Abstract
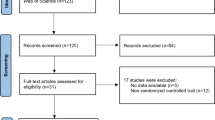
Melasma is a highly prevalent and cosmetically disfiguring pigmented skin disease. The post-treatment results are often unsatisfactory. A large number of clinical trials have tried to prove the effectiveness of the combination therapy involving laser therapy, but the results have been indeterminate. This study aimed to evaluate the effectiveness of laser treatment for melasma via a systematic review and meta-analysis. We respectively searched 4 databases and clinicaltrials.gov as of June 8, 2021. Two researchers independently searched for literature and extracted data. Study outcomes were computed by weighted mean differences (WMD). All statistical analyses were performed by the Review Manager version 5.3, STATA version 14 software at 95% confidence interval. We obtained 22 eligible studies which involved a total of 694 patients. After the heterogeneity test and sensitivity analysis, we took a subgroup meta-analysis on the before and after treatment of different laser types. We found that most lasers and laser-based combinations were associated with reduced melasma area and severity index (MASI), such as low-fluence Q-switch 1,064-nm Nd: YAG laser (QSNYL) (WMD: − 2.76; 95% CI: − 3.53 to − 1.99), fractional ablative CO2 laser (WMD: − 9.36; 95% CI: − 12.51 to − 6.21), and fractional ablative 2940-nm Er: YAG laser (WMD: − 2,72; 95% CI: − 3.94 to − 1.49). Significant decrease was seen in neither MASI score of non-ablative 1550-nm fractional laser (WMD: − 1.29; 95% CI: − 2.80 to 0.21) and picosecond laser (WMD: − 0.58; 95% CI: − 1.43 to 0.27), nor melanin index (MI) of low-fluence QSNYL treatment (WMD: 10.17; 95% CI: − 4.11 to 24.46). When using laser to treat melasma, various adverse reactions may occur, most of which will resolve quickly without subsequent treatment, such as edema, erythema, scaling, and burning sensation after treatment. However, for patients with darker skin, there are risks of postinflammatory hyperpigmentation and hypopigmentation. The laser and laser-based combination treatment for melasma could significantly reduce the MASI score, which was showed by our systematic review and meta-analysis.





Similar content being viewed by others
Data availability
The data supporting the findings of this study are available from the corresponding author on reasonable request.
References
Sheth VM, Pandya AG (2011) Melasma: a comprehensive update: part I. J Am Acad Dermatol 65(4):689–697
Ogbechie-Godec OA, Elbuluk N (2017) Melasma: an up-to-date comprehensive review. Dermatol Ther (Heidelb) 7(3):305–318
Gupta AK, Gover MD, Nouri K, Taylor S (2006) The treatment of melasma: a review of clinical trials. J Am Acad Dermatol 55(6):1048–1065
Nordlund JJ, Grimes PE, Ortonne JP (2006) The safety of hydroquinone. J Eur Acad Dermatol Venereol 20(7):781–787
Lee HC, Thng TG, Goh CL (2016) Oral tranexamic acid (TA) in the treatment of melasma: a retrospective analysis. J Am Acad Dermatol 75(2):385–392
Kumari R, Thappa DM (2010) Comparative study of trichloroacetic acid versus glycolic acid chemical peels in the treatment of melasma. Indian J Dermatol Venereol Leprol 76(4):447
Chalermchai T, Rummaneethorn P (2018) Effects of a fractional picosecond 1,064 nm laser for the treatment of dermal and mixed type melasma. J Cosmet Laser Ther 20(3):134–139
Wang YJ, Lin ET, Chen YT, Chiu PC, Lin BS, Chiang HM, Huang YH, Wang KY, Lin HY, Chang TM et al (2020) Prospective randomized controlled trial comparing treatment efficacy and tolerance of picosecond alexandrite laser with a diffractive lens array and triple combination cream in female Asian patients with melasma. J Eur Acad Dermatol Venereol 34(3):624–632
Manuskiatti W, Yan C, Tantrapornpong P, Cembrano KAG, Techapichetvanich T, Wanitphakdeedecha R (2020) A prospective, split-face, randomized study comparing a 755-nm picosecond laser with and without diffractive lens array in the treatment of melasma in Asians. Lasers Surg Med 53(1):95–103
Moubasher AE, Youssef EM, Abou-Taleb DA (2014) Q-switched Nd: YAG laser versus trichloroacetic acid peeling in the treatment of melasma among Egyptian patients. Dermatol Surg 40(8):874–882
Wattanakrai P, Mornchan R, Eimpunth S (2010) Low-fluence Q-switched neodymium-doped yttrium aluminum garnet (1,064 nm) laser for the treatment of facial melasma in Asians. Dermatol Surg 36(1):76–87
Vachiramon V, Sirithanabadeekul P, Sahawatwong S (2015) Low-fluence Q-switched Nd: YAG 1064-nm laser and intense pulsed light for the treatment of melasma. J Eur Acad Dermatol Venereol 29(7):1339–1346
Kim HS, Kim EK, Jung KE, Park YM, Kim HO, Lee JY (2013) A split-face comparison of low-fluence Q-switched Nd: YAG laser plus 1550 nm fractional photothermolysis vs. Q-switched Nd: YAG monotherapy for facial melasma in Asian skin. J Cosmet Laser Ther 15(3):143–149
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Bmj 339:b2535
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Bmj 343:d5928
Melsen WG, Bootsma MC, Rovers MM, Bonten MJ (2014) The effects of clinical and statistical heterogeneity on the predictive values of results from meta-analyses. Clin Microbiol Infect 20(2):123–129
Trelles MA, Velez M, Gold MH (2010) The treatment of melasma with topical creams alone, CO2 fractional ablative resurfacing alone, or a combination of the two: a comparative study. J Drugs Dermatol 9(4):315–322
Kroon MW, Wind BS, Beek JF, van der Veen JP, Nieuweboer-Krobotová L, Bos JD, Wolkerstorfer A (2011) Nonablative 1550-nm fractional laser therapy versus triple topical therapy for the treatment of melasma: a randomized controlled pilot study. J Am Acad Dermatol 64(3):516–523
Park KY, Kim DH, Kim HK, Li K, Seo SJ, Hong CK (2011) A randomized, observer-blinded, comparison of combined 1064-nm Q-switched neodymium-doped yttrium-aluminium-garnet laser plus 30% glycolic acid peel vs. laser monotherapy to treat melasma. Clin Exp Dermatol 36(8):864–870
Hong SP, Han SS, Choi SJ, Kim MS, Won CH, Lee MW, Choi JH, Moon KC, Kim YJ, Chang SE (2012) Split-face comparative study of 1550 nm fractional photothermolysis and trichloroacetic acid 15% chemical peeling for facial melasma in Asian skin. J Cosmet Laser Ther 14(2):81–86
Kar HK, Gupta L, Chauhan A (2012) A comparative study on efficacy of high and low fluence Q-switched Nd:YAG laser and glycolic acid peel in melasma. Indian J Dermatol Venereol Leprol 78(2):165–171
Shin JU, Park J, Oh SH, Lee JH (2013) Oral tranexamic acid enhances the efficacy of low-fluence 1064-nm quality-switched neodymium-doped yttrium aluminum garnet laser treatment for melasma in Koreans: a randomized, prospective trial. Dermatol Surg 39(3 Pt 1):435–442
Jalaly NY, Valizadeh N, Barikbin B, Yousefi M (2014) Low-power fractional CO2 laser versus low-fluence Q-switch 1,064 nm Nd: YAG laser for treatment of melasma: a randomized, controlled, split-face study. Am J Clin Dermatol 15(4):357–363
Lee DB, Suh HS, Choi YS (2014) A comparative study of low-fluence 1,064nm Q-Switched Nd: YAG laser with or without chemical peeling using Jessner’s solution in melasma patients. J Cosmet Laser Ther 16(6):264–270
Ustuner P, Balevi A, Ozdemir M (2017) A split-face, investigator-blinded comparative study on the efficacy and safety of Q-switched Nd:YAG laser plus microneedling with vitamin C versus Q-switched Nd:YAG laser for the treatment of recalcitrant melasma. J Cosmet Laser Ther 19(7):383–390
Kong SH, Suh HS, Choi YS (2018) Treatment of melasma with pulsed-dye laser and 1,064-nm Q-switched Nd: YAG laser: a split-face study. Ann Dermatol 30(1):1–7
Garg S, Vashisht KR, Makadia S (2019) A prospective randomized comparative study on 60 Indian patients of melasma, comparing pixel Q-switched NdYAG (1064 nm), super skin rejuvenation (540 nm) and ablative pixel erbium YAG (2940 nm) lasers, with a review of the literature. J Cosmet Laser Ther 21(5):297–307
Yun WJ, Moon HR, Lee MW, Choi JH, Chang SE (2014) Combination treatment of low-fluence 1,064-nm Q-switched Nd: YAG laser with novel intense pulse light in Korean melasma patients: a prospective, randomized, controlled trial. Dermatol Surg 40(8):842–850
Zamanian A, Behrangi E, Hossein Ghafarpour G, Mehran G, Espahbodi R, Hoseinzade Fakhim T, Azizian Z (2015) Effect of hydroquinone plus neodymium-doped yttrium aluminium garnet laser with and without CO2 fractional laser on resistant dermal melasma. J Skin Stem Cell 2(2). https://doi.org/10.17795/jssc30290
Dev T, Sreenivas V, Sharma VK, Sahni K, Bhari N, Sethuraman G (2020) A split face randomized controlled trial comparing 1,064 nm Q-switched Nd-YAG laser and modified Kligman’s formulation in patients with melasma in darker skin. Int J Dermatol 59(12):1525–1530
Qu Y, Wang F, Liu J, Xia X (2021) Clinical observation and dermoscopy evaluation of fractional CO(2) laser combined with topical tranexamic acid in melasma treatments. J Cosmet Dermatol 20(4):1110–1116
Badawi AM, Osman MA (2018) Fractional erbium-doped yttrium aluminum garnet laser-assisted drug delivery of hydroquinone in the treatment of melasma. Clin Cosmet Investig Dermatol 11:13–20
Laothaworn V, Juntongjin P (2018) Topical 3% tranexamic acid enhances the efficacy of 1064-nm Q-switched neodymium-doped yttrium aluminum garnet laser in the treatment of melasma. J Cosmet Laser Ther 20(6):320–325
Kaminaka C, Furukawa F, Yamamoto Y (2017) The clinical and histological effect of a low-fluence Q-switched 1,064-nm neodymium: yttrium-aluminum-garnet laser for the treatment of melasma and solar lentigenes in Asians: prospective, randomized, and split-face comparative study. Dermatol Surg 43(9):1120–1133
Polnikorn N (2008) Treatment of refractory dermal melasma with the MedLite C6 Q-switched Nd:YAG laser: two case reports. J Cosmet Laser Ther 10(3):167–173
Gokalp H, Akkaya AD, Oram Y (2016) Long-term results in low-fluence 1064-nm Q-Switched Nd:YAG laser for melasma: is it effective? J Cosmet Dermatol 15(4):420–426
Katz TM, Glaich AS, Goldberg LH, Firoz BF, Dai T, Friedman PM (2010) Treatment of melasma using fractional photothermolysis: a report of eight cases with long-term follow-up. Dermatol Surg 36(8):1273–1280
Rokhsar CK, Fitzpatrick RE (2005) The treatment of melasma with fractional photothermolysis: a pilot study. Dermatol Surg 31(12):1645–1650
Neeley MR, Pearce FB, Collawn SS (2010) Successful treatment of malar dermal melasma with a fractional ablative CO2 laser in a patient with type V skin. J Cosmet Laser Ther 12(6):258–260
Geronemus RG (2006) Fractional photothermolysis: current and future applications. Lasers Surg Med 38(3):169–176
Wu DC, Goldman MP, Wat H, Chan HHL (2021) A systematic review of picosecond laser in dermatology: evidence and recommendations. Lasers Surg Med 53(1):9–49
Choi YJ, Nam JH, Kim JY, Min JH, Park KY, Ko EJ, Kim BJ, Kim WS (2017) Efficacy and safety of a novel picosecond laser using combination of 1 064 and 595 nm on patients with melasma: a prospective, randomized, multicenter, split-face, 2% hydroquinone cream-controlled clinical trial. Lasers Surg Med 49(10):899–907
Lyons AB, Moy RL, Herrmann JL (2019) A randomized, controlled, split-face study of the efficacy of a picosecond laser in the treatment of melasma. J Drugs Dermatol 18(11):1104–1107
Acknowledgements
We would like to express our sincere gratitude to the Institute of Clinical Medical Sciences, China-Japan Friendship Hospital, Beijing, for help in revising the critical content of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Dihui Lai and Shaona Zhou were responsible for the material preparation, data collection, and analysis. The first draft of the manuscript was written by Dihui Lai. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lai, D., Zhou, S., Cheng, S. et al. Laser therapy in the treatment of melasma: a systematic review and meta-analysis. Lasers Med Sci 37, 2099–2110 (2022). https://doi.org/10.1007/s10103-022-03514-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-022-03514-2