Abstract
Background
Use of ultrasonically activated shears (UAS) is gaining popularity in open surgery but without concrete evidence. We conducted a prospectively randomized study to assess the efficacy of ultrasonic dissection in open gastrectomy for gastric cancer.
Methods
Patients with gastric cancer who were to undergo gastrectomy with D2 lymph node dissection were enrolled and assigned to either the conventional surgery group (n = 125) or the UAS group (n = 128).
Results
The mean operating time was significantly reduced in the UAS group (89.3 ± 15.6 min) when compared to the conventional group (97.8 ± 17.2 min; p < 0.001). However, we did not find any significant difference in operative blood loss, the amount of postoperative abdominal drainage, or the rate of postoperative complications between the groups. A multivariate analysis for operating time revealed that the use of UAS, female gender and BMI less than 25 were significantly associated with reduced operating time. The operating time was significantly longer in the conventional group than in the UAS group (B 7.786; 95 % CI 4.103–11.468; p < 0.001). In the subgroup analysis, the use of UAS significantly reduced the operating time, especially in male patients, regardless of the BMI status.
Conclusions
The use of UAS in gastrectomy for gastric cancer was a safe and efficient method, especially in terms of reducing operating time for male patients.
Similar content being viewed by others
Introduction
Gastric cancer is one of the most common malignancies worldwide and a major cause of cancer death in Korea [1]. The mainstay of treatment for gastric cancer has been complete surgical resection including lymph node dissection, which shows an excellent survival rate. In this regard, the standard operation for gastric cancer means subtotal or total gastrectomy according to the location of the tumor and at least D2 lymph node dissection [2].
Ultrasonically activated shears (UAS) were first introduced and widely used in laparoscopic surgery and robot-assisted surgery, and they are a quite useful surgical apparatus in the surgical field [3, 4]. This technique has recently been applied to open procedures. UAS has been proven to occlude small to medium-sized arteries and lymphatic vessels in several animal studies [5, 6], and UAS is reported to have several advantages over conventional electrosurgical instruments in terms of reduced operating times, less intraoperative blood loss and reduced leakage from the cut surface of organs in a variety of surgeries such as cholecystectomy, thyroidectomy, colorectal surgery, and pancreatic and hepatic resections [7–11].
In gastric cancer surgery, UAS is also gaining popularity not only in laparoscopic surgery and robotic surgery, but also in open gastrectomy for its safe, effective and efficient features, but without concrete evidence. There are few articles comparing the safety and efficacy of ultrasonic dissection with conventional surgery in gastrectomy. In an earlier, randomized study to determine the effectiveness of the UAS versus monopolar electrosurgery in D2 lymphatic dissection, the use of UAS was associated with reduced operative blood loss, postoperative drained fluid and hospital stay, but the operating time was not significantly different between the two groups [12]. However, the number of patients studied in the study was small and operative procedures were quite variable among the patients in the study, which made results less confirmative. Therefore, we conducted a prospectively randomized controlled study in a large number on patients with gastric cancer whose operations were performed by one surgeon and attempted to evaluate the efficacy of ultrasonic dissection by comparing it with conventional surgery.
Patients and methods
Study design and participants
Patients between the ages of 20 and 75 years with gastric cancer who were to undergo gastrectomy with D2 lymph node dissection were recruited from the Department of Surgery, Samsung Medical Center, between January 2010 and April 2011. Exclusion criteria were as follows: a history of malignancy or other chronic disorders such as coagulation impairment, liver disease, cardiovascular disease, etc., women during menstruation, anticoagulation medication before surgery and previous abdominal surgery. Evaluation of the eligibility of the patients to be included was performed by one of the authors (SJO). Informed written consent was obtained from all patients, and the study protocol was approved by the institutional review board of the Samsung Medical Center, Seoul, Korea. This trial was registered on ClinicalTrials.gov, no. NCT01179750.
Randomization and sample size
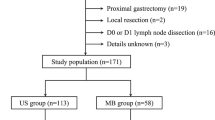
The patients were randomly assigned to the UAS or the conventional surgery group. We stratified patients according to gender, body mass index (BMI) and preoperative depth of tumor invasion (early or advanced gastric cancers based on endoscopic findings). Randomization lists were generated from an independent randomization group using a permuted block design of size four within each stratum. The assignment of each patient to one of the two surgery groups was shown to the surgeon at the time of surgery after the confirmation of inclusion. Figure 1 summarizes the study scheme. The primary end points of the study were operative blood loss and operating time. The secondary end points were postoperative lymphatic drainage and postoperative complications. Based on the previous operation data, we calculated the sample size by estimating a 20 % advantage of saving intraoperative blood loss and also operating time when using UAS. One hundred fifteen patients in each group were required to detect a difference in mean intraoperative blood loss of 184.5 ml, with an estimated SD of 99.7 ml, a power of 80 % and a 5 % risk of type 1 error. Fourteen patients in each group were required to detect a difference in mean operating time of 92.6 min, with an estimated SD of 17.1 min, a power of 80 % and a 5 % risk of type 1 error. We decided to randomize 128 patients per group considering an elimination rate of 10 %.
Procedures
All operations included subtotal or total gastrectomy with a standard D2 lymph node dissection and were performed by one surgeon (JMB) to minimize bias between operators due to using different surgical techniques to dissect the lymph node. In the UAS group, operations were performed using a Harmonic Scalpel (Ethicon Endosurgery, Inc., Cincinnati, OH, USA). The UAS was mainly applied to seal lymphatic and vascular vessels during procedures such as omentectomy, lymph node dissection and clearance of perigastric adipose tissues around the gastric wall. Major blood vessels such as the left and right gastric vessels and the left and right gastroepiploic vessels were ligated with a surgical tie and/or hemoclips. In the conventional group, a monopolar electric coagulator was used for tissue dissection, and hemoclips or surgical ties were applied for vessel ligation. Use of monopolar diathermy was allowed in both groups.
Operating time was checked only for the main gastrectomy procedure, namely from the opening of the peritoneal cavity to the extraction of the surgical specimen. We eliminated other time spent for procedures such as laparotomy, bowel reconstruction, wound closure, etc., to avoid possible bias. The operating time for those procedures can be quite variable depending on the patient status, type of anastomosis and the surgical experience of assistants. Operative blood loss was calculated by the sum of the suctioned blood during the operation and by the difference in the pre- and postoperative weight of the gauze. The weight of unused gauze was measured preoperatively, and all the used gauze was collected in a closed can immediately after being discarded. The weight of the used gauze was calculated carefully. Postoperative abdominal drainage was calculated by checking the daily amount of drained fluid from the day of operation to the day of drain removal. The drain was removed when the amount of drainage was <100 cc per day.
Statistical analysis
The data were statistically compared between the UAS and control groups using an independent sample t test for continuous variables and Chi-squared test or Fisher’s exact test for categorical data analysis. Multivariate analysis was carried out using a linear regression method. All statistical analyses were performed using the statistical software program PASW Statistics 18 (SPSS Inc., Somers, NY, USA). p <0.05 was considered significant.
Results
Two hundred fifty-six patients were randomized, 127 into the conventional group and 129 into the UAS group. Two patients in the conventional group and one in the UAS group were excluded from the study, leaving 125 patients in the conventional group and 128 patients in the UAS group for final analysis (Fig. 1).
The comparison of demographic features revealed no significant difference in the mean age, gender ratio, body mass index (BMI), type of operation, depth of tumor invasion, lymph node metastasis and tumor stages between the groups (Table 1).
In the analysis of surgical outcomes, the mean operating time was significantly reduced in the UAS group (89.3 ± 15.6 min) compared to the conventional group (97.8 ± 17.2 min; Table 2). However, we did not find any difference in intraoperative blood loss and the amount of postoperative abdominal drainage. The rates of postoperative complications such as postoperative bleeding, chylous drainage, pancreatitis and wound problems were not different between the groups. Both univariate and multivariate analysis revealed that the use of UAS, female gender and BMI <25 were significantly associated with reduced operating time (Tables 3, 4). The operative blood loss was significantly associated with gender, BMI and the type of operation; postoperative drainage was also significantly related to BMI, depth of tumor invasion and an advanced tumor stage in the univariate analysis (Table 3). In the subgroup analysis, the use of UAS significantly reduced the operating time compared to the conventional group especially in male patients, regardless of the BMI status (Table 5).
Discussion
UAS exploits mechanical energy to achieve hemostasis. It transfers high frequency to a vibrating blade that is used to grasp tissue against a non-vibrating pad, and the friction heat generated by ultrasonic vibration denatures the protein in the tissue to form a sticky coagulum that seals the vessel lumen. It is known that UAS can securely occlude not only arteries but also veins and lymphatic vessels, and it can therefore be used safely and effectively for lymph node dissection for malignant diseases in open procedures as well as laparoscopic surgery [6].
Operating time, the amount of operative blood loss and postoperative abdominal drainage are mainly dependent on surgical procedures and surgeon’s personal skills. Thus, operative results can be different among surgeons, and how carefully hemostasis and lymphatic sealing are carried out may be more important than surgical tools used. In this regard, the present study was conducted by only one expert surgeon who has performed thousands of gastrectomies to reduce possible difference in the operative procedure among the surgeons. However, it is also a limitation of the present study in that the outcome of using UAS could be different, especially in the hands of less expert surgeons.
It has been reported that BMI and gender can influence operating time and other surgical outcomes [13]. Also, tumor stage and lymph node metastasis can be associated with operating time and the amount of drainage after surgery. In this regard, a stratified randomization was performed in our study to make both groups uniform based on gender, BMI and preoperative tumor stage.
Contrary to the previous study that showed that the use of UAS in gastric cancer surgery could reduce operative blood loss and postoperative lymphorrhea but not operating time [12], the present study on a large scale showed that only operating time was significantly reduced in the UAS group compared to the conventional group. There was an approximately 10 % difference in the amount of operative blood loss between the groups, but it was not statistically significant in this study.
The operating time was also significantly shorter in females and those with lower BMI (<25 kg/m2) in the univariate analysis. The type of operation did not affect the operating time, possibly because the operating time was checked only for the main gastrectomy procedure, eliminating other time spent for laparotomy, reconstruction, wound closure, etc. The depth of tumor invasion, lymph node metastasis and tumor stage also did not affect the operating time. Generally, a large-sized tumor with extensive and grossly enlarged lymph node metastasis makes the operation more difficult, and it has been reported that for gastric cancers larger than 7 cm in diameter, the use of UAS could be beneficial in terms of shorter operating times and less intraoperative blood loss than standard electrosurgery [14].
In the multivariate analysis, the UAS group, being female and having lower BMI (<25 kg/m2) were independent factors for determining the operating time, and a subgroup analysis revealed that the use of UAS significantly reduced the operating time in male patients, regardless of the BMI status. In females, the use of UAS tended to reduce the operating time in both the high or low BMI group, but this was not statistically significant. It seems that some physical dissimilarity between the genders such as body shape, visceral and subcutaneous fat distribution, and abdominal wall distensibility might have affected the differences in operating times [13].
Our data suggest that the use of UAS could effectively shorten the operating time, possibly by reducing the use of many ligations with a surgical tie. It may seem that an approximatley 10–15-min difference is not so clinically significant; however, it represents a more than 10 % reduction in operating time for the main procedure and also implies clear benefits in terms of providing convenient and efficient procedures during surgery.
Another possible advantage of using UAS would be prevention of possible tumor cell spillage from the lymphovascular channels by more secure coagulation, especially in advanced-stage cancer. It has been reported that lymph node dissection might open lymphatic channels and spread viable free cancer cells into the peritoneal cavity [15, 16].
It is quite difficult to make any clear judgment regarding the cost-benefit issue of a UAS device at this time. The device is about $US 800 in our country and still not covered by public health insurance. The present study showed an approximately 9-min reduction in average operating time however; there could be other possible conveniences that we didn’t measure in the present study, so the matter is quite subjective and may lead to different responses from surgeons. The issue needs to be reassessed if the device is covered by health insurance in the future.
In conclusion, the use of UAS in gastrectomy for gastric cancer was a safe and efficient method, especially in terms of reducing the operating time for male patients.
References
Choi Y, Gwack J, Kim Y, et al. Long term trends and the future gastric cancer mortality in Korea: 1983–2013. Cancer Res Treat. 2006;38:7–12.
Sasako M, Sano T, Yamamoto S, et al. D2 lymphadenectomy alone or with para-aortic nodal dissection for gastric cancer. N Engl J Med. 2008;359:453–62.
Amaral JF. The experimental development of an ultrasonically activated scalpel for laparoscopic use. Surg Laparosc Endosc. 1994;4:92–9.
Amaral JF. Laparoscopic cholecystectomy in 200 consecutive patients using an ultrasonically activated scalpel. Surg Laparosc Endosc. 1995;5:255–62.
Kanehira E, Omura K, Kinoshita T, Kawakami K, Watanabe Y. How secure are the arteries occluded by a newly developed ultrasonically activated device? Surg Endosc. 1999;13:340–2.
Abe K, Terashima M, Fujiwara H, Takagane A, Uesugi N, Saito K. Experimental evaluation of bursting pressure in lymphatic vessels with ultrasonically activated shears. World J Surg. 2005;29:106–9.
Bessa SS, Abdel-Razek AH, Sharaan MA, Bassiouni AE, El-Khishen MA, El-Kayal el SA. Laparoscopic cholecystectomy in cirrhotic: a prospective randomized study comparing the conventional diathermy and the harmonic scalpel for gallbladder dissection. J Laparoendosc Adv Surg Tech A. 2011;21:1–5.
Hubner M, Demartines N, Muller S, Dindo D, Clavien PA, Hahnloser D. Prospective randomized study of monopolar scissors, bipolar vessel sealer and ultrasonic shears in laparoscopic colorectal surgery. Br J Surg. 2008;95:1098–104.
Voutilainen PE, Haglund CH. Ultrasonically activated shears in thyroidectomies: a randomized trial. Ann Surg. 2000;231:322–8.
Tanaka T, Matsugu Y, Fukuda Y. Use of ultrasonically activated shears improves the safety of pancreaticojejunostomy after pancreaticoduodenectomy. Arch Surg. 2002;137:1258–61.
Belli G, Limongelli P, Belli A, et al. Ultrasonically activated device for parenchymal division during open hepatectomy. HPB (Oxford). 2008;10:234–8.
Tsimoyiannis EC, Jabarin M, Tsimoyiannis JC, Betzios JP, Tsilikatis C, Glantzounis G. Ultrasonically activated shears in extended lymphadenectomy for gastric cancer. World J Surg. 2002;26:158–61.
Lee JH, Paik YH, Lee JS, et al. Abdominal shape of gastric cancer patients influences short-term surgical outcomes. Ann Surg Oncol. 2007;14:1288–94.
Mohri Y, Tonouchi H, Tanaka K, et al. Ultrasonically activated shears in gastrectomy for large gastric cancers. Surg Today. 2007;37:1060–3.
Marutsuka T, Shimada S, Shiomori K, et al. Mechanisms of peritoneal metastasis after operation for non-serosa-invasive gastric carcinoma: an ultrarapid detection system for intraperitoneal free cancer cells and a prophylactic strategy for peritoneal metastasis. Clin Cancer Res. 2003;9:678–85.
Kodera Y, Yamamura Y, Shimizu Y, et al. Peritoneal washing cytology: prognostic value of positive findings in patients with gastric carcinoma undergoing a potentially curative resection. J Surg Oncol. 1999;72:60–4 (discussion 4–5).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Choi, MG., Oh, S.J., Noh, J.H. et al. Ultrasonically activated shears versus electrocautery in open gastrectomy for gastric cancer: a randomized controlled trial. Gastric Cancer 17, 556–561 (2014). https://doi.org/10.1007/s10120-013-0301-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-013-0301-7