Abstract
Background
Gastric cancer after successful Helicobacter pylori eradication therapy is often difficult to diagnose by endoscopy because of its indistinct borderline or lack of obviously cancerous characteristics. Furthermore, it has become evident that non-neoplastic epithelium covers cancerous areas in gastric cancer after eradication. Here, we investigated these endoscopic features and their relationship to histological findings.
Methods
We studied 24 and 47 gastric cancers in patients who had (eradication group) and had not (control group) undergone H. pylori eradication, respectively. A gastritis-like appearance revealed by conventional endoscopy was defined as a mucosal pattern with no marked difference from the surrounding non-cancerous area and that revealed by narrow-band imaging (NBI)-magnifying endoscopy (ME) as the mucosal pattern observed in H. pylori-associated atrophic gastritis. We investigated a gastritis-like appearance revealed by conventional endoscopy (A), a gastritis-like appearance at the margin (B) and within (C) the cancerous area revealed by NBI-ME, and the histological characteristics of the overlying non-neoplastic epithelium. We also evaluated the relationship between endoscopic and histological findings in the eradication group.
Results
Endoscopy showed that features A, B and C were significantly more frequent in the eradication group (P = 0.031, P < 0.001, P < 0.001, respectively). Non-neoplastic epithelium covered more than 10 % of the cancerous area more frequently in the eradication group. In the eradication group, more than 90 % of cancers showing a gastritis-like appearance had non-neoplastic epithelium extending over 10 % of the cancerous area.
Conclusion
Gastric cancer after successful H. pylori eradication tends to have gastritis-like features due to non-neoplastic epithelium covering the cancerous tissue.
Similar content being viewed by others
Introduction
It has been clarified that gastric cancer develops as a result of persistent infection with Helicobacter pylori. A previous prospective study conducted in Japan showed that the incidence of metachronous gastric cancer was reduced to one-third when H. pylori eradication therapy was provided after endoscopic resection of early gastric cancer [1]. Therefore, the Japanese government approved national health insurance system coverage of eradication therapy for patients with H. pylori-associated gastritis. However, Kamada et al. [2] reported an annual gastric cancer incidence rate of 0.24 % in patients who had undergone successful eradication therapy. We have realized that gastric cancer after H. pylori eradication is often difficult to diagnose by endoscopy because of its indistinct borderline or lack of obviously cancerous characteristics. Furthermore, histologically, gastric cancer after eradication of H. pylori is often covered by non-neoplastic epithelium [3]. Accordingly, we attempted to clarify the features of gastric cancer demonstrated by conventional endoscopic and narrow-band imaging (NBI)-magnifying endoscopy after successful eradication of H. pylori. In order to confirm whether the indistinct borderline and lack of cancerous characteristics are, in fact, related to such non-neoplastic epithelium, we assessed the histological features of such cancers and then devised an NBI-magnifying endoscopy method for more accurate diagnosis of gastric cancer in patients after successful H. pylori eradication therapy.
Patients and methods
Patients
For the purposes of this study, we defined gastric cancer after successful H. pylori eradication as that which was detected and diagnosed at least 1 year after the therapy. We enrolled 22 patients with 24 consecutive gastric cancers after successful H. pylori eradication who had been treated by endoscopic submucosal dissection (ESD) at Niigata Prefectural Yoshida Hospital between April 2010 and April 2014 (eradication group). The efficacy of H. pylori eradication treatment was evaluated by the 13C-urea breath test (UBIT, Otsuka, Tokushima, Japan) and the H. pylori stool antigen test (Premier Platinum HpSA; Meridian, Cincinnati, OH, USA). If the results were negative in both tests, we judged that H. pylori eradication had been successful.
To provide a control group, we registered 40 patients with 47 consecutive gastric cancers who had not undergone H. pylori eradication therapy but had also undergone ESD during the same period (control group). As these lesions were selected randomly, there were no significant differences between the two groups in terms of patient age, sex, histologic type and invasion depth. Patients with autoimmune gastritis, previous gastrectomy or severe hepatorenal dysfunction were excluded. In the control group, 28 patients had been examined for H. pylori, and 12 had not. The presence of H. pylori infection was determined by at least one of the following methods: the 13C-urea breath test (UBIT, Otsuka, Tokushima, Japan), H. pylori stool antigen test (Premier Platinum HpSA; Meridian, Cincinnati, OH, USA), serum immunoglobulin (Ig) G antibody test (E-plate, Eiken, Tokyo, Japan) and biopsy culture. Nineteen patients were H. pylori-positive, and nine were negative. The study protocol was approved by our institutional ethics committee.
Clinical characteristics of patients and gastric cancers
In both groups, we examined patient age, sex, degree of endoscopic gastric mucosal atrophy, lesion size, location, color, macroscopic type, histological type and depth of invasion, and in the eradication group we examined the period between eradication therapy and detection of gastric cancer as well as the reason for eradication therapy. The degree of endoscopic gastric mucosal atrophy was judged according to the Kimura and Takemoto [4] classification. Tumor histology was evaluated according to the Japanese Classification of Gastric Carcinoma, 14th edition [5].
Endoscopic procedure and evaluation of endoscopic features of gastric cancers
The instruments used in the present study were a magnifying videoendoscope and an electronic endoscopic system (GIF-H260Z and EVIS LUCERA Spectum; Olympus Medical Systems, Tokyo, Japan).
A gastritis-like appearance demonstrated by conventional endoscopy was defined as a mucosal pattern with no marked difference in mucosal texture relative to the surrounding non-cancerous area, although slight elevation or depression was evident [6]. A gastritis-like appearance demonstrated by NBI-magnifying endoscopy was defined as the mucosal pattern observed in chronic atrophic gastritis due to H. pylori infection, i.e., oval or slit-like pits surrounded by a groove, or a tubular or granular pattern, with a regular microvascular pattern [7]. We evaluated whether or not the following endoscopic features were evident in the two groups and whether there was a significant inter-group difference in their incidence:
-
(A)
A gastritis-like appearance demonstrated by conventional endoscopy (Fig. 1a).
Fig. 1 Endoscopic features of gastric cancer after successful H. pylori eradication therapy. a Conventional endoscopic view shows a gastritis-like appearance (arrows). Slight elevation can be seen, but there is no marked difference in mucosal texture between the cancerous area and surrounding non-cancerous area. The surrounding non-cancerous area has been marked by high-frequency waves for ESD. b NBI-magnifying endoscopic view of the proximal side of the gastric cancer, showing a gastritis-like appearance at the cancer margin (arrows), making the borderline of the lesion indistinct. c NBI-magnifying endoscopic view of the proximal side of the gastric cancer, showing the cancerous margin (dotted line), which is similar to the surrounding mucosa, and an area showing a gastritis-like appearance within the cancerous area (arrows). Therefore, the entire area of the gastric cancer appears to lack cancerous features
-
(B)
A gastritis-like appearance at the margin of the cancerous area, creating an indistinct borderline, demonstrated by NBI-magnifying endoscopy (Fig. 1b).
-
(C)
A gastritis-like appearance within the cancerous area demonstrated by NBI-magnifying endoscopy (Fig. 1c).
Endoscopic features A, B and C were considered to be those making diagnosis of cancerous lesions difficult. The borderline between cancer and the surrounding non-cancerous mucosa was discriminated as a slight difference in the mucosal pattern, because—in cancer with a gastritis-like appearance—we had recognized that the cancerous area showed a mucosal pattern that, although gastritis-like, was slightly different from the surrounding non-cancerous mucosa. On the other hand, irregular mucosa that is characteristic of gastric cancer shows features including a non-uniform size, shape and arrangement. Irregular microvascular patterns, which are also characteristic of gastric cancer, include inequality of caliber and irregularity of arrangement. Gastric cancer with an irregular mucosal and microvascular pattern can be easily recognized as cancer by NBI-magnifying endoscopy.
All of the endoscopic examinations were performed by two expert endoscopists (AS and KY). Endoscopic features A, B and C were identified by each of the endoscopists independently on the basis of the endoscopic pictures. If their opinions did not agree, a final judgment was arrived at by consensus following discussion of each individual case. During evaluation of the endoscopic pictures, the two endoscopists were blinded to any history of successful H. pylori eradication therapy and histological findings.
Evaluation of the histological features of gastric cancers
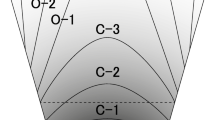
We focused on the histological evaluation of non-neoplastic epithelium covering the intramucosal carcinoma (Fig. 2) and classified it into three grades according to the extent of the non-neoplastic epithelium.
Histological features of gastric cancer after successful H. pylori eradication therapy. a ×100 Representative histological features of non-neoplastic epithelium at the surface of an intramucosal differentiated-type carcinoma. A few lympho-plasmacytes are also evident in the lamina propria mucosae. b ×200 Non-neoplastic epithelia (box area in a) are highly magnified and indicated by the dotted line. The surface epithelia consist of mature foveolar epithelium without cytological atypia, forming a distinct boundary with the area of differentiated carcinoma 
Grade 0: ≤10 % of the entire cancerous area.
Grade 1: more than 10 % and ≤50 % of the entire cancerous area.
Grade 2: more than 50 % of the entire cancerous area.
We examined all of the specimens resected by ESD in the two groups to investigate the grade of the non-neoplastic epithelium and assessed whether there was any significant inter-group difference in the grade. Evaluation was done using specimens stained with hematoxylin and eosin (HE). We defined non-neoplastic epithelium as surface epithelium without cytological atypia, forming a distinct boundary with the area of cancer.
Histological evaluation was performed by an expert pathologist (SN) independently of the endoscopists. This pathologist was blinded to the history of successful H. pylori eradication therapy and endoscopic findings.
Relationship between gastric cancers showing endoscopic features A, B and C and the three histological grades in the eradication group
In the eradication group, we investigated whether or not the histological grade—grade 0, 1 or 2—was related to endoscopic features A, B and C in gastric cancers.
Relationship between endoscopic features and histological grade, and the period after eradication therapy
In the eradication group, we divided gastric cancers into two clusters: those detected ≤10 years after eradication and those detected after more than 10 years. We then investigated whether or not these two clusters showed any correlation with endoscopic features A, B and C or with the histological grade.
Statistical analysis
Results are reported as mean ± SD. All statistical analyses were performed using the t test and chi squared test with Stat Mate IV for Windows (ATMS Inc., Tokyo, Japan). Differences at P < 0.05 were considered to be statistically significant.
Results
Clinical characteristics of patients and gastric cancers in the two groups (Table 1)
Clinicohistological data for the eradication group and control group are summarized in Table 1. There were no significant differences between the groups in terms of patient age, sex, degree of endoscopic gastric mucosal atrophy, lesion size, color, histological type and depth of invasion. The lesions in the eradication group were located in the middle part of the stomach more frequently than those in the control group. In the eradication group, the frequency of elevated lesions was lower than in the control group, and the mean period between eradication therapy and detection of gastric cancer was 5.9 years (range 1–14 years). The reasons for eradication therapy were gastric or gastroduodenal ulcer (50 %), gastric cancer after endoscopic resection (27.3 %), and gastric adenoma (22.7 %).
Endoscopic features of gastric cancers in the two groups (Table 2)
A gastritis-like appearance revealed by conventional endoscopy (A) and NBI-magnifying endoscopic findings of a gastritis-like appearance at the margin of cancer (B) and within the cancerous area (C) were observed significantly more frequently in the eradication group than in the control group (P = 0.031, P < 0.001, P < 0.001, respectively).
Histological grades of gastric cancers in the two groups (Table 3)
Grade 0 was significantly more frequent in the control group (93.6 %) than in the eradication group (33.3 %) (P < 0.001). However, grades 1 and 2 were significantly more frequent in the eradication group than in the control group (P < 0.001, P = 0.013, respectively).
Relationship between gastric cancers showing endoscopic features A, B and C and the three histological grades in the eradication group (Table 4)
Over 90 % of gastric cancers showing endoscopic features A, B or C in the eradication group were confirmed to have non-neoplastic epithelium covering more than 10 % of the entire cancerous area (grade 1 or 2) histologically. On the other hand, 87.5 % of gastric cancers without endoscopic features A, B and C were histological grade 0.
Relationship between endoscopic features and histological grade, and the period after eradication therapy (Table 5)
There was no relationship between endoscopic features and the period after eradication therapy. However, histological grade 2 was significantly more frequent in patients who had undergone eradication therapy more than 10 years previously (P = 0.013).
Discussion
Several studies have reported preventive effects of H. pylori eradication therapy against gastric cancers [1, 8, 9]. However, it has been clarified that primary or metachronous gastric cancers may be discovered even after successful eradication therapy [2, 10]. Previously, Kamada et al. [2, 11] reported that the features of gastric cancer detected after successful eradication therapy were a lesion size of typically <20 mm, location in the middle and lower parts of the stomach, a depressed microscopic type and a differentiated histology. In the present study, gastric cancers after H. pylori eradication were mainly <20 mm (16.6 mm) in size, located in the middle part of the stomach and appeared depressed macroscopically; all of the lesions were histologically differentiated type adenocarcinoma. These results are similar to those reported by Kamada et al.
It has been recognized that gastric cancer detected after H. pylori eradication is often difficult to diagnose by endoscopy because of its indistinct border or lack of obvious cancerous characteristics. Furthermore, upon histological examination of specimens resected by ESD, non-neoplastic epithelium is often found to cover the cancerous tissue.
Ito et al. [12] have reported that the endoscopic features of gastric cancer changed to a flattened and indistinct form after H. pylori eradication and that non-neoplastic epithelium covered the neoplasm in 73 % of indistinct lesions.
On the other hand, in a study using NBI-magnifying endoscopy and histological examination of controls and patients who had undergone H. pylori eradication, Kobayashi et al. [13] reported that a gastritis-like appearance revealed by NBI-magnifying endoscopy was observed more frequently in the eradication group and was correlated with histological surface differentiation. These previous studies suggested that the endoscopic and histological features of gastric cancer after successful H. pylori eradication therapy differ from those of gastric cancer we have observed previously.
Accordingly, we designed the present study to clarify the degree to which gastric cancer after H. pylori eradication is indistinct or gastritis-like, relative to a control group, using conventional endoscopy and NBI-magnifying endoscopy. We focused particularly on indistinct recognition of gastric cancer by conventional endoscopy, the difficulty in determining the borderline margin of the cancer and confidence of cancer diagnosis within the cancerous area, using NBI-magnifying endoscopy. Furthermore, to clarify whether an indistinct borderline and lack of obvious cancerous characteristics are related to non-neoplastic epithelium covering the cancerous tissue, we investigated the histological features of the gastric cancers.
We confirmed that the frequency of a gastritis-like appearance by conventional endoscopy was significantly higher in the eradication group than in the control group (Table 1. P = 0.031). A gastritis-like appearance evident on conventional endoscopy masks any obvious cancerous characteristics, thus making it difficult to detect and diagnose gastric cancer accurately [3].
NBI-magnifying endoscopy also demonstrated a gastritis-like appearance at the cancer margin more frequently in the eradication group than in the control group (Table 1; P < 0.001), making it difficult to delineate the borderline between the cancerous area and the surrounding non-cancerous mucosa. In Japan, ESD is carried out widely, and for accurate curability it is necessary to delineate the border of the cancerous area accurately. This may be difficult to achieve after H. pylori eradication because of the indistinct nature of the cancerous borderline. Furthermore, a gastritis-like appearance within the cancerous area would make endoscopists less confident about diagnosing the cancer.
As one possible reason for the development of a gastritis-like appearance, we focused on non-neoplastic epithelium covering cancerous tissue. Non-neoplastic epithelium was observed more frequently in the eradication group, and in more than 90 % of such cancers the non-neoplastic epithelium covered over 10 % of the cancerous area. However, even in the eradication group, non-neoplastic epithelium covered over 10 % of the cancerous area in only 12.5 % of gastric cancers that did not show a gastritis-like appearance. This result confirmed that the gastritis-like appearance is attributable to non-neoplastic epithelium covering the cancerous tissue.
Furthermore, we investigated the extent to which non-neoplastic epithelium covering cancerous tissue might be influenced by the period after eradication therapy. It was found that 50 % of gastric cancers detected more than 10 years after H. pylori eradication showed non-neoplastic epithelium over 50 % of the cancerous area, whereas this feature was evident in only 5 % of gastric cancers detected ≤10 years after eradication.
Non-neoplastic epithelium covering cancerous tissue has previously been reported as a specific histological feature of gastric cancer after successful eradication of H. pylori [12]. As well as histological surface differentiation of cancer [13], surface epithelium with low-grade atypia has also been reported [14]. All of these histological findings were reported to make endoscopic diagnosis difficult, although it remains unresolved whether the latter two types of epithelium are neoplasia or non-neoplasia.
To diagnose gastric cancer showing a gastritis-like appearance after H. pylori eradication, we think the following measures are necessary [3]. (1) First, endoscopists should be aware that gastric cancer after H. pylori eradication tends to show gastritis-like features. (2) Even if gastric cancer shows such features, NBI-magnifying endoscopy can indicate differences in patterning relative to the surrounding non-cancerous mucosa, and it is important to detect this difference. (3) Slight irregularity can be discerned by careful observation using NBI-magnifying endoscopy. Consequently, it is necessary to delineate the borderline of the cancerous area if any slight irregularity is evident.
We have reported the features revealed by NBI-magnifying endoscopy that are helpful for determining whether a stomach has been treated for eradication of H. pylori [15]. If this is the case, then the endoscopic diagnosis procedure described above should be carried out.
In this study, we investigated gastric cancers in patients who had undergone successful H. pylori eradication therapy and in those who had not. In some patients, however, H. pylori infection sometimes resolves naturally. Therefore, in the future, it will be necessary to compare such patients with those who have undergone successful H. pylori eradication therapy. In conclusion, gastric cancer after successful H. pylori eradication therapy tends to have a gastritis-like appearance, which is attributable to non-neoplastic epithelium covering the cancerous tissue. To diagnose gastric cancer after successful H. pylori eradication therapy, it is necessary to be aware of its possible presence and to perform careful endoscopic observation.
References
Fukase K, Kato M, Kikuchi S, Inoue K, Uemura N, Okamoto S, et al. Effect of eradication of Helicobacter pylori on incidence of metachronous gastric carcinoma after endoscopic resection of early gastric cancer: an open-label, randomised controlled trial. Lancet. 2008;372:392–7.
Kamada T, Hata J, Sugiu K, Kusunoki H, Ito M, Tanaka S, et al. Clinical features of gastric cancer discovered after successful eradication of Helicobacter pylori: results from a 9-year prospective follow-up study in Japan. Aliment Pharmacol Ther. 2005;21:1121–6.
Yagi K, Saka A, Nozawa Y, Nakamura A, Nimura S. Endoscopic diagnosis of gastric cancer after successful H. pylori eradication therapy. Gastroenterol Endosc 2015 (in press).
Kimura K, Takemoto T. An endoscopic recognition of the atrophic border and its significance in chronic gastritis. Endoscopy. 1969;3:87–97.
Japanese Classification of Gastric Carcinoma March 2010 (ed 14). Japanese Gastric Cancer Association, 2010.
Yoshida S, Yamaguchi H, Saito D, Kido M. Endoscopic diagnosis: latest trends. Gastric cancer. Tokyo: Springer-Verlag; 1993. p. 246–62.
Yagi K, Sato T, Nakamura A, Sekine A. Magnifying endoscopic findings, using NBI, of chronic gastritis due to Helicobacter pylori infection. Stomach Intest. 2009;44:1446–55 (in Japanese with English abstract).
Take S, Mizuno M, Ishiki K, Nagahara Y, Yoshida T, Yokota K, et al. The effect of eradicating Helicobacter pylori on the development of gastric cancer in patients with peptic ulcer disease. Am J Gastroenterol. 2005;100:1037–42.
Mabe K, Takahashi M, Oizumi H, Tsukuma H, Shibata A, Fukase K, et al. Does Helicobacter pylori eradication therapy for peptic ulcer prevent gastric cancer? World J Gastroenterol. 2009;15:4290–7.
Take S, Mizuno M, Ishiki K, Yoshida T, Ohara N, Yokota K, et al. The long term risk of gastric cancer after the successful eradication of Helicobacter pylori. J Gastroenterol. 2011;46:318–24.
Kamada T, Mabe K, Fukase K, Inoue K, Okada H, Matsuo T, et al. Clinicopathological features of gastric cancer detected after Helicobacter pylori eradication: results from 100 cases of gastric cancer in a multi-center study. Stomach Intest. 2008;43:1810–9 (in Japanese with English abstract).
Ito M, Tanaka S, Takata S, Oka S, Imagawa H, Ueda Y, et al. Morphological changes in human gastric tumours after eradication therapy of Helicobacter pylori in a short-term follow-up. Aliment Pharmacol Ther. 2005;21:559–66.
Kobayashi M, Hashimoto S, Nishikura K, Mizuno K, Takeuchi M, Sato Y, et al. Magnifying narrow-band imaging of surface maturation in early differentiated-type gastric cancers after Helicobacter pylori eradication. J Gastroenterol. 2013;48:1332–42.
Kitamura Y, Ito M, Matsuo T, Boda T, Oka S, Yoshihara M, et al. Characteristic epithelium with low-grade atypia appears on the surface of gastric cancer after successful Helicobacter pylori eradication therapy. Helicobacter. 2014;19:289–95.
Yagi K, Saka A, Nozawa Y, Nakamura A. Prediction of Helicobacter pylori status by conventional endoscopy, narrow-band imaging magnifying endoscopy in stomach after endoscopic resection of gastric cancer. Helicobacter. 2014;19:111–5.
Conflict of interest
The authors have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
A. Saka, K. Yagi and S. Nimura contributed equally to this study.
Rights and permissions
About this article
Cite this article
Saka, A., Yagi, K. & Nimura, S. Endoscopic and histological features of gastric cancers after successful Helicobacter pylori eradication therapy. Gastric Cancer 19, 524–530 (2016). https://doi.org/10.1007/s10120-015-0479-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-015-0479-y