Abstract
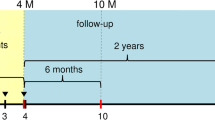
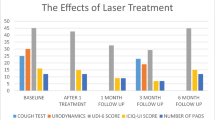
Stress urinary incontinence (SUI) is a common health problem that affects roughly 35% of women in the reproductive period. A prospective uncontrolled study was conducted to assess the long-term efficacy and safety of a non-ablative Er:YAG laser treatment of SUI. Forty-three patients participated in the study. All women underwent three sessions of IncontiLase® procedure, and efficacy of laser treatment was assessed by 1-h pad test, 24-h pad test, 3-day voiding diary, and ICIQ-UI SF questionnaire at multiple follow-ups. Statistical analysis was performed using one-way repeated measures ANOVA. Patients were questioned about discomfort during treatment and any adverse events following the laser procedures. All outcome measures showed a significant change over a period of the entire clinical trial. Eighteen-month follow-up revealed a fading of the effect, which was alleviated by single-session maintenance treatments every 6 months. There were no serious adverse events reported during the study. All reported side effects were mild and transient. The application of non-ablative Er:YAG laser for SUI treatment significantly improves the SUI symptoms. High improvement rates and patient satisfaction can be maintained with single-session maintenance treatments performed every 6 months. Long-term safety profile of multiple non-ablative Er:YAG laser treatment is shown. NCT04348994, 16.04.2020, retrospectively registered.


Similar content being viewed by others
References
Van Kerrebroeck PEV, ed. ICS Standards 2022. 2020th ed. ICS; 2022.
MacLennan AH, Taylor AW, Wilson DHD, Wilson DHD (2000) The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. BJOG An Int J Obstet Gynaecol 107(12):1460–1470. https://doi.org/10.1111/j.1471-0528.2000.tb11669.x
Holroyd-Leduc JM, Straus SE (2004) Management of urinary incontinence in women. JAMA 291(8):986. https://doi.org/10.1001/jama.291.8.986
Rovner ES, Wein AJ. Treatment options for stress urinary incontinence. Rev Urol. 2004;6 Suppl 3(Table 1):S29–47. doi:https://doi.org/10.1002/nau
Dumoulin C, Hay-Smith EJC, Mac H-Séguin G (2014) Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane database Syst Rev 5(5):119. https://doi.org/10.1002/14651858.CD005654.pub3
Shamout S, Campeau L (2017) Stress urinary incontinence in women: current and emerging therapeutic options. Can Urol Assoc J 11(6):S155–S158. https://doi.org/10.5489/cuaj.4613
Chapple CR, Raz S, Brubaker L, Zimmern PE (2013) Mesh sling in an era of uncertainty: lessons learned and the way forward. Eur Urol 64(4):525–529. https://doi.org/10.1016/j.eururo.2013.06.045
Nilsson CG (2015) Creating a gold standard surgical procedure: the development and implementation of TVT. Int Urogynecol J Pelvic Floor Dysfunct 26(4):467–469. https://doi.org/10.1007/s00192-014-2616-2
El-Domyati M, Abd-El-Raheem T, Medhat W, Abdel-Wahab H, Anwer M Al. Multiple fractional erbium: yttrium–aluminum–garnet laser sessions for upper facial rejuvenation: clinical and histological implications and expectations. J Cosmet Dermatol. 2014;13(1):30–37. https://doi.org/10.1111/jocd.12079
Vizintin Z, Rivera M, Fistonić I et al (2012) Novel minimally invasive VSP Er:YAG laser treatments in gynecology. J Laser Heal Acad 2012(1):46–58
Lapii GAA, Yakovleva AYY, Neimark AII (2017) Structural reorganization of the vaginal mucosa in stress urinary incontinence under conditions of Er:YAG laser treatment. Bull Exp Biol Med 162(4):510–514. https://doi.org/10.1007/s10517-017-3650-0
Rechberger T, Postawski K, Jakowicki JA, Gunja-Smith Z, Woessner JF Jr (2016) Role of fascial collagen in stress urinary incontinence. Am J Obstet Gynecol 179(6):1511–1514. https://doi.org/10.1016/S0002-9378(98)70017-1
Lin KL, Chou SH, Long CY. Effect of er:yag laser for women with stress urinary incontinence. Biomed Res Int. 2019;2019. doi:https://doi.org/10.1155/2019/7915813
Majaron B, Kelly KM, Park HB, Verkruysse W, Nelson JS (2001) Er:YAG laser skin resurfacing using repetitive long-pulse exposure and cryogen spray cooling: I. Histological study. Lasers Surg Med. 28(2):121–130. https://doi.org/10.1002/lsm.1026
Drnovšek-Olup B, Beltram M, Pižem J et al (2004) Repetitive Er:YAG laser irradiation of human skin: a histological evaluation. Lasers Surg Med 35(2):146–151. https://doi.org/10.1002/lsm.20080
Lapii GA, Yakovleva AY, Neimark AI, Lushnikova EL (2017) Study of proliferative activity of vaginal epithelium in women with stress urinary incontinence treated by Er:YAG laser. Bull Exp Biol Med. 1–4. https://doi.org/10.1007/s10517-017-3784-0
Ghoniem G, Stanford E, Kenton K et al (2008) Evaluation and outcome measures in the treatment of female urinary stress incontinence: International Urogynecological Association (IUGA) guidelines for research and clinical practice. Int Urogynecol J Pelvic Floor Dysfunct 19(1):5–33. https://doi.org/10.1007/s00192-007-0495-5
FDA. Guidance for Industry and Food and Drug Administration Staff: Clinical Investigations of Devices Indicated for the Treatment of Urinary Incontinence.; 2011. http://www.fda.gov/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/ucm07. Accessed March 7, 2018.
Blaganje M, Šćepanović D, Žgur L, Verdenik I, Pajk F, Lukanović A (2018) Non-ablative Er:YAG laser therapy effect on stress urinary incontinence related to quality of life and sexual function: a randomized controlled trial. Eur J Obstet Gynecol Reprod Biol 224:153–158. https://doi.org/10.1016/j.ejogrb.2018.03.038
Bizjak-Ogrinc U, Senčar S, Lenasi H et al (2015) Novel minimally invasive laser treatment of urinary incontinence in women. Lasers Surg Med 47(9):689–697. https://doi.org/10.1002/lsm.22416
Pardo JI, Solà VR, Morales AA (2016) Treatment of female stress urinary incontinence with Erbium-YAG laser in non-ablative mode. Eur J Obstet Gynecol Reprod Biol 204:1–4. https://doi.org/10.1016/j.ejogrb.2016.06.031
Tien YW, Hsiao SM, Lee CN, Lin HH (2017) Effects of laser procedure for female urodynamic stress incontinence on pad weight, urodynamics, and sexual function. Int Urogynecol J Pelvic Floor Dysfunct 28(3):469–476. https://doi.org/10.1007/s00192-016-3129-y
Fistonic N, Fistonic I, Lukanovic A, et al. First assessment of short-term efficacy of Er:YAG laser treatment on stress urinary incontinence in women: prospective cohort study. Climacteric. 2015;18 Suppl 1(sup1):37–42. doi:https://doi.org/10.3109/13697137.2015.1071126
Fistonic N, Fistonic I, Gustek SF et al (2016) Minimally invasive, non-ablative Er:YAG laser treatment of stress urinary incontinence in women–a pilot study. Lasers Med Sci 31(4):635–643. https://doi.org/10.1007/s10103-016-1884-0
Kuszka A, Gamper M, Walser C, Kociszewski J, Viereck V. Erbium:YAG laser treatment of female stress urinary incontinence: midterm data. Int Urogynecol J. December 2019. https://doi.org/10.1007/s00192-019-04148-9
Gaviria JP, Korosec B, Fernandez J et al (2016) Up to 3-year follow-up of patients with vaginal relaxation syndrome participating in laser vaginal tightening. J Laser Heal Acad 2016(May):1–6
González Isaza P, Jaguszewska K, Cardona JL, Lukaszuk M. Long-term effect of thermoablative fractional CO2 laser treatment as a novel approach to urinary incontinence management in women with genitourinary syndrome of menopause. Int Urogynecol J. May 2017. https://doi.org/10.1007/s00192-017-3352-1
Hardy LA, Chang C-H, Myers EM, Kennelly MJ, Fried NM. Laser treatment of female stress urinary incontinence: optical, thermal, and tissue damage simulations. In: Choi B, Kollias N, Zeng H, et al., eds.; 2016:96891R. https://doi.org/10.1117/12.2208126
Karcher C, Sadick N (2016) Vaginal rejuvenation using energy-based devices. Int J Women’s Dermatology 2(3):85–88. https://doi.org/10.1016/j.ijwd.2016.05.003
Okui N (2019) Comparison between erbium-doped yttrium aluminum garnet laser therapy and sling procedures in the treatment of stress and mixed urinary incontinence. World J Urol 37(5):885–889. https://doi.org/10.1007/s00345-018-2445-x
FDA warns against use of energy-based devices to perform vaginal “rejuvenation” or vaginal cosmetic procedures: FDA Safety Communication | FDA. https://www.fda.gov/medical-devices/safety-communications/fda-warns-against-use-energy-based-devices-perform-vaginal-rejuvenation-or-vaginal-cosmetic. Published 2018. Accessed December 13, 2019.
Gambacciani M, Cervigni M, Gaspar A et al (2020) Safety of Vaginal Erbium Laser (VELTM): a review of 113,000 patients treated in the past eight years. Climacteric 23(sup1):S28–S32. https://doi.org/10.1080/13697137.2020.1813098
Author information
Authors and Affiliations
Contributions
H Brandi—study management and data collection.
A Gaspar—protocol development, study management, data collection, data analysis, and manuscript writing.
N Koron—manuscript writing.
J Silva—data collection.
Corresponding author
Ethics declarations
Ethics approval
Study was approved by the Ethics Review Board of the Uroclinica.
Conflict of interest
A. Gaspar has received honoraria from the manufacturer of the medical device used in this study, for speaking at symposia. N. Koron is an employee of the manufacturer of the device used in this study. Other authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gaspar, A., Koron, N., Silva, J. et al. Vaginal erbium laser for treatment of stress urinary incontinence: optimization of treatment regimen for a sustained long-term effect. Lasers Med Sci 37, 2157–2164 (2022). https://doi.org/10.1007/s10103-021-03474-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-021-03474-z