Abstract
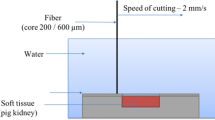
The goal of this study was to assess the ablation, coagulation, and carbonization characteristics of the holmium:YAG (Ho:YAG) laser and thulium fiber lasers (TFL). The Ho:YAG laser (100 W av.power), the quasi-continuous (QCW) TFL (120 W av.power), and the SuperPulsed (SP) TFL (50 W av.power) were compared on a non-frozen porcine kidney. To control the cutting speed (2 or 5 mm/s), an XY translation stage was used. The Ho:YAG was tested using E = 1.5 J and Pav = 40 W or Pav = 70 W settings. The TFL was tested using E = 1.5 J and Pav = 30 W or Pav = 60 W settings. After ex vivo incision, histological analysis was performed in order to estimate thermal damage. At 40 W, the Ho:YAG displayed a shallower cutting at 2 and 5 mm/s (1.1 ± 0.2 mm and 0.5 ± 0.2 mm, respectively) with virtually zero coagulation. While at 70 W, the minimal coagulation depth measured 0.1 ± 0.1 mm. The incisions demonstrated zero carbonization. Both the QCW and SP TFL did show effective cutting at all speeds (2.1 ± 0.2 mm and 1.3 ± 0.2 mm, respectively, at 30 W) with prominent coagulation (0.6 ± 0.1 mm and 0.4 ± 0.1 mm, respectively, at 70 W) and carbonization. Our study introduced the TFL as a novel efficient alternative for soft tissue surgery to the Ho:YAG laser. The SP TFL offers a Ho:YAG-like incision, while QCW TFL allows for fast, deep, and precise cutting with increased carbonization.
Similar content being viewed by others
Data availability
On demand.
References
Parsons RL, Campbell JL, Thomley MW (1968) Carcinoma of the penis treated by the ruby laser. J Urol 100(1):38–39
Bruskewitz RC (2003) Quality of life and sexual function in patients with benign prostatic hyperplasia. Rev Urol 5(2):72–80
Rieken M, Bachmann A (2014) Laser treatment of benign prostate enlargement--which laser for which prostate? Nat Rev Urol 11(3):142–152
Kyriazis I, Swiniarski PP, Jutzi S, Wolters M, Netsch C, Burchardt M et al (2015) Transurethral anatomical enucleation of the prostate with Tm:YAG support (ThuLEP): review of the literature on a novel surgical approach in the management of benign prostatic enlargement. World J Urol 33(4):525–530
Li K, Xu Y, Tan M, Xia S, Xu Z, Xu D (2019) A retrospective comparison of thulium laser en bloc resection of bladder tumor and plasmakinetic transurethral resection of bladder tumor in primary non-muscle invasive bladder cancer. Lasers Med Sci 34(1):85–92
Fried NM, Murray KE (2005) High-power thulium fiber laser ablation of urinary tissues at 1.94 microm. J Endourol 19(1):25–31
Enikeev D, Glybochko P, Rapoport L, Gahan J, Gazimiev M, Spivak L et al (2018) A randomized trial comparing the learning curve of three endoscopic enucleation techniques (HoLEP, ThuFLEP and MEP) for BPH using mentoring approach - initial results. Urology 121:51
Bach T, Huck N, Wezel F, Hacker A, Gross AJ, Michel MS (2010) 70 vs 120 W thulium:yttrium-aluminium-garnet 2 microm continuous-wave laser for the treatment of benign prostatic hyperplasia: a systematic ex-vivo evaluation. BJU Int 106(3):368–372. https://doi.org/10.1111/j.1464-410X.2009.09059.x
Enikeev D, Glybochko P, Okhunov Z, Alyaev Y, Rapoport L, Tsarichenko D et al (2018) Retrospective analysis of short-term outcomes after monopolar versus laser endoscopic enucleation of the prostate: a single center experience. J Endourol 32(5):417–423
Cooper TE, Trezek GJ (1972) A probe technique for determining the thermal conductivity of tissue. J Heat Transf 94:133–140
Patch SK, Rao N, Kelly H, Jacobsohn K, See WA (2011) Specific heat capacity of freshly excised prostate specimens. Physiol Meas 32(11):N55–N64
Giering K, Lamprecht I, Minet O (1995) Determination of the specific heat capacity of healthy and tumorous human tissue. Thermochim Acta 251:199–205
Fischer AH, Jacobson KA, Rose J, Zeller R. Hematoxylin and eosin staining of tissue and cell sections. CSH protocols. 2008;2008:pdb prot4986
Peavy GM (2002) Lasers and laser-tissue interaction. Vet Clin North Am Small Anim Pract 32(3):517–534 v-vi
Fried NM (2006) Therapeutic applications of lasers in urology: an update. Exp Rev Med Dev 3(1):81–94
Shah HN, Mahajan AP, Sodha HS, Hegde S, Mohile PD, Bansal MB (2007) Prospective evaluation of the learning curve for holmium laser enucleation of the prostate. J Urol 177(4):1468–1474
Netsch C, Bach T, Herrmann TR, Neubauer O, Gross AJ (2013) Evaluation of the learning curve for thulium vapoenucleation of the prostate (ThuVEP) using a mentor-based approach. World J Urol 31(5):1231–1238
Kuntz RM (2006) Current role of lasers in the treatment of benign prostatic hyperplasia (BPH). Eur Urol 49(6):961–969
Jung GI, Kim JS, Lee TH, Choi JH, Oh HB, Kim AH et al (2015) Photomechanical effect on type I collagen using pulsed diode laser. Technol Health Care 23(Suppl 2):S535–S541
Andreeva V, Vinarov A, Yaroslavsky I, Kovalenko A, Vybornov A, Rapoport L et al (2019) Preclinical comparison of superpulse thulium fiber laser and a holmium:YAG laser for lithotripsy. World J Urol 38:497
Kuntz RM (2007) Laser treatment of benign prostatic hyperplasia. World J Urol 25(3):241–247
Teichmann HO, Herrmann TR, Bach T (2007) Technical aspects of lasers in urology. World J Urol 25(3):221–225
Enikeev D, Glybochko P, Rapoport L, Gahan J, Gazimiev M, Spivak L et al (2018) A randomized trial comparing the learning curve of 3 endoscopic enucleation techniques (HoLEP, ThuFLEP, and MEP) for BPH using mentoring approach-initial results. Urology. 121:51–57
Enikeev D, Taratkin M, Klimov R, et al. Superpulsed thulium fiber laser for stone dusting: in search of a perfect ablation regimen-a prospective single-center study. J Endourol. 2020;https://doi.org/10.1089/end.2020.0519. [published online ahead of print, 2020 Jul 15]
Enikeev D, Taratkin M, Klimov R, et al. Thulium-fiber laser for lithotripsy: first clinical experience in percutaneous nephrolithotomy. World J Urol. 2020;https://doi.org/10.1007/s00345-020-03134-x. [published online ahead of print, 2020 Feb 27]
Taratkin M, Laukhtina E, Singla N, et al. How lasers ablate stones: in vitro study of laser lithotripsy (Ho:YAG and Tm-fiber lasers) in different environments [published online ahead of print, 2020 Jan 29]. J Endourol. 2020;https://doi.org/10.1089/end.2019.0441. doi:https://doi.org/10.1089/end.2019.0441
Fried NM (2018) Recent advances in infrared laser lithotripsy [Invited]. Biomed Opt Express 9(9):4552–4568. https://doi.org/10.1364/BOE.9.004552 Published 2018 Aug 30
Large T, Nottingham C, Stoughton C, Williams J Jr, Krambeck A (2020) Comparative study of holmium laser enucleation of the prostate with MOSES enabled pulsed laser modulation. Urology. 136:196–201. https://doi.org/10.1016/j.urology.2019.11.029
Enikeev D, Shariat SF, Taratkin M, Glybochko P (2020) The changing role of lasers in urologic surgery. Curr Opin Urol 30(1):24–29. https://doi.org/10.1097/MOU.0000000000000695
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
No ethics approval is necessary for this type of work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(PDF 259 kb)
Rights and permissions
About this article
Cite this article
Taratkin, M., Kovalenko, A., Laukhtina, E. et al. Ex vivo study of Ho:YAG and thulium fiber lasers for soft tissue surgery: which laser for which case?. Lasers Med Sci 37, 149–154 (2022). https://doi.org/10.1007/s10103-020-03189-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-020-03189-7