Abstract
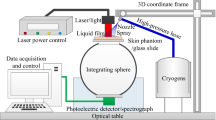
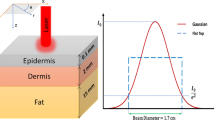
Laser lipolysis is a promising body contouring technology. However, the skin tissue could be thermally damaged owing to the laser energy absorption by water, which limits the lipolysis efficiency. To protect skin tissue and improve the lipolysis effect, cryogen spray cooling is introduced and synergized with the pulsed laser irradiation aiming to propose a new therapy protocol. By simulating heat conduction in the skin after spray cooling assisted laser lipolysis, the temperature distribution in the skin tissue was obtained to analyze the tissue damage by the Arrhenius integral. After parameter optimization according to the damage threshold of skin and adipose tissue, a new protocol with high laser intensity and short time was proposed including 150-ms R134a spray cooling with spray distance of 30 mm, and 100 ms 1064 nm laser irradiation with energy density of 20 J/cm2, with a relaxation for 9.75 s. This cycle of 10 s can be repeated 90 to 150 times for a total of 15 to 25 min. Compared with previous treatment procedure, new protocol can increase the fat dissolution depth from 2 to 4.5 mm beneath the dermis with same order laser fluence.










Similar content being viewed by others
References
Hales CM, Carroll MD, Fryar CD, et al (2020) Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS data brief, 2020(360):1–8. February 2020NCHS data brief
Jaacks LM, Vandevijvere S, Pan A et al (2019) The obesity transition: stages of the global epidemic. Lancet Diabetes Endocrinol 2019:231–240. https://doi.org/10.1016/S2213-8587(19)30026-9
Li TY, Rana JS, Manson J et al (2006) Obesity as compared with physical activity in predicting risk of coronary heart disease in women. Digest World Core Med J 113(4):499. https://doi.org/10.1161/CIRCULATIONAHA.105.574087
Kalantar ZK, Kopple JD (2006) Body mass index and risk for end-stage renal disease. Ann Intern Med 144(9):701. https://doi.org/10.7326/0003-4819-144-9-200605020-00021
Matjaz L, Zdenko V, Janez Z, et al (2009) QCW Pulsed Nd: YAG 1064 nm Laser Lipolysis[J]. J Laser Health Acad 2009:4–1. https://www.laserandhealthacademy.com/en/journal/?id=963&type=1
Neira R, Arroyave J, Ramirez H, Ortiz CL, Solarte E, Sequeda F, Gutierrez MI (2002) Fat liquefaction: effect of low-level laser energy on adipose tissue. Plast Reconstr Surg 110(3):912–922. https://doi.org/10.1097/00006534-200209010-00030
Goldman A (2006) Submental Nd: Yag laser-assisted liposuction. Laser Surg Med 38(3):181–184. https://doi.org/10.1002/lsm.20270
Pinar A, Theodore TN, Gaurav KG, Magesh S, Michael RH (2013) Low-level laser therapy for fat layer reduction: a comprehensive review. Laser Surg Med 45(6):349–357. https://doi.org/10.1002/lsm.22153
Dibernardo BE, Reyes J, Chen B (2009) Evaluation of tissue thermal effects from 1064/1320-nm laser-assisted lipolysis and its clinical implications. J Cosmet Laser Ther 11(2):62–69. https://doi.org/10.1080/14764170902792181
Anderson RR, Farinelli W, Laubach H et al (2010) Selective photothermolysis of lipid-rich tissues: a free electron laser study. Lasers Surg Med 38(10):913–919. https://doi.org/10.1002/lsm.20393
Wanner M, Avram M, Gagnon D, Mihm MC, Manstein D (2009) Effects of non-invasive, 1,210 nm laser exposure on adipose tissue: results of a human pilot study. Lasers Surg Med 41(6):401–407. https://doi.org/10.1002/lsm.20785
Decorato JW, Chen B, Sierra R (2017) Subcutaneous adipose tissue response to a non-invasive hyperthermic treatment using a 1,060 nm laser: adipose tissue response to noninvasive laser treatment. Lasers Surg Med 49(5):480. https://doi.org/10.1002/lsm.22625
Li D, Chen B, Wu W, He Y, Xing LZ, Wang G. Numerical analysis of cold injury of skin in cryogen spray cooling for laser dermatologic surgery. American Journal of Heat and Mass Transfer 2014(No.1):38-51.
Pennes HH (1948) Analysis of tissue and arterial blood temperature in resting forearm[J]. J Appl Phy 1(2):93–122. https://doi.org/10.1152/jappl.1948.1.2.93
Prahl SA, Keijzer M, Jacques SL, Welch AJ (1989) A Monte Carlo model of light propagation in tissue. Proceedings of SPIE—The International Society for Optical Engineering; 1989–01–01; Berlin, Germany. SPIE. p 102–111. (Proceedings of SPIE—The International Society for Optical Engineering)
Chen B, Zhang Y, Li D (2018) Numerical investigation of the thermal response to skin tissue during laser lipolysis. J THERM SCI 27(05):470–478. https://doi.org/10.1007/s11630-018-1042-z
Du Y, Hu XH, Cariveau M, Ma X, Kalmus GW, Lu JQ (2001) Optical properties of porcine skin dermis between 900 nm and 1500 nm. Phys Med Biol 46(1):167–181. https://doi.org/10.1088/0031-9155/46/1/312
Walfre F, Amogh et al (2010) Hyperthermic injury to adipocyte cells by selective heating of subcutaneous fat with a novel radiofrequency device: feasibility studies. Lasers Surg Med 42(5):361–370. https://doi.org/10.1002/lsm.20925
NA (1978) The American society for aesthetic plastic surgery. Ann Plas Surg 1(5):530. https://doi.org/10.1097/00000637-197809000-00024
Manstein D, Laubach H, Watanabe K, Farinelli W, Zurakowski D, Anderson RR (2008) Selective cryolysis: a novel method of non-invasive fat removal. Lasers Surg Med 40(9):595. https://doi.org/10.1002/lsm.20719
Mathew M, Avram et al (2009) CryolipolysisTM for subcutaneous fat layer reduction. Lasers Surg Med 41(10):703–708. https://doi.org/10.1002/lsm.20864
Tell EN (1979) Time progression of hemolysis of erythrocyte populations exposed to supraphysiological temperatures[J]. J Biomech Eng 101(3):213–217. https://doi.org/10.1115/1.3426247
Chen B, Thomsen SL, Thomas RJ, Oliver J, Welch AJ (2010) Histological and modeling study of skin thermal injury to 2.0 microm laser irradiation. Lasers Surg Med 40(5):358–370. https://doi.org/10.1002/lsm.20630
Li D (2013) Theoretical and experimental research on selective photothermalysis of biological tissue: [Ph.D. Thesis]. Xi'an Jiao Tong University, Xi’an
Wang L, Jacques SL, Zheng L (1995) MCML—Monte Carlo modeling of light transport in multi-layered tissues. Comput Meth Prog Bio 1995(No.2):131–146. https://doi.org/10.1007/978-1-4757-6092-7_4
Funding
National Natural Science Foundation of China (contract grant number: 52036007) and Fundamental Research Funds for the Central Universities.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yu, F., Xin, H., Chen, B. et al. New protocol for the R134a cryogen spray cooling assisted 1064-nm laser lipolysis. Lasers Med Sci 37, 2605–2614 (2022). https://doi.org/10.1007/s10103-022-03525-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-022-03525-z