Abstract
Background
Preoperative chemotherapy is a promising strategy for downstaging advanced gastric cancer before radical resection, although severe adverse events can occur and clinical outcomes are often unsatisfactory. To identify predictive biomarkers of drug sensitivity, we used a well-designed functional apoptosis assay and assessed the correlations between chemosensitivity and clinical outcomes.
Methods
Drug sensitivity to docetaxel, cisplatin, and 5-fluorouracil was examined in 11 gastric cancer cell lines. BCL2-homology domain 3 (BH3) profiling was performed and assessed for correlations with drug sensitivity. Immunohistochemical staining of clinical gastric cancer specimens was performed before preoperative chemotherapy, and correlations with histopathological responses and clinical outcomes were assessed.
Results
BIM (BCL2L11)-BH3 profiling results correlated with docetaxel sensitivity and BAK protein expression, whose knockdown caused docetaxel resistance. The BAK expression indexes of 69 gastric cancer specimens before preoperative chemotherapy (including docetaxel treatment) were determined by multiplying numerical values describing the degrees of BAK positivity and staining intensity observed. Patients whose specimens showed good chemotherapeutic histopathological responses had higher BAK indexes than those with poor responses. Patients with BAK index values ≥3 showed improved progression-free survival (HR, 2.664; 95 % CI, 1.352–5.248; P = 0.005) and overall survival (HR, 3.390; 95 % CI, 1.549–7.422; P = 0.002).
Conclusions
BH3 profiling clearly showed that BIM expression, which depends on BAK expression, correlated with docetaxel sensitivity. BAK expression in gastric cancer is thus predictive of chemotherapeutic responses to docetaxel and clinical prognosis in patients treated with preoperative chemotherapy.
Similar content being viewed by others
Introduction
Gastric cancer is the fourth most common cancer in the world and the second most common cancer, with the third highest mortality rate, in eastern Asia [1]. The prognosis of advanced gastric cancer remains poor in Japan, with the overall 5-year survival rate being less than 50 %, or only 5 % in cases involving distant metastasis [2]. To improve the long-term prognosis of patients with gastric cancer, preoperative chemotherapy may increase the probability of curative resection (R0) by eradicating a distant metastasis. Combination therapy with the cytotoxic drugs 5-fluorouracil (5-FU), cisplatin (CDDP), irinotecan, and epirubicin was previously used [3–5], which showed good responses and higher R0 rates in patients with resectable advanced gastric cancer. However, severe adverse events such as treatment-related deaths have been reported [4], and the clinical benefits in patients with unresectable metastatic gastric cancer remain to be determined.
Docetaxel, which belongs to the taxane family of compounds, causes antitumor activity by promoting the assembly of microtubules and preventing their depolymerization, resulting in cell apoptosis [6, 7]. A triple regimen of docetaxel, CDDP, and 5-FU was shown to improve survival compared with a double regimen of CDDP and 5-FU in patients with advanced gastric cancer [8, 9]. The triple regimen also caused increased adverse events [8]; therefore, both the efficacy and tolerability of combination chemotherapy are critical for clinical success.
S-1 was developed as an orally activated prodrug of 5-FU that contains tegafur, gimeracil, and potassium oxonate and which shows enhanced treatment efficacy and reduced gastrointestinal toxicity [10]. We previously reported the high efficacy and safety of a novel triplet regimen containing docetaxel, CDDP, and S-1 for unresectable metastatic and locally advanced gastric cancer [11, 12]. The tumor response rate was 74.4 %, and the proportions of curative resections and pathological responses in patients receiving this triplet chemotherapy were as great as 90.7 % and 65.9 %, respectively. No treatment-related deaths occurred, and the regimen was well tolerated; however, we did observe the occurrence of high-grade hematological toxicity, or non-hematological toxicity such as nausea, diarrhea, and stomatitis. The histopathological analysis of resected specimens from patients treated with preoperative chemotherapy has revealed valuable biomarkers for assessing survival benefits after surgery [13, 14]. Predicting responses to cytotoxic drugs before initiating preoperative chemotherapy can potentially spare patients who are unlikely to respond to such treatment from the associated adverse effects. A high curative resection rate associated with our novel triplet regimen enabled us to assess histopathological responses in resected specimens with minimal influence.
The BCL-2 family proteins are known to control the apoptosis and classified into pro-apoptotic and anti-apoptotic members [15]. Because of the complexity of their interaction, it is hard to determine on which BCL-2 family protein the living cancer cells would functionally depend. Recently, a new functional assay, BCL2-homology domain 3 (BH3) profiling, was reported, and this profiling could predict a single drug sensitivity in patients with acute myelogenous leukemia and multiple myeloma who were treated with multiple drugs [16, 17].
Here, we explored biomarkers for predicting sensitivity to docetaxel, CDDP, and 5-FU in gastric cancer. Drug cytotoxicity and BH3 profiling were examined in gastric cancer cells, which enabled the identification of candidate biomarkers for drug sensitivity. Clinical gastric cancer specimens obtained before preoperative chemotherapy were tested by immunostaining and assessed for correlations with histopathological responses and clinical outcomes.
Patients and methods
Cell lines
The gastric cancer cell lines MKN74, MKN45, MKN1, NUGC-2, NUGC-3, NUGC-4, and KATO-III were purchased from the JCRB cell bank (Ibaraki, Osaka, Japan). The JR-St and HSC39 cell lines were purchased from Takara Bio (Otsu, Shiga, Japan). The NCI-N87 cell line was obtained from ATCC (Manassas, VA, USA). The TMK1 cell line was initially established by Ochiai et al. [18]. All cell lines were cultured at 37 °C in a humidified 5 % CO2 incubator in RPMI (Sigma, St. Louis, MO, USA) medium supplemented with 10 % fetal bovine serum (FBS; Sigma), 10 mM l-glutamine (Sigma), 100 U/ml penicillin, and 100 µg/ml streptomycin (Sigma), except for NUGC-2 cells, which were grown in RPMI medium supplemented with 15 % FBS.
Drug sensitivity
First, 10,000 gastric cancer cells were treated for 72 h with either docetaxel (Sigma), 5-FU (Sigma), or CDDP (LKT Laboratories, St. Paul, MN, USA) at the indicated concentrations in 96-well plates (Nunc, Roskilde, Denmark). Subsequently, cell proliferation was determined using the Premix WST-1 Cell Proliferation Assay (Takara Bio) and an Infinite M100 PRO microplate reader (Tecan Japan, Kawasaki, Kanagawa, Japan). The resulting absorbances were converted to percent survival rates by comparisons with untreated cells (set as 100 % survival). The half-maximal inhibitory concentration (IC50) was defined as the drug concentration resulting in 50 % cell survival relative to that of untreated cells. Triplicate wells were treated with various drug concentrations, and average IC50 values were determined.
Apoptosis assays
Gastric cancer cells (500,000) were then allowed to adhere to 75-cm2 plastic tissue culture flasks for 24 h, after which they were treated with either 12 nM docetaxel, 12 μM CDDP, or 20 μM 5-FU for 72 h. Cells were then harvested and washed, followed by staining with a phycoerythrin-conjugated Annexin V antibody and 7-AAD (BD Pharmingen, San Jose, CA, USA). Apoptotic cells were analyzed on a BD FACSCanto II flow cytometer (BD Biosciences, San Jose, CA, USA) with FACSDiva software (BD Biosciences).
Western blotting
Western blotting was performed as previously described [19]. Briefly, separated proteins were transferred to nylon membranes and blotted with specific antibodies to detect BCL-2 (Cell Signaling Technology, Danvers, MA, USA, #2870), BCL-XL (Cell Signaling Technology, #2764), BCL-W (Cell Signaling Technology, #2724), MCL-1 (Cell Signaling Technology, #5453), BIM (Cell Signaling Technology, #2933), BAK (Cell Signaling Technology, #12105), BAX (Cell Signaling Technology, #5023), and actin (Santa Cruz Biotechnology, Santa Cruz, CA, USA, #sc1615). After incubation with horseradish peroxidase-conjugated donkey anti-rabbit IgG (GE Healthcare, Pittsburgh, PA, USA), the membrane was stained by the ECL Prime Western Blotting Detection Reagent (GE Healthcare). Finally, bands were imaged by exposing BIOMAX XAR film (Carestream Health, Rochester, NY, USA) to membranes and developing the film on a Kodak X-OMAT 1000 Processor (Amersham, Piscataway, NJ USA). Protein expression levels were quantified using ImageJ software (NIH), and relative expression levels were calculated from the expression ratio of each protein to actin.
BH3 profiling
Eight BH3 peptides (including one control peptide derived from the PUMA peptide, but with two amino acid substitutions) were obtained as HPLC-purified products from Sigma-Aldrich (Supplementary Table 1). All peptides were dissolved in dimethyl sulfoxide (DMSO; Sigma-Aldrich) as 1 mM stock solutions and stored at −80 °C. BH3 profiling was performed as described previously [20]. Briefly, 200,000 gastric cancer cells were suspended in T-EB buffer [300 mM Trehalose, 10 mM HEPES–KOH (pH 7.7), 80 mM KCl, 1 mM EDTA, 1 mM EGTA, 0.1 % bovine serum albumin (BSA), and 5 mM succinate; all from Sigma] containing 0.001 % digitonin (Sigma) and 20 μg/ml oligomycin (Sigma). The cells were then incubated with BH3 peptide at a final concentration of 10 μM. After staining cells with 25 nM tetramethylrhodamine ethyl ester (Invitrogen, Carlsbad, CA, USA), fluorescence intensities were analyzed on a BD FACSCanto II with FACSDiva software. The percentage of relative mitochondrial depolarization was calculated using the following equation:
where DMSO(fv) is the mean fluorescence value with the negative control, X(fv) indicates the mean fluorescence value with the tested BH3 peptide, and FCCP(fv) indicates the mean fluorescence value with the positive control.
Inhibition of BAK expression by small-interfering RNA (siRNA) transfections
One million gastric cancer cells in six-well plates were transfected either with siRNAs targeting human BAK (Dharmacon, Lafayette, CO, USA; D-003305-01, D-003305-04) or a non-targeting siRNA (Dharmacon; D-001210-03-05) using RNAi Max reagent (Invitrogen), according to the manufacturer’s instructions. The transfected cells were analyzed both by BH3 profiling and apoptosis assays with docetaxel, as described in the earlier “Apoptosis assays” and “BH3 profiling” sections.
Patients and treatment
The examined patients were registered in a clinical study that was part of an open-label, multicenter, nonrandomized phase II trial investigating triplet chemotherapy with docetaxel, CDDP, and S-1 [11, 12] for treating gastric cancer. These studies were carried out according to the ethical principles of the Declaration of Helsinki and Japanese Good Clinical Practice Guidelines. These studies were also approved by the institutional review board from each participating institution and hospital, and written informed consent was obtained upon registration (UMIN registration numbers C000000080, UMIN000000801, UMIN000002361). Inclusion criteria were as follows: histologically confirmed gastric adenocarcinoma; locally advanced or distant metastatic disease, judged to be radically unresectable at the time of registration; no uncontrolled infectious or cardiac diseases; adequate renal, hepatic, and bone marrow functions; no prior history of gastric surgery, chemotherapy, or radiotherapy; and an Eastern Cooperative Oncology scale performance status of 0–1. Tumor invasion, numbers of lymph node metastases, and distant metastases were graded by TNM classification, according to the 14th Japanese Classification of Gastric Carcinoma staging system [21].
S-1 was orally administered twice daily for 2 weeks at a dose calculated as described previously [12]. CDDP was administered by intravenous infusion at 60 mg/m2 for 2 h with adequate hydration, followed by docetaxel administration at either 50 or 60 mg/m2 on day 8. Patients received this regimen every 3 weeks for two or more cycles, and chemotherapeutic responders were treated by radical surgical resection, which was scheduled for at least 4 weeks after completion of the last cycle of chemotherapy. Patient eligibility for radical resection surgery was at the discretion of both an internist and a surgeon, who judged the chemotherapeutic responses by endoscopy, computed tomography, and staging laparoscopy. Adverse events were evaluated according to the National Cancer Institute Common Toxicity Criteria grading scale, version 3.0 [22]. The chemotherapeutic histopathological responses in resected specimens were classified according to the recommendations of the Japanese Gastric Cancer Association [21]. After surgery, most patients (57 of 69) were treated with S-1 as postoperative chemotherapy at the physician’s discretion.
BAK protein immunohistochemistry
Gastric cancer biopsy specimens were prospectively collected for clinical diagnosis and biomarker analysis, according to a protocol established in the three clinical trials mentioned previously. Sixty-nine gastric cancer samples were collected before preoperative chemotherapy between March 2005 and December 2013. Paraffin-embedded specimens were sliced into 3-μm-thick sections and mounted on glass slides, followed by staining with an anti-BAK antibody (Cell Signaling Technology, #6947) and Mayer’s hematoxylin, using an automated Leica BOND-MAX IHC system (Leica Biosystems, Nussloch, Germany) [23]. Two pathologists (T.H. and S.S.), who were blinded to clinical outcomes, independently assessed BAK immunostaining, as described [24, 25]. Briefly, two categories of positivity and staining intensity in the gastric cancer cells were assessed and classified as having scores ranging from 1 to 3 (positivity scores 1–3: 0–19, 20–59, and 60–100 %, respectively; intensity scores 1–3: no or weak intensity, moderate intensity, and strong intensity, respectively). These two values were multiplied, resulting in BAK-index scores ranging from 1 to 9.
Statistical analysis
For in vitro testing, all correlation calculations were performed by the Spearman rank (r s) correlation test. Comparison calculations between the control and experimental groups were performed by analysis of variance (ANOVA) with Dunnett’s multiple comparison test.
For clinical sample analysis, the cutoff date was set at December 31, 2014. We did not estimate a pre-planned sample size to obtain power calculations for biomarker analysis. For comparisons between pathological responses, the Mann–Whitney U test was used. Receiver operating characteristic curves defining the ability to predict histopathological responses were constructed, and optimal cutoff values were determined by the Youden index [26]. Overall survival (OS) was defined as the duration from the date of registration to the date of death from any cause. Progression-free survival (PFS) was defined as the duration from the date of registration to the date of either progressive disease or death from any cause after surgery. Tumor responses to chemotherapy were assessed by the Response Evaluation Criteria in Solid Tumours and Primary Lesions, version 1.0 [27].
Survival analysis was performed by the Kaplan–Meier method and compared using the log-rank test. The influence of each biological variable on clinical outcomes was analyzed by a Cox proportional hazards model in a stepwise manner. All statistical analyses were performed using SPSS software, version 21 (SPSS, Chicago, IL, USA).
Results
Positive correlation of BIM-BH3 profiling results with docetaxel sensitivity
Initially, we examined the cytotoxicity of docetaxel, CDDP, and 5-FU to 11 gastric cell lines, in both proliferation assays and apoptosis assays (Supplementary Fig. 1). The results showed a dynamic range of drug cytotoxicity between the gastric cell lines. When the mitochondrial transmembrane potential is lost following exposure to pro-apoptotic peptides derived from the BH3 domains of BH3-only proteins, cells are considered primed for death [15]. To study mitochondrial priming in gastric cancer cells, seven series of 10-μM BH3 peptides were tested (Fig. 1a). For BIM profiling, lower concentrations of the BIM BH3 peptide (up to 0.03 μM) were further tested (Fig. 1b) because most gastric cancer cells (>70 %) were fully primed when treated with 10 μM BIM BH3 peptide. Profiling following treatment with 1 μM BIM, 10 μM BID, and 10 μM BMF provided dynamic priming ranges when tested against 11 gastric cancer cell lines. Mitochondrial priming by 10 μM BAD and 10 μM PUMA peptide was observed only in KATO-III cells, suggesting survival dependence on the anti-apoptotic protein BCL-2 [15]. Less priming was seen following exposure to 10 μM NOXA and 10 μM HRK peptide.
a, b Heat map for mitochondrial responses in 11 gastric cancer cell lines to 7 BH3 peptides: seven series of 10-μM BH3 peptides (a) and different concentrations of BIM peptide (0.03–1 μM) (b) were tested. Correlation between apoptosis following treatment with 12 nM docetaxel and mitochondrial priming when treated with the BH3 peptides BIM (c), BID (d), and BMF (e). Correlation between IC50 values for docetaxel and mitochondrial priming following treatment with the BH3 peptides BIM (f), BID (g), and BMF (h). Values along the Y-axis (% annexin V negative and 7-AAD negative) indicate the percentages of living cells. The percentage of living cells following drug treatment was calculated by dividing the percentage of living (annexin V- and 7-AAD negative) cells treated with the indicated drug concentrations by the percentage of living, untreated cells. All correlation tests were evaluated by performing two-tailed Spearman correlations (r s)
We next investigated the correlation between BH3 profiling and cytotoxicity. In apoptosis assays, a strong correlation was observed between docetaxel treatment and mitochondrial priming by 1 μM BIM (r s = −0.88, P < 0.001; Fig. 1c), 10 μM BID (r s = −0.77, P = 0.006; Fig. 1d), and 10 μM BMF (r s = −0.75, P = 0.007; Fig. 1e). Mitochondrial priming by 1-μM BIM treatment was most strongly correlated with the IC50 for docetaxel (r s = −0.82, P = 0.002; Fig. 1f). There was no correlation between BH3 profiling and chemosensitivity to CDDP or 5-FU (data not shown). These data suggested that BIM profiling could predict docetaxel chemosensitivity.
BAK expression is strongly correlated with BIM-BH3 profiling
Because the BIM protein is known to interact with multiple apoptosis-related proteins [15], their expression levels were measured quantitatively (Fig. 2a). Only BAK expression positively correlated with mitochondrial priming by BIM (r s = 0.76, P = 0.006; Fig. 2b), whereas expression of any of the other proteins (data not shown), including endogenous BIM (Fig. 2c), did not. These data indicated that BIM profiling depended on BAK protein expression, but not on endogenous BIM protein expression.
Correlation between BIM-BH3 profiling and apoptosis-related protein expression. a Western blot analysis of apoptosis-related protein expression in 11 gastric cell lines: correlation between BIM-BH3 profiling and protein expression of BAK (b) and BIM (c). Relative protein expression levels were calculated by normalizing the expression of each protein to that of actin. All correlation tests were calculated by performing two-tailed Spearman correlations (r s)
Inhibition of BAK expression causes resistance to apoptosis following docetaxel treatment
To determine whether BAK protein expression could functionally affect docetaxel cytotoxicity, two gastric cancer cell lines, TMK1 and HSC39, were transfected with siRNAs targeting the human BAK transcript and then treated with docetaxel. Following BAK silencing, both gastric cancer cell lines were insensitive to the BIM peptide (Fig. 3c; Supplementary Fig. 2C) and resistant to docetaxel, compared with control siRNA-transfected cells (Fig. 3b, d; Supplementary Fig. 2b, 2d). To further assess the potential of BAK expression to predict the docetaxel chemosensitivity, the correlation between BAK expression and the IC50 for docetaxel in 11 gastric cancer cell lines was investigated. As shown in Fig. 3e, a strong correlation was observed between BAK expression and the IC50 for docetaxel (r s = −0.78, P = 0.004). These data showed that BAK expression in gastric cancer cells could directly affect sensitivity to docetaxel treatment.
Effect of BAK knockdown on docetaxel sensitivity in TMK1 cells. a Western blot analysis of BAK protein expression in BAK siRNA-transfected cells. Data shown are representative of three independent experiments. b Apoptosis assay results with siRNA-transfected TMK1 cells treated with docetaxel for 48 h. Y-axis indicates the percentage of living cells identified as both annexin V-negative and 7-AAD negative cells. All data represent mean ± SD (n = 3). c BIM-BH3 profiling in siRNA-transfected TMK1 cells. All data represent mean ± SD (n = 3). d Representative flow cytometry data from apoptosis assays. Values indicate percentage of living cells identified as both annexin-V negative and 7-AAD negative. P values (*P < 0.05, **P < 0.01) reflect significant differences observed, when compared with non-targeting siRNA (siNT)-transfected cells by analysis of variance (ANOVA) with Dunnett’s multiple-comparison test. e Correlation between BAK expression and IC50 values for docetaxel in 11 gastric cancer cell lines. A correlation test was calculated by performing two-tailed Spearman correlations (r s)
BAK expression significantly correlates with pathological chemotherapeutic effects
BAK protein expression was studied in gastric cancer cells obtained from 69 patients before preoperative chemotherapy with docetaxel, CDDP, and S-1 (Table 1). Seven of 31 patients registered with the UMIN C000000080 Trial were treated following resection by TNM clinical downstaging [11]. Gastric cancer cells from 40 patients enrolled in the UMIN 000000801 Trial [12] and 22 patients enrolled in the UMIN 000002361 Trial were also examined. At the time of analysis, the median follow-up time was 29.5 months (range, 3.6–96.4 months), and 46.4 % of the patients [32] had died. Thirty patients died of progressive disease, 1 patient died of a brain infarction, and 1 other patient died in a traffic accident. The clinical response rate to chemotherapy was 75.4 % (52 partial response, 17 stable disease). The incidence and severity of adverse events during preoperative chemotherapy were comparable with previous values (Supplementary Table 2) [12]. In 52 patients (75.4 %), residual tumors (R0) were found to be absent after surgery.
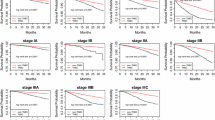
Next, we asked whether BAK indexes could facilitate the prediction of histopathological responses in resected specimens. The patients whose specimens showed good responses (grades 2 and 3) had higher BAK indexes (P = 0.018, Mann–Whitney U test; Fig. 4a, b) than patients whose specimens showed poor responses (grades 0, 1a, 1b). To further examine the correlation of the BAK indexes to clinical outcomes, we identified an optimal BAK index cutoff value of 3 (area under the curve, 0.662; sensitivity, 0.613; specificity, 0.658; Fig. 4c). Patients with higher BAK indexes (three or more) had both a longer OS (P = 0.010, log-rank test; Fig. 4d) and PFS (P = 0.007, log-rank test; Fig. 4e) compared with patients with fewer than three indexes. In univariate analysis (Table 2), the BAK indexes, TNM stage, and residual tumor status were independent factors for both OS and PFS. In multivariate analysis, the BAK indexes was found to be a prognostic indicator for OS (adjusted HR, 3.390; 95 % CI, 1.549–7.422; P = 0.002) and PFS (adjusted HR, 2.664; 95 % CI, 1.352–5.248; P = 0.005) before preoperative chemotherapy.
BAK expression in gastric cancer cells before preoperative chemotherapy. a Comparison of BAK indexes in patients whose specimens either showed a poor response (grade 0, 1a, or 1b) or a good response (grade 2 or 3). Comparisons between each group were made by performing Mann–Whitney U tests. b BAK immunostaining of representative gastric cancer specimens. Left BAK index = 1; middle BAK index = 4; right BAK index = 9. Bars 50 μm. c Receiver operating curve describing the ability of the BAK index to predict histopathological responses in the respective specimens. Kaplan–Meyer curve showing overall survival (OS) (d) and progression-free survival (PFS) (e), based on the BAK cutoff index
Discussion
Here, we explored biomarkers for predicting chemosensitivity to docetaxel, CDDP, and 5-FU in gastric cancer. BIM profiling strongly correlated with docetaxel cytotoxicity, and BAK protein expression in clinical gastric cancer cells before preoperative chemotherapy could predict histopathological responses to docetaxel. Our results suggested that BAK protein expression could be used to identify patients who might achieve an additional benefit when docetaxel is added to the perioperative regimen.
Cellular stress caused by cytotoxic drugs induces apoptosis-related proteins known as BCL-2 family proteins. In cells highly primed for death, the activity of pro-apoptotic BCL-2 family members overwhelms that of anti-apoptotic members, resulting in cell death. In less primed cells, the activities of anti-apoptotic BCL-2 family members prevent cell death. BAK, which stands for BCL-2 antagonist killer and functions as an “effector” member, is normally expressed in monomer form on the outer mitochondrial membrane [28]. When the intrinsic mitochondrial apoptosis-signaling pathway is activated by cellular damage, BAK homo-oligomerizes, resulting in permeabilization of the outer mitochondrial membrane and lost mitochondrial membrane potential [29]. BIM, which is also known as BCL2-like 11, contains a conserved BH3 region and functions as a pro-apoptotic activator of BAK and BAX [15]. BIM is usually bound to microtubules under physiological conditions and recruited to mitochondria caused by cytotoxic drugs [30]. Taxane agents can stabilize microtubules by interfering with spindle microtubule dynamics, resulting in cell-cycle arrest [6]. Previous results indicated that the BAK and BIM proteins were important in the cytotoxicity of taxane agents in breast and lung cancer cells [31–34]. However, as these apoptosis-related proteins take part in a complex network [15], it is difficult to predict apoptotic responses by quantifying simple protein expression.
BH3 profiling can be used as a functional assay for determining how living cells depend on these apoptosis-related proteins without regard to protein expression. The advantage of this profiling approach is that the understanding of mitochondrial priming in the living cells can be determined without exposure to drug treatment, enabling prediction of drug sensitivity when correlations do in fact exist. BH3 profiling has been examined in acute myelogenous leukemia and multiple myeloma [16, 17]. Profiling for BIM, BMF, and PUMA was found to predict drug responses and clinical outcomes. More recently, BH3 profiling could clarify the mechanism of resistance to Janus kinase inhibitors in myeloproliferative neoplasms [35] and for predicting cytotoxic responses in lung cancer and ovarian adenocarcinoma [36].
Previous reports have described predictors for docetaxel chemosensitivity in gastric cancer. Izzo et al. [37] reported an association of activated NF-κB with chemoradiation resistance and poor survival. NF-κB can directly activate expression of the anti-apoptotic protein BCL-XL [38], which prevents apoptosis. NF-κB expression is associated with drug resistance to docetaxel [39], CDDP [40], and 5-FU [41]; therefore, it may be difficult to predict chemotherapeutic responses to docetaxel only. Kaoru et al. [42] examined FoxM1 expression in gastric cancer specimens before docetaxel treatment, showing a correlation with survival. However, as they did not assess histopathological responses and R0, which strongly affect disease progression [13, 14], clinical outcomes after surgery remain obscure when compared with the results presented in this study.
There are some limitations to this study. Although clinically examined samples were collected at a multicenter hospital and institution, the sample size was relatively small. A prospective study of larger sample size needs to be conducted to validate the findings of this study in the future. As we did not study BAK expression in clinical gastric cancer cells before preoperative chemotherapy with CDDP and S-1, there could be confounding bias for validating the predictive value of BAK expression with our triplet regimen. A future study for examining Bim BH3 profiling in clinical gastric cancer cells before our triplet chemotherapy might elucidate this. There were also selection biases for patients who only underwent surgery and could be judged for histopathological responses. Hence, the interpretation of null-responders remains to be analyzed in terms of survival prognosis.
In conclusion, the results from this study demonstrated that BAK expression in gastric cancer cells is a potential biomarker for predicting chemotherapeutic responses to docetaxel. BAK expression could also predict clinical prognosis in patients treated with preoperative chemotherapy, which included docetaxel. Taken together, these data indicate that the modification of BAK expression and function could be a promising therapeutic strategy for overcoming docetaxel resistance in advanced gastric cancer. Furthermore, the combination of previously described biomarkers with BAK expression may enable a more detailed stratification of individual sensitivity to each drug, thereby increasing the possibilities for precision medicine.
References
Ferley J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al: GLOBOCAN 2012 v1.2. Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 11: International Agency for Research on Cancer. 2014. http://www.iarc.fr.
Matsuda T, Ajiki W, Marugame T, Ioka A, Tsukuma H, Sobue T. Population-based survival of cancer patients diagnosed between 1993 and 1999 in Japan: a chronological and international comparative study. Jpn J Clin Oncol. 2011;41:40–51. doi:10.1093/jjco/hyq167.
Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson M, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355:11–20.
Yoshikawa T, Sasako M, Yamamoto S, Sano T, Imamura H, Fujitani K, et al. Phase II study of neoadjuvant chemotherapy and extended surgery for locally advanced gastric cancer. Br J Surg. 2009;96(9):1015. doi:10.1002/bjs.6665.
Schuhmacher C, Gretschel S, Lordick F, Reichardt P, Hohenberger W, Eisenberger CF, et al. Neoadjuvant chemotherapy compared with surgery alone for locally advanced cancer of the stomach and cardia: European Organisation for Research and Treatment of Cancer randomized trial 40954. J Clin Oncol. 2010;. doi:10.1200/JCO.2009.26.6114.
Cortes JE, Pazdur R. Docetaxel. J Clin Oncol. 1995;13:2643–55.
Bissery MC, Guénard D, Guéritte-Voegelein F, Lavelle F. Experimental antitumor activity of taxotere (RP 56976, NSC 628503), a taxol analogue. Cancer Res. 1991;51:4845–52.
Van Cutsem E, Moiseyenko VM, Tjulandin S, Majlis A, Constenla M, Boni C, et al. Phase III study of docetaxel and cisplatin plus fluorouracil compared with cisplatin and fluorouracil as first-line therapy for advanced gastric cancer: a report of the V325 Study Group. J Clin Oncol. 2006;24:4991–7.
Ajani JA, Moiseyenko VM, Tjulandin S, Majlis A, Constenla M, Boni C, et al. Clinical benefit with docetaxel plus fluorouracil and cisplatin compared with cisplatin and fluorouracil in a phase III trial of advanced gastric or gastroesophageal cancer adenocarcinoma: the V-325 Study Group. J Clin Oncol. 2007;25:3205–9.
Shirasaka T. Development history and concept of an oral anticancer agent S-1 (TS-1): its clinical usefulness and future vistas. Jpn J Clin Oncol. 2009;. doi:10.1093/jjco/hyn127.
Sato Y, Takayama T, Sagawa T, Takahashi Y, Ohnuma H, Okubo S, et al. Phase II study of S-1, docetaxel and cisplatin combination chemotherapy in patients with unresectable metastatic gastric cancer. Cancer Chemother Pharmacol. 2010;. doi:10.1007/s00280-009-1215-2.
Hirakawa M, Sato Y, Ohnuma H, Takayama T, Sagawa T, Nobuoka T, et al. A phase II study of neoadjuvant combination chemotherapy with docetaxel, cisplatin, and S-1 for locally advanced resectable gastric cancer: nucleotide excision repair (NER) as potential chemoresistance marker. Cancer Chemother Pharmacol. 2013;. doi:10.1007/s00280-013-2073-5.
Wu TT, Chirieac LR, Abraham SC, Krasinskas AM, Wang H, Rashid A, et al. Excellent interobserver agreement on grading the extent of residual carcinoma after preoperative chemoradiation in esophageal and esophagogastric junction carcinoma: a reliable predictor for patient outcome. Am J Surg Pathol. 2007;31:58–64.
Bain GH, Petty RD. Predicting response to treatment in gastroesophageal junction adenocarcinomas: combining clinical, imaging, and molecular biomarkers. Oncologist. 2010;. doi:10.1634/theoncologist.2009-0293.
Ryan J, Brunelle JK, Letai A. Heightened mitochondrial priming is the basis for apoptotic hypersensitivity of CD4+ CD8+ thymocytes. Proc Natl Acad Sci USA. 2010;. doi:10.1073/pnas.0914878107.
Ni Chonghaile T, Sarosiek KA, Vo TT, Ryan JA, Tammareddi A, Moore Vdel G, et al. Pretreatment mitochondrial priming correlates with clinical response to cytotoxic chemotherapy. Science. 2011;. doi:10.1126/science.1206727.
Vo TT, Ryan J, Carrasco R, Neuberg D, Rossi DJ, Stone RM, et al. Relative mitochondrial priming of myeloblasts and normal HSCs determines chemotherapeutic success in AML. Cell. 2012;. doi:10.1016/j.cell.2012.08.038.
Ochiai A, Yasui W, Tahara E. Growth-promoting effect of gastrin on human gastric carcinoma cell line TMK-1. Jpn J Cancer Res. 1985;76:1064–71.
Kawano Y, Kobune M, Yamaguchi M, Nakamura K, Ito Y, Sasaki K, et al. Ex vivo expansion of human umbilical cord hematopoietic progenitor cells using a coculture system with human telomerase catalytic subunit (hTERT)-transfected human stromal cells. Blood. 2003;101:532–40.
Murase K, Kim HT, Bascuq OR, Kawano Y, Ryan J, Matsuoka K, et al. Increased mitochondrial apoptotic priming of human regulatory T cells after allogeneic hematopoietic stem cell transplantation. Haematologica. 2014;. doi:10.3324/haematol.2014.104166.
Association Japanese Gastric Cancer. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;. doi:10.1007/s10120-011-0041-5.
National Cancer Institute Common Toxicity Criteria, version 3.0: Cancer Therapy Evaluation Program. 1998. http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf.
Martins RG, Parvathaneni U, Bauman JE, Sharma AK, Raez LE, Papagikos MA, et al. Cisplatin and radiotherapy with or without erlotinib in locally advanced squamous cell carcinoma of the head and neck: a randomized phase II trial. J Clin Oncol. 2013;. doi:10.1200/JCO.2012.46.3299.
Krajewska M, Krajewski S, Epstein JI, Shabaik A, Sauvageot J, Song K, et al. Immunohistochemical analysis of bcl-2, bax, bcl-X, and mcl-1 expression in prostate cancers. Am J Pathol. 1996;148:1567–76.
Barrezueta LF, Oshima CT, Lima FO, De Oliveira Costa H, Gomes TS, Neto TS, et al. The intrinsic apoptotic signaling pathway in gastric adenocarcinomas of Brazilian patients: immunoexpression of the Bcl-2 family (Bcl-2, Bcl-x, Bak, Bax, Bad) determined by tissue microarray analysis. Mol Med Rep. 2010;. doi:10.3892/mmr_00000249.
Youden WJ. Index for rating diagnostic tests. Cancer (Phila). 1950;3:32–5.
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92:205–16.
Wei MC, Lindsten T, Mootha VK, Weiler S, Gross A, Ashiya M, et al. tBID, a membrane-targeted death ligand, oligomerizes BAK to release cytochrome c. Genes Dev. 2000;14:2060–71.
Kluck RM, Bossy-Wetzel E, Green DR, Newmeyer DD. The release of cytochrome c from mitochondria: a primary site for Bcl-2 regulation of apoptosis. Science. 1997;275:1132–6.
Klotz DM, Nelson SA, Kroboth K, Newton IP, Radulescu S, Ridgway RA, et al. The microtubule poison vinorelbine kills cells independently of mitotic arrest and targets cells lacking the APC tumour suppressor more effectively. J Cell Sci. 2012;. doi:10.1242/jcs.091843.
Zhou M, Liu Z, Zhao Y, Ding Y, Liu H, Xi Y, et al. MicroRNA-125b confers the resistance of breast cancer cells to paclitaxel through suppression of pro-apoptotic Bcl-2 antagonist killer 1 (Bak1) expression. J Biol Chem. 2010;. doi:10.1074/jbc.M109.083337.
Miller AV, Hicks MA, Nakajima W, Richardson AC, Windle JJ, Harada H. Paclitaxel-induced apoptosis is BAK-dependent, but BAX and BIM-independent in breast tumor. PLoS ONE. 2013;. doi:10.1371/journal.pone.0060685.
Li R, Moudqil T, Ross HJ, Hu HM. Apoptosis of non-small-cell lung cancer cell lines after paclitaxel treatment involves the BH3-only proapoptotic protein Bim. Cell Death Differ. 2005;12:292–303.
Savry A, Carre M, Berges R, Rovini A, Pobel I, Chacon C, et al. Bcl-2-enhanced efficacy of microtubule-targeting chemotherapy through Bim overexpression: implications for cancer treatment. Neoplasia. 2013;15:49–60.
Winter PS, Sarosiek KA, Lin KH, Meggendorfer M, Schnittger S, Letai A, et al. RAS signaling promotes resistance to JAK inhibitors by suppressing BAD-mediated apoptosis. Sci Signal. 2014;. doi:10.1126/scisignal.2005301.
Montero J, Sarosiek KA, DeAngelo JD, Maertens O, Ryan J, Ercan D, et al. Drug-induced death signaling strategy rapidly predicts cancer response to chemotherapy. Cell. 2015;. doi:10.1016/j.cell.2015.01.042.
Izzo JG, Malhotra U, Wu TT, Ensor J, Luthra R, Lee JH, et al. Association of activated transcription factor nuclear kappaB with chemoradiation resistance and poor outcome in esophageal carcinoma. J Clin Oncol. 2006;24:748–54.
Chen C, Edelstein LC, Gélinas C. The Rel/NF-kappaB family directly activates expression of the apoptosis inhibitor Bcl-x(L). Mol Cell Biol. 2000;20:2687–95.
Huang Y, Johnson KR, Norris JS, Fan W. Nuclear factor-kappaB/IkappaB signaling pathway may contribute to the mediation of paclitaxel-induced apoptosis in solid tumor cells. Cancer Res. 2000;60:4426–32.
Eichholtz-Wirth H, Sagan D. IkappaB/NF-kappaB mediated cisplatin resistance in HeLa cells after low-dose gamma-irradiation is associated with altered SODD expression. Apoptosis. 2000;5:255–63.
Camp ER, Li J, Minnich DJ, Brank A, Moldawer LL, MacKay SL, et al. Inducible nuclear factor-kappaB activation contributes to chemotherapy resistance in gastric cancer. J Am Coll Surg. 2004;199:249–58.
Okada K, Fujiwara Y, Takahashi T, Nakamura Y, Takiguchi S, Nakajima K, et al. Overexpression of forkhead box M1 transcription factor (FOXM1) is a potential prognostic marker and enhances chemoresistance for docetaxel in gastric cancer. Ann Surg Oncol. 2013;. doi:10.1245/s10434-012-2680-0.
Acknowledgments
We thank the staff at the Biomedical Research Center (Division of Morphological Research) and the Division of Digital Imaging at the Sapporo Medical University School of Medicine. We greatly thank Yumiko Kaneko for preparing and managing the clinical samples. We also thank Dr. Minami Shinya, Dr. Takanashi Kunihiro, Dr. Sagawa Tamotsu, Dr. Okubo Syunichi, Dr. Maeda Masahiro, Dr. Katsuki Shinnichi, Dr. Takahashi Minoru, Dr. Takahashi Yasuo, Dr. Takaoka Yoshifumi, and Dr. Miyamoto Hiroshi, who all kindly provided us the clinical information. This study was funded by Grants-in-Aid for Scientific Research (Grant Number 26460943). The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical standards
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (Sapporo Medical University School of Medicine) and with the Helsinki Declaration of 1964 and later versions. Informed consent was obtained from all patients for being included in the study.
Additional information
Tomohiro Kubo and Yutaka Kawano contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Fig. 1.
The IC50 values of docetaxel (a), CDDP (b), and 5-FU (c) in 11 gastric cell lines. The IC50 was defined as the drug concentration resulting in 50 % cell survival when compared with untreated cells, as measured in triplicate wells treated with various drug concentrations. Apoptosis assay results following treatment with 12 nM docetaxel (d), 12 μM CDDP (e), and 20 μM 5-FU (f) for 72 h. Y-axis values (d–f) indicate the percentage of living cells described in the legend of Fig. 1. All data represent the mean ± SD (n = 3). 1, MKN74; 2, MKN45; 3, NCI-N87; 4, JR-St; 5, NUGC-4; 6, KATO-III; 7, HSC-39; 8, NUGC-3; 9, MKN1; 10, TMK1; 11, NUGC-2 (PDF 358 kb)
Supplementary Fig. 2.
Effect of BAK knockdown on docetaxel sensitivity in HSC39 cells. a Western blot analysis of BAK protein expression in siRNA-transfected cells. Data shown are representative of three independent experiments. b Apoptosis assay results obtained with siRNA-transfected TMK1 cells treated with docetaxel for 48 h. Y-axis indicates the percentage of living cells. All data represent mean ± SD (n = 3). c BIM priming in siRNA-transfected TMK1 cells. All data represent mean ± SD (n = 3). d Representative flow cytometry data obtained in the apoptosis assays. The values indicate the percentage of living cells identified as both annexin V negative and 7-AAD negative. P values (*P < 0.05, ** P < 0.01) reflect significant differences observed when compared with nontargeting siRNA (siNT)-transfected cells by ANOVA with Dunnett’s multiple comparison test (PDF 532 kb)
Rights and permissions
About this article
Cite this article
Kubo, T., Kawano, Y., Himuro, N. et al. BAK is a predictive and prognostic biomarker for the therapeutic effect of docetaxel treatment in patients with advanced gastric cancer. Gastric Cancer 19, 827–838 (2016). https://doi.org/10.1007/s10120-015-0557-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-015-0557-1