Abstract
Objective
Postoperative chemotherapy with S-1 or capecitabine plus oxaliplatin is a standard treatment for resectable gastric cancer (GC). However, survival outcomes of stage IIIB–IV (M0) GC cases are still poor. We investigated the efficacy and safety of docetaxel, capecitabine, and cisplatin (DXP) in patients with stage IIIB–IV GC.
Methods
This was a single-arm phase 2 study that included patients with stage IIIB–IV GC who underwent D2 gastrectomy. Patients received six cycles of docetaxel [60 mg/m2 on day 1 (D1)], capecitabine (1,875 mg/m2/day on D1–14), and cisplatin (60 mg/m2 on D1) every 3 weeks. The primary end-point was recurrence-free survival (RFS).
Results
A total of 46 GC patients between January 2007 and August 2008 were included. After a median follow-up of 56.1 months (range 52.2–64.1), the median RFS and overall survival (OS) were 26.9 months (95 % CI 7.5–46.4) and 43.9 months (95 % CI 29.2–58.7), respectively. The 5-year RFS and OS rates were 39.1 and 41.3 %, respectively. The most common grade 3/4 toxicities were neutropenia (40 %), anorexia (22 %), and febrile neutropenia (15 %).
Conclusions
Adjuvant DXP is feasible and effective for patients with stage IIIB–IV GC. A phase 3 study comparing triplet and doublet regimens for these patients is ongoing.
Similar content being viewed by others
Introduction
Gastric cancer (GC) is a major cause of cancer deaths worldwide [1, 2]. Although surgical resection is the mainstay of treatment for localized GC, a significant proportion of GC patients experience a recurrence even after curative surgery [3]. To improve the survival outcomes of patients with localized GC, various adjuvant treatment strategies have been investigated. With its efficacy demonstrated in pivotal trials, adjuvant treatment is now accepted as the standard of care in patients with resectable GC, although there are still differences in the specific strategies utilized in different geographic regions [4]. Perioperative chemotherapy using epirubicin, cisplatin, and 5-fluorouracil (ECF) as well as postoperative chemoradiation are the standard adjuvant therapies in Europe and North America, respectively. In East Asia, where extended lymph node (D2) resection is performed in most patients, postoperative chemotherapy with S-1 for 1 year or combined capecitabine–oxaliplatin (XELOX) for 6 months has been considered the standard of care based on the results of the ACTS-GC and CLASSIC trials [5–8].
Although the survival outcomes of patients with localized GC have improved with adjuvant treatment, the prognosis for patients with more advanced cancers is still poor. With postoperative chemotherapy, the 5-year recurrence-free survival (RFS) rates of patients with stage IIIB–IV tumors [according to the American Joint Committee on Cancer (AJCC) staging, 6th edition] in the ACTS-GC and CLASSIC trials ranged from 38 to 52 %, whereas the rates were 79–80 % for stage II and 58–61 % for stage IIIA cancers [9, 10]. Therefore, improvements in the efficacy of standard regimens are necessary, particularly for GC patients with tumors at relatively advanced stages.
Intensifying chemotherapy by adding other active agents may be effective in improving the outcomes of patients with more advanced staged tumors. Docetaxel is a good candidate agent for this strategy because this drug has demonstrated efficacy in patients with metastatic or recurrent GC, either as a single agent or as a combination chemotherapy [11–13]. Furthermore, the addition of docetaxel to fluorouracil plus cisplatin (DCF) demonstrated improved efficacy compared to a doublet regimen in a randomized phase 3 trial (V325) for chemotherapy-naïve patients with metastatic or recurrent GC [12]. In that trial, triplet chemotherapy including docetaxel significantly improved time to progression (5.6 vs. 3.7 months), overall survival (OS; 9.2 vs. 8.6 months), and response rate (37 vs. 25 %). Despite the promising efficacy of the DCF regimen, substantial toxicities (grade 3/4 toxicities and febrile neutropenia were reported in 82 and 29 % of patients, respectively) that accompanied the addition of docetaxel proved to be obstacles to the wide implementation of combination in daily clinical practice.
Many modified DCF regimens that aim to reduce the toxicity while retaining the efficacy of DCF have been investigated in patients with metastatic or recurrent GC [14]. We also modified DCF by substituting capecitabine for intravenous fluorouracil and adjusted the doses of docetaxel and cisplatin [15]. This triplet regimen (docetaxel–capecitabine–cisplatin, DXP) showed favorable efficacy as a first-line chemotherapy in a previous phase 1/2 study for unresectable or metastatic GC with a median OS of 14.4 months, a progression-free survival (PFS) of 7.6 months, and pathologic complete response in 10 % of patients [15]. In another phase 2 trial of DXP for locally advanced, unresectable GC, curative R0 resection was achieved in 63 % of patients after neoadjuvant DXP, and a long-term disease-free interval was noted even in patients with paraaortic lymph node-limited metastasis, despite the fact that this is regarded as a distant metastasis [16]. In addition, DXP displayed a favorable safety profile compared to DCF [15, 16]. Of note, 10 % (4/40) and 4 % (2/48) of patients experienced febrile neutropenia in a phase I/II study and a neoadjuvant study, respectively, which are more favorable than the 29 % of patients who experienced febrile neutropenia while on the DCF regimen in the V325 trial.
To investigate DXP in the adjuvant setting, we conducted a phase II trial to evaluate the efficacy and safety of adjuvant DXP in patients with stage IIIB–IV [without distant metastasis (M0)] GC.
Materials and methods
Study design and patients
This study was an open-label, single-arm, phase 2 trial. Eligibility criteria included histologically documented adenocarcinoma of the stomach or esophagogastric junction; curative D2 resection; stage IIIB or IV without distant metastasis (pT3N2, pT4N1-2M0 or pTanyN3M0) according to the AJCC staging system, 6thedition; an age of between 18 and 70 years; an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1; adequate bone marrow function (absolute neutrophil count [17] >1,500/µL, hemoglobin >9.0 g/dL, and platelets >100,000/µL); adequate renal function (serum creatinine <1.5 mg/dL); adequate liver function [total serum bilirubin less than the upper normal limit (UNL)], aspartate aminotransferase and alanine aminotransferase <2.5 × UNL, alkaline phosphatase <5 × UNL); and no prior chemotherapy or radiotherapy.
The study protocol was approved by the Institutional Review Board of the Asan Medical Center, Seoul, Korea, and was conducted in accordance with the principles of the Declaration of Helsinki and the International Conference on Harmonization good clinical practice guidelines. All patients provided written informed consent prior to study entry (ClinicalTrials.gov identifier: NCT00976976).
Study treatment
DXP consisted of the following every 21 days: intravenous docetaxel (60 mg/m2) on day 1; oral capecitabine (1,875 mg/m2), divided into two daily doses, on days 1–14; and intravenous cisplatin (60 mg/m2) on day 1 [15]. Chemotherapy was administered within 3 weeks after operation. Prophylactic use of granulocyte colony-stimulating factor was not allowed. Study treatment was initiated at least 3 weeks after surgery, and patients received a total of six cycles of study chemotherapy unless there was disease recurrence or unacceptable toxicity. Before starting each cycle, an ANC of ≥1,500/µL and platelet counts of ≥100,000/µL were required.
Doses of chemotherapeutic agents were modified according to the protocol. Briefly, capecitabine and docetaxel were simultaneously reduced by 25 % with febrile neutropenia, grade 4 neutropenia for >7 days, or grade 4 thrombocytopenia. Dose reduction or interruption was not allowed for anemia if it could be successfully managed by transfusions. Docetaxel, capecitabine, and cisplatin were interrupted for grade 2–3 nonhematological toxicities (except for alopecia and nail toxicity) until the toxicities resolved to below grade 1. A delay in the study treatment of up to 3 weeks was not allowed. Study medications were discontinued when any grade 4 nonhematological toxicities occurred.
Assessment
Baseline assessments included medical history, physical exams, electrocardiography, chest X-ray, computed tomography (CT) scan of the abdomen and pelvis, complete blood counts, serum electrolytes and chemistry, and urine analysis. During the study treatment, adverse events and laboratory profiles were assessed every 3 weeks. After completion of chemotherapy, clinical assessments were performed every 3 months until 2 years after surgery, and then every 6 months for an additional 3 years. To detect recurrences, a chest X-ray and CT scans were performed every 6 months, and an esophagogastroduodenoscopy was undertaken every year for the first 5 years after surgery. Additional imaging studies were performed whenever recurrence was clinically suspected. If imaging findings were suggestive of recurrent disease but not conclusive, rigorous serial follow-up examinations were performed to verify the recurrence, and the date of the first recognition of image findings suggestive of recurrence was defined as the date of recurrence. Adverse events were graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events, version 3.0.
Statistical analysis
The primary endpoint of the present study was RFS, and secondary endpoints were the OS and safety profiles. On the basis of the results of our previous phase 3 trial of adjuvant chemotherapy, which included 158 patients with stage IIIB–IV (M0) gastric cancer and demonstrated a 3-year RFS of 29.4 % [18], the 3-year RFS rate in patients with stage IIIB–IV tumors receiving adjuvant chemotherapy with a doublet of fluoropyrimidine and platinum was assumed to be 29 % (P0), and we hypothesized that this could be improved to 45 % (P1) with DXP. With an alpha of 0.10 and a power of 80 %, 43 patients were required for this study according to the Simon single-stage phase 2 design. Considering a 10 % rate of loss to follow-up, the target enrollment was 46 patients.
RFS was defined as the time from the date of surgery to documented disease recurrence or death. OS was defined as the interval between surgery and death of any cause. Kaplan–Meier curves were used to estimate survival and compared using the log-rank test. Efficacy outcome was analyzed on an intention-to-treat basis. The ratio of the actual dose taken to the prescribed dose was used to calculate relative dose intensity. A safety analysis was conducted in patients who received at least one dose of chemotherapy. Statistical analyses were performed using SPSS statistical software (version 18.0, IBM SPSS Inc., Chicago, IL, USA).
Results
A total of 46 patients with a curatively resected stage IIIB–IV GC between January 2007 and August 2008 were enrolled in this study. Baseline patient characteristics are summarized in Table 1. Fourteen (30 %) patients were pathologically graded as stage IIIB and 32 (70 %) patients as stage IV according to the AJCC, 6th edition. All patients underwent D2 lymph node dissection, and none had a distant metastasis at the time of study enrollment. The cutoff date for analysis was November 28, 2012.
With a median follow-up of 56.1 months (range 52.2–64.1 months) in the surviving patients, 28 (61 %) patients experienced a recurrence and 27 (59 %) patients died. While locoregional relapse was observed in two (7 %) patients, most patients (n = 26, 93 %) with recurrence showed a distant metastasis (Table 2). The peritoneum was the most common site of relapse (n = 12, 43 %), followed by the lymph nodes (n = 10, 36 %). The 3-year RFS and OS rates were 48 % (95 % CI 36–60 %) and 59 % (95 % CI 46–72 %), respectively, and 5-year RFS and OS rates were 39 % (95 % CI 28–50 %) and 41 % (95 % CI 30–52 %), respectively. The median RFS was 26.9 months (95 % CI 7.5–46.4 months) and the median OS was 43.9 months (95 % CI 29.2–58.7 months; Fig. 1). Based on the pathologic stage, the 5-year RFS and OS rates were 50 % (95 % CI 24–76 %) and 57 % (95 % CI 31–83 %), respectively, in patients with stage IIIB, and 34 % (95 % CI 18–51 %) and 34 % (95 % CI 18–51 %), respectively, in patients with stage IV (M0). The differences in the survival outcomes of patients with stage IIIB and IV tumors were not statistically significant (RFS, p = 0.32; and OS, p = 0.14).
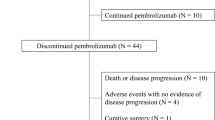
The planned six cycles of adjuvant DXP treatment were completed in 40 (87 %) patients. Study treatment was discontinued in 6 (13 %) patients; 3 (7 %) due to the patient’s wishes, 1 (2 %) due to disease recurrence, 1 (2 %) due to intolerable grade 3 anorexia and stomatitis, and 1 (2 %) due to transverse colon perforation, which was not considered treatment-related since it was not accompanied by any other treatment-related changes in the intestine. Doses of docetaxel, capecitabine, and cisplatin were reduced in 18 (39 %), 20 (43 %), and 38 (83 %) patients, respectively. Study treatment was delayed in 24 (52 %) patients. The median relative dose intensities for docetaxel, capecitabine, and cisplatin were 77, 66, and 85 %, respectively (Fig. 2).
A safety analysis was available for all patients. The adverse events associated with DXP are summarized in Table 3. There was no treatment-related death in our cohort. The most common adverse events of any grade were fatigue (100 %), alopecia (100 %), anorexia (99 %), and anemia (89 %). Grade 3/4 neutropenia occurred in 18 (40 %) patients, and febrile neutropenia developed in 7 (15 %) patients. Grade 3/4 thrombocytopenia was observed in 2 (4 %) patients. Among the nonhematological toxicities, grade 3/4 anorexia, fatigue, and nausea were the most frequent, as reported in 10 (22 %), 5 (11 %), and 5 (11 %) patients, respectively. Among 31 patients whose doses of chemotherapeutic agents were modified, grade 4 neutropenia (n = 18) was the most frequent cause of dose modification, followed by grade 3 anorexia (n = 3), grade 3 asthenia (n = 3), grade 3 febrile neutropenia (n = 2), grade 3 nausea (n = 2), grade 3 diarrhea (n = 2), and grade 4 thrombocytopenia (n = 1).
Discussion
The results of our present phase 2 study show that a DXP triplet regimen is feasible in the adjuvant setting. Furthermore, considering that 70 % of our study population were graded as stage IV (M0) pathologically, our efficacy outcomes appear to be promising for patients with resectable but more advanced disease. In addition, considering the poor prognosis of this patient population, further investigation of this strategy is warranted in a future randomized phase 3 trial.
Although differences in the therapeutic approaches for patients with resectable GC still exist among different geographic regions, adjuvant treatment has been accepted worldwide as the standard of care with proven survival benefits [4]. In East Asia, where D2 resection is the standard surgery for resectable GC, postoperative oral fluoropyrimidine-based chemotherapy has been established as the standard based on the results of the ACTS-GC and CLASSIC trials [7, 8]. Because the pathologic stage is the most important prognostic factor for gastric cancer, patients with stage IIIB–IV (M0) tumors show poor survival outcomes. In those two earlier studies, however, stage IIIB–IV patients comprised only 13–18 % of the overall study population. Moreover, no stage IV (M0) patient was enrolled for treatment with XELOX in the CLASSIC trial, and only 8 % of patients assigned to the S-1 arm were stage IV (M0) in the ACTS-GC trial. Considering that differences in the clinical features may exist between early and advanced gastric cancer, even though they are resectable, these data suggest that current standard regimens might not be optimal for patients with stage IIIB–IV (M0) gastric cancer.
Given that the outcomes of patients with axillary node-positive breast cancer have been improved with more intensive adjuvant chemotherapy by adding taxane [19], a similar adjuvant strategy might also be effective for the management of patients with curatively resected but more advanced gastric cancer. Based on the promising efficacy data and tolerable safety profile demonstrated in our previous phase 2 trials, which investigated DXP in the preoperative and first-line palliative settings [15, 16], we implemented DXP in the postoperative adjuvant setting. In our current study of this intensive triplet regimen, 5-year RFS and OS rates were 39 and 41 %, respectively, in patients with resected stage IIIB–IV (M0) gastric cancer. The median RFS and OS were 26.9 and 43.9 months, respectively. In previously reported long-term follow-up analyses of the ACTS-GC and CLASSIC trials, 5-year RFS rates were 36 % in stage IIIB and 29 % in stage IV with S-1, and 52 % in stage IIIB with XELOX, and the 5-year OS rates were 50 % in stage IIIB and 45 % in stage IV with S-1, and 66 % in stage IIIB with XELOX [9, 10]. Although cross-trial comparison with subgroups of other trials should be done cautiously, our present results appear to be promising for these potentially curable patients considering that 70 % of our cases had stage IV (M0) tumors. In addition, despite the fact that the 5-year survival outcomes of stage IIIB patients in our current study series (50 and 57 %) appear similar to those in the CLASSIC trial in which patients received XELOX [10], such a comparison may be premature because only 14 patients with stage IIIB were enrolled in our current cohort.
The use of more intensive chemotherapy to improve the efficacy of existing regimens for adjuvant chemotherapy has already been investigated in previous randomized phase 3 trials for overall stages of gastric cancer patients, but all of those studies failed to demonstrate a survival benefit for this strategy [17, 18, 20]. The AMC 0201 trial in Korea compared mitomycin, cisplatin, and 12 months of oral doxifluridine (MFP) with mitomycin plus 3 months of oral doxifluridine (Mf) in patients with D2-resected stage II–IV (M0) gastric cancer [18]. There was no difference between the two groups in RFS (5-year RFS 61.1 % in Mf and 57.9 % in MFP; hazard ratio (HR) 1.10 (95 % CI 0.89–1.35; p = 0.39) and OS (5-year OS 66.5 % in Mf and 65.0 % in MFP; HR 1.1 (95 % CI 0.89–1.39; p = 0.33) in patients with stage II–IV (M0). In stage IIIB–IV (M0), MFP could not show a significant difference in RFS (5-year RFS 60.9 % in Mf and 59.0 % in MFP; HR 1.074 (95 % CI 0.870–1.326); p = 0.505) as well as in OS (5-year OS 66.6 % in Mf and 64.1 % in MFP; HR 1.133 (95 % CI 0.904–1.419); p = 0.278). In the North American CALGB 80101 trial, the standard 5-fluorouracil/leucovorin regimen was intensified by adding epirubicin and cisplatin (ECF) as a postoperative chemoradiotherapy for patients with resected gastric cancer (p = 0.99 for RFS and p = 0.80 for OS) [20]. In the ITACA-S trial from Italy, four cycles of FOLFIRI (5-fluorouracil, leucovorin, and irinotecan) followed by three cycles of docetaxel and cisplatin were tested for comparison with 5-fluorouracil/leucovorin (p = 0.97 for RFS and p = 0.87 for OS) [17]. These might represent evidence against the potential role of intensive chemotherapy in patients with curatively resected gastric cancer. However, in more advanced disease, there is a greater chance of residual microscopic disease associated with increased recurrence even after grossly radical excision of tumors. Although subgroup analyses in these studies could not show a survival benefit for intensified chemotherapy in patients with stage IIIB–IV tumors, it is noteworthy that these studies were not sufficiently powered to determine survival differences between these subgroups, and that only small numbers of stage IIIB–IV patients were included.
The lack of reliable previous data for chemotherapy against stage IIIB–IV gastric cancer and the promising outcomes obtained with DXP in our current study argue that further investigation of an intensive triplet regimen is strongly warranted in this patient population. Based on this consideration, a randomized phase III trial (TRIUMPH) of adjuvant chemotherapy for patients with D2-resected stage IIIB–IV (M0) gastric cancer is now ongoing to compare the efficacy and safety of docetaxel, capecitabine, and oxaliplatin (DXO) with those of XELOX, the current standard regimen in East Asia (NCT01935778). As oxaliplatin has replaced cisplatin in the first-line treatment setting for unresectable or metastatic disease based on the results of REAL-2, and the oxaliplatin–capecitabine doublet is now regarded as one of the standard adjuvant treatments [21], we used an oxaliplatin-containing triplet DXO regimen for this phase III trial instead of DXP.
The adverse events associated with DXP were comparable with those noted in our previous phase 2 trials [15, 16], and there was no new toxicity of DXP observed in this study. Compliance with adjuvant chemotherapy is generally well known to be poor following a gastrectomy, but this triplet regimen was found to be well tolerated, although toxicities seem to be increased compared to a single agent or doublet, as expected. Among grade 3 or 4 events, neutropenia, anorexia, fatigue, and nausea represented the most common toxicities associated with adjuvant DXP. Although the incidence of severe neutropenia was previously reported to be higher than that with XELOX in the CLASSIC trial [8], there was no treatment-related death, and most toxicities were manageable with prompt dose modifications. In particular, 39 % (18/46) and 15 % (7/46) of patients experienced grade 3 or 4 neutropenia and febrile neutropenia in this study, which is more favorable than the corresponding values, 82 % (181/221) and 29 % (63/221), noted for patients on the DCF regimen in the V325 trial.
In our current study, the 6th edition of the AJCC staging system was used to stratify patients with stage IIIB–IV, although the staging system was subsequently revised to the 7th edition. We chose to use the 6th edition of the AJCC staging system because our study was planned before the publication of the 7th edition. In addition, because previous pivotal trials for current standard adjuvant chemotherapy were conducted based on the AJCC 6th edition, we believed that the efficacy outcomes in our current analyses would be more readily comparable with those of previous trials.
In conclusion, adjuvant DXP is feasible and effective and warrants a phase 3 trial for patients with completely resected stage IIIB–IV (M0) gastric cancer. This indicates that there is still room to improve the survival outcomes of patients with localized but more advanced disease. An ongoing phase 3 trial comparing an adjuvant triplet regimen with a doublet regimen will likely address the role of intensive chemotherapy in this patient population.
References
Jung KW, Won YJ, Kong HJ, Oh CM, Lee DH, Lee JS. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2011. Cancer Res Treat. 2014;46(2):109–23.
Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014;64(1):9–29.
D’Angelica M, Gonen M, Brennan MF, Turnbull AD, Bains M, Karpeh MS. Patterns of initial recurrence in completely resected gastric adenocarcinoma. Ann Surg. 2004;240(5):808–16.
Yoo C, Kang Y-K. An update of adjuvant treatments for localized advanced gastric cancer. Clin Investig. 2012;2(11):1101–8.
Macdonald JS, Smalley SR, Benedetti J, Hundahl SA, Estes NC, Stemmermann GN, et al. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N Engl J Med. 2001;345(10):725–30.
Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson M, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355(1):11–20.
Sakuramoto S, Sasako M, Yamaguchi T, Kinoshita T, Fujii M, Nashimoto A, et al. Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med. 2007;357(18):1810–20.
Bang YJ, Kim YW, Yang HK, Chung HC, Park YK, Lee KH, et al. Adjuvant capecitabine and oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): a phase 3 open-label, randomised controlled trial. Lancet. 2012;379(9813):315–21.
Sasako M, Sakuramoto S, Katai H, Kinoshita T, Furukawa H, Yamaguchi T, et al. Five-year outcomes of a randomized phase III trial comparing adjuvant chemotherapy with S-1 versus surgery alone in stage II or III gastric cancer. J Clin Oncol. 2011;29(33):4387–93.
Noh SH, Park SR, Yang HK, Chung HC, Chung IJ, Kim SW, et al. Adjuvant capecitabine plus oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): 5-year follow-up of an open-label, randomised phase 3 trial. Lancet Oncol. 2014;15(12):1389–96.
Bang YJ, Kang WK, Kang YK, Kim HC, Jacques C, Zuber E, et al. Docetaxel 75 mg/m(2) is active and well tolerated in patients with metastatic or recurrent gastric cancer: a phase II trial. Jpn J Clin Oncol. 2002;32(7):248–54.
Van Cutsem E, Moiseyenko VM, Tjulandin S, Majlis A, Constenla M, Boni C, et al. Phase III study of docetaxel and cisplatin plus fluorouracil compared with cisplatin and fluorouracil as first-line therapy for advanced gastric cancer: a report of the V325 Study Group. J Clin Oncol. 2006;24(31):4991–7.
Lee JL, Ryu MH, Chang HM, Kim TW, Yook JH, Oh ST, et al. A phase II study of docetaxel as salvage chemotherapy in advanced gastric cancer after failure of fluoropyrimidine and platinum combination chemotherapy. Cancer Chemother Pharmacol. 2008;61(4):631–7.
Ajani JA. Optimizing docetaxel chemotherapy in patients with cancer of the gastric and gastroesophageal junction: evolution of the docetaxel, cisplatin, and 5-fluorouracil regimen. Cancer. 2008;113(5):945–55.
Kang YK, Ryu MH, Yoo C, Chang HM, Yook JH, Oh ST, et al. Phase I/II study of a combination of docetaxel, capecitabine, and cisplatin (DXP) as first-line chemotherapy in patients with advanced gastric cancer. Cancer Chemother Pharmacol. 2011;67(6):1435–43.
Sym SJ, Chang HM, Ryu MH, Lee JL, Kim TW, Yook JH, et al. Neoadjuvant docetaxel, capecitabine and cisplatin (DXP) in patients with unresectable locally advanced or metastatic gastric cancer. Ann Surg Oncol. 2010;17(4):1024–32.
Bajetta E, Floriani I, Di Bartolomeo M, Labianca R, Falcone A, Di Costanzo F, et al. Randomized trial on adjuvant treatment with FOLFIRI followed by docetaxel and cisplatin versus 5-fluorouracil and folinic acid for radically resected gastric cancer. Ann Oncol. 2014;25(7):1373–8.
Kang YK, Chang HM, Yook JH, Ryu MH, Park I, Min YJ, et al. Adjuvant chemotherapy for gastric cancer: a randomised phase 3 trial of mitomycin-C plus either short-term doxifluridine or long-term doxifluridine plus cisplatin after curative D2 gastrectomy (AMC0201). Br J Cancer. 2013;108(6):1245–51.
Mamounas EP, Bryant J, Lembersky B, Fehrenbacher L, Sedlacek SM, Fisher B, et al. Paclitaxel after doxorubicin plus cyclophosphamide as adjuvant chemotherapy for node-positive breast cancer: results from NSABP B-28. J Clin Oncol. 2005;23(16):3686–96.
Fuchs CS, Tepper JE, Niedzwiecki D, Hollis D, Mamon HJ, Swanson R, Haller DG, Dragovich T, Alberts SR, Bjarnason GA, Willett CG, Enzinger PC, Goldberg RM, Venook AP, Mayer RJ. Postoperative adjuvant chemoradiation for gastric or gastroesophageal junction (GEJ) adenocarcinoma using epirubicin, cisplatin, and infusional (CI) 5-FU (ECF) before and after CI 5-FU and radiotherapy (CRT) compared with bolus 5-FU/LV before and after CRT: intergroup trial CALGB 80101. J Clin Oncol. 2011;29:4003.
Cunningham D, Starling N, Rao S, Iveson T, Nicolson M, Coxon F, Middleton G, Daniel F, Oates J, Norman AR, for the Upper Gastrointestinal Clinical Studies Group of the National Cancer Research Institute of the United Kingdom. Capecitabine and oxaliplatin for advanced esophagogastric cancer. N Engl J Med. 2008;2008(358):36–46.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yoon-Koo Kang received honoraria from Roche, Taiho, and Sanofi and research grants from Roche and Sanofi. The authors have no other potential conflicts of interest to declare.
Ethical standards
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation at the Asan Medical Center, Korea, and with the Helsinki Declaration of 1964 and later versions. Informed consent or a substitute for it was obtained from all patients before they were included in the study.
Additional information
Shinkyo Yoon and Changhoon Yoo contributed equally to this work.
Rights and permissions
About this article
Cite this article
Yoon, S., Yoo, C., Ryu, MH. et al. Phase 2 study of adjuvant chemotherapy with docetaxel, capecitabine, and cisplatin in patients with curatively resected stage IIIB–IV gastric cancer. Gastric Cancer 20, 182–189 (2017). https://doi.org/10.1007/s10120-015-0580-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-015-0580-2