchi N, et al. Sequential paclitaxel followed by tegafur and uracil (UFT) or S-1 versus UFT or S-1 monotherapy as adjuvant chemotherapy for T4a/b gastric cancer (SAMIT): a phase 3 factorial randomised controlled trial. Lancet Oncol. 2014;15:886–93.
Association Japanese Gastric Cancer. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017;20:1–19.
Kodera Y, Ito S, Mochizuki Y, Kondo K, Koshikawa K, Suzuki N, et al. A phase II study of radical surgery followed by postoperative chemotherapy with S-1 for gastric carcinoma with free cancer cells in the peritoneal cavity (CCOG0301 study). Eur J Surg Oncol. 2009;35:1158–63.
Yang K, Liu K, Zhang WH, Lu ZH, Chen XZ, Chen XL, et al. The value of palliative gastrectomy for gastric cancer patients with intraoperativel proven peritoneal seeding. Medicine. 2015;94:e1051.
Ishigami H, Kitayama J, Kaisaki S, Hidemura A, Kato M, Otani K, et al. Phase II study of weekly intravenous and intraperitoneal paclitaxel combined with S-1 for advanced gastric cancer with peritoneal metastasis. Ann Oncol. 2010;21:67–70.
Kono K, Yong WP, Okayama H, Shabbir A, Momma T, Ohki S, et al. Intraperitoneal chemotherapy for gastric cancer with peritoneal disease: experience from Singapore and Japan. Gastric Cancer. 2017;20:122–7.
Kitayama J, Ishigami H, Yamaguchi H, Yamashita H, Emoto S, Kaisaki S, et al. Salvage gastrectomy after intravenous and intraperitoneal paclitaxel (PTX) administration with oral S-1 for peritoneal dissemination of advanced gastric cancer with malignant ascites. Ann Surg Oncol. 2014;21:539–46.
Acknowledgements
Paclitaxel was provided by Bristol-Myers K. K. for intraperitoneal administration in the study arm and testing of drug hypersensitivity. This study was supported, in part, by the nonprofit Epidemiological and Clinical Research Information Network (ECRIN).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures followed were in accordance with the ethical standards of the responsible institutional committee on human experimentation and with the Helsinki Declaration of 1964 and later versions. Informed consent to be included in the study, or the equivalent, was obtained from all patients.
Conflict of interest disclosure statement
Dr. Yoshikawa reports grants from Japanese Foundation for Multidisciplinary Treatment of Cancer during the conduct of the study; grants and personal fees from Chugai Pharmaceutical, Taiho Pharmaceutical, and Novartis Pharmaceuticals Japan; personal fees from Abbott Japan, Ono Pharmaceutical, Eli Lilly Japan, Kaken Pharmaceutical, Yakult Honsha, Nippon Kayaku, Johnson and Johnsons, Covidien Japan, Takeda Pharmaceutical, and Olympus outside the submitted work. Dr. Sakamoto received a consulting fee from Takeda Pharmaceutical and personal fees from Tsumura and Chugai Pharmaceutical Co. Ltd outside the submitted work. Dr. Morita received personal fees from Daiichi-Sankyo and Chugai Pharmaceutical outside the submitted work. Dr. Kodera reports grants and personal fees from Taiho Pharmaceutical, Chugai Phamaceutical, Sanofi, Merck Serono, Yakult Honsha, Daiichi Sankyo, Otsuka Pharmaceutical Factory, Takeda Pharmaceutical, Kaken Pharmaceutical, Ono Pharmaceutical, Johnson & Johnson, and Eli Lilly Japan; and grants from Pfizer Japan, EA Pharma, Covidien Japan, Shionogi, Bristol Myers Squib, Japan Blood Products Organization, AbbVie GK, Eizai, Abbott Japan, CSL Behring, Tsumura, Nippon Kayaku, Novartis Pharmaceuticals Japan, KCI, Toyama Chemical, and Maruho; and personal fees from MSD, Olympus, and Asahi Kasei Pharma outside the submitted work.
Rights and permissions
About this article
Cite this article
Takahashi, N., Kanda, M., Yoshikawa, T. et al. A randomized phase II multicenter trial to explore efficacy of weekly intraperitoneal in comparison with intravenous paclitaxel administered immediately after gastrectomy to the patients with high risk of peritoneal recurrence: final results of the INPACT trial. Gastric Cancer 21, 1014–1023 (2018). https://doi.org/10.1007/s10120-018-0817-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-018-0817-y