Abstract
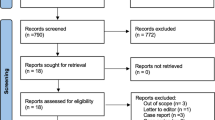
Antimicrobial photodynamic therapy (aPDT) is a complementary therapeutic modality for periodontal and endodontic diseases, in which Gram-negative bacteria are directly involved. Currently, there are few evidences regarding the effects of aPDT on bacterial components such as lipopolysaccharide (LPS) and it would represent a major step forward in the clinical use of this therapy. In this context, this study aimed to evaluate the efficacy of different photosensitizers (PSs) used in aPDT in LPS inhibition. Four PSs were used in this study: methylene blue (MB), toluidine blue (TBO), new methylene blue (NMB), and curcumin (CUR). Different approaches to evaluate LPS interaction with PSs were used, such as spectrophotometry, Limulus amebocyte lysate (LAL) test, functional assays using mouse macrophages, and an in vivo model of LPS injection. Spectrophotometry showed that LPS decreased the absorbance of all PSs used, indicating interactions between the two species. LAL assay revealed significant differences in LPS concentrations upon pre-incubation with the different PSs. Interestingly, the inflammatory potential of LPS decreased after previous treatment with the four PSs, resulting in decreased secretion of inflammatory cytokines by macrophages. In vivo, pre-incubating curcumin with LPS prevented animals from undergoing septic shock within the established time. Using relevant models to study the inflammatory activity of LPS, we found that all PSs used in this work decreased LPS-induced inflammation, with a more striking effect observed for NMB and curcumin. These data advance the understanding of the mechanisms of LPS inhibition by PSs.





Similar content being viewed by others
References
Pitts DL, Williams BL, Morton TH (1982) Investigation of the role of endotoxin in periapical inflammation. J Endod 8:10–18. https://doi.org/10.1016/S0099-2399(82)80310-5
Hong CY, Lin SK, Kok SH et al (2004) The role of lipopolysaccharide in infectious bone resorption of periapical lesion. J Oral Pathol Med 33(3):162–169. https://doi.org/10.1111/j.0904-2512.2004.00045.x
Silva TA, Garlet GP, Fukada SY et al (2007) Chemokines in oral inflammatory diseases: apical periodontitis and periodontal disease. J Dent Res 86(4):306–319. https://doi.org/10.1177/154405910708600403
Martinho FC, de Rabello DGD, Ferreira LL, Nascimento GG (2017) Participation of endotoxin in root canal infections: a systematic review and meta-analysis. Eur J Dent 11(3):398–406. https://doi.org/10.4103/ejd.ejd
Aquino-Martinez R, Rowsey JL, Fraser DG et al (2020) LPS-induced premature osteocyte senescence: implications in inflammatory alveolar bone loss and periodontal disease pathogenesis. Bone 132:115220. https://doi.org/10.1016/j.bone.2019.115220
Jain S, Darveau R (2011) Contribution of Porphyromonas gingivalis lipopolysaccharide to periodontitis. Periodontal 2000 54(1):53–70. https://doi.org/10.1111/j.1600-0757.2009.00333.x
Strachan A, Harrington Z, McIlwaine C et al (2019) Subgingival lipid A profile and endotoxin activity in periodontal health and disease. 23(9):3527–3534. https://doi.org/10.1007/s00784-018-2771-9
Lucisano MP, Nelson-Filho P, da Silva RAB et al (2014) Role of endotoxin in the etiology of periapical lesions: molecular mechanisms involved in endotoxin’s recognition and cell activation. RGO (Porto Alegre) 62(3):289–298. https://doi.org/10.1590/1981-8637201400030000092561
Nair P (2004) Pathogenesis of apical periodontitis and the causes of endodontic failures. Crit Rev Oral Biol Med 15(6):348–381. https://doi.org/10.1177/154411130401500604
Nelson-Filho P, Leonardo MR, Silva LA, Assed S (2002) Radiographic evaluation of the effect of endotoxin (LPS) plus calcium hydroxide on apical and periapical tissues of dogs. J Endod 28(10):694–696. https://doi.org/10.1097/00004770-200210000-00004
Leonardo MR, da Silva RAB, Assed S, Nelson-Filho P (2004) Importance of bacterial endotoxin (LPS) in endodontics. J Appl Oral Sci 12(2):93–98 S1678–77572004000200002
Paque F, Laib A, Gautschi H et al (2009) Hard-tissue debris accumulation analysis by high-resolution computed tomography scans. J Endod 35(7):1044–1047. https://doi.org/10.1016/j.joen.2009.04.026
Siqueira-Júnior J (2005) Reaction of periradicular tissues to root canal treatment: benefits and drawbacks. Endod Top 10(1):123–147. https://doi.org/10.1111/j.1601-1546.2005.00134.x
Chávez de Paz LE, Bergenholtz G, Svensäter G (2010) The effects of antimicrobials on endodontic biofilm bacteria. J Endod 36(1):70–77. https://doi.org/10.1016/j.joen.2009.09.017
Hwang TJ, Gibbs KA, Podolsky SH, Linder JA (2015) Antimicrobial stewardship and public knowledge of antibiotics. The Lancet Inf Dis 15(9):1000–1001. https://doi.org/10.1016/S1473-3099(15)00235-2
Laxminarayan R, Matsoso P, Pant S et al (2016) Access to effective antimicrobials: a worldwide challenge. Lancet 387(10014):168–175. https://doi.org/10.1016/S0140-6736(15)00474-2
Wong DTS, Cheung GSP (2014) Extension of bactericidal effect of sodium hypochlorite into dentinal tubules. J Endod 40(6):825–829. https://doi.org/10.1016/j.joen.2013.09.045
Ahmed HMA, Versiani MA, Dummer PMH (2017) A new system for classifying root and root canal morphology. Int Endod J 50(8):761–770. https://doi.org/10.1111/iej.12685
Safavi KE, Nichols FC (1994) Alteration of biological properties of bacterial lipopolysaccharide by calcium hydroxide treatment. J Endod 20(3):127–129. https://doi.org/10.1016/S0099-2399(06)80057-9
Paula-Silva FWG, Ghosh A, Arzate H et al (2010) Calcium hydroxide promotes cementogenesis and induces cementoblastic differentiation of mesenchymal periodontal ligament cells in a CEMP1- and ERK-dependent manner. Calcif Tissue Int 87(2):144–157. https://doi.org/10.1007/s00223-010-9368-x
Mohammadi Z, Shalavi S, Yazdizadeh M (2012) Antimicrobial activity of calcium hydroxide in endodontics: a review. Chonnam Med J 48(3):133–140. https://doi.org/10.4068/cmj.2012.48.3.133
Marinho ACS, To TT, Darveau RP, Gomes BPFA (2018) Detection and function of lipopolysaccharide and its purified lipid A after treatment with auxiliary chemical substances and calcium hydroxide dressings used in root canal treatment. Int Endod J 51(10):1118–1129. https://doi.org/10.1111/iej.12920
Garcez AS, Arantes-Neto JG, Sellera DP, Fregnani ER (2015) Effects of antimicrobial photodynamic therapy and surgical endodontic treatment on the bacterial load reduction and periapical lesion healing. Three years follow up. Photodiagn Photodyn Ther 12(4):575–580. https://doi.org/10.1016/j.pdpdt.2015.06.002
Tennert C, Drews AM, Walther V et al (2015) Ultrasonic activation and chemical modification of photosensitizers enhances the effects of photodynamic therapy against Enterococcus faecalis root-canal isolates. Photodiagn Photodyn Ther 12(2):244–251. https://doi.org/10.1016/j.pdpdt.2015.02.002
Chiniforush N, Pourhajibagher M, Shahabi S et al (2016) Can antimicrobial photodynamic therapy (aPDT) enhance the endodontic treatment? J Lasers Med Sci 7(2):76–85. https://doi.org/10.15171/jlms.2016.14
Nuernberg MAA, Miessi DMJ, Ivanaga CA et al (2019) Influence of antimicrobial photodynamic therapy as an adjunctive to scaling and root planing on alveolar bone loss: a systematic review and meta-analysis of animal studies. Photodiagn Photodyn Ther 25:354–363. https://doi.org/10.1016/j.pdpdt.2019.01.020
Chrepa V, Kotsakis GA, Pagonis TC, Hargreaves KM (2014) The effect of photodynamic therapy in root canal disinfection: a systematic review. J Endod 40(7):891–898. https://doi.org/10.1016/j.joen.2014.03.005
Hamblin M (2016) Antimicrobial photodynamic inactivation: a bright new technique to kill resistant microbes. Curr Opin Microbiol 33:67–73. https://doi.org/10.1016/j.mib.2016.06.008
Ramos UD, Ayub LG, Reino DM et al (2016) Antimicrobial photodynamic therapy as an alternative to systemic antibiotics: results from a double-blind, randomized, placebo-controlled, clinical study on type 2 diabetics. J Clin Periodontol 43(2):147–155. https://doi.org/10.1111/jcpe.12498
de Oliveira RR, Schwartz-Filho HO, Novaes AB Jr (2007) Antimicrobial photodynamic therapy in the non-surgical treatment of aggressive periodontitis: a preliminary randomized controlled clinical study. J Periodontol 78(6):965–973. https://doi.org/10.1902/jop.2007.060494
Silva LA, Novaes AB Jr, de Oliveira RR et al (2012) Antimicrobial photodynamic therapy for the treatment of teeth with apical periodontitis: a histopathological evaluation. J Endod 38(3):360–366. https://doi.org/10.1016/j.joen.2011.12.023
Fumes AC, da Silva Telles PD, Corona SAM, Borsatto MC (2018) Effect of aPDT on Streptococcus mutans and Candida albicans present in the dental biofilm: systematic review. Photodiagn Photodyn Ther 21:363–366. https://doi.org/10.1016/j.pdpdt.2018.01.013
Weishaupt KR, Gomer CJ, Dougherty TJ (1976) Identification of singlet oxygen as the cytotoxic agent in photo-inactivation of a murine tumor. Cancer Res 36(7):2326–2329
Wainwright M (1998) Photodynamic antimicrobial chemotherapy (PACT). J Antimicrob Chemother 42(1):13–28. https://doi.org/10.1093/jac/42.1.13
Kikuchi T, Mogi M, Okabe I et al (2015) Adjunctive application of antimicrobial photodynamic therapy in nonsurgical periodontal treatment: a review of literature. Int J Mol Sci 16(10):24111–24126. https://doi.org/10.3390/ijms161024111
Banerjee SM, MacRobert AJ, Mosse CA et al (2017) Photodynamic therapy: inception to application in breast cancer. Breast 31:105–113. https://doi.org/10.1016/j.breast.2016.09.016
Kwiatkowski S, Knap B, Przystupski D et al (2018) Biomedicine & Pharmacotherapy Photodynamic therapy – mechanisms , photosensitizers and combinations. 106:1098–1107. https://doi.org/10.1016/j.biopha.2018.07.049
Garcia VG, Longo M, Gualberto Junior EC et al (2014) Effect of the concentration of phenothiazine photosensitizers in antimicrobial photodynamic therapy on bone loss and the immune inflammatory response of induced periodontitis in rats. J Periodontol Res 49(5):584–594. https://doi.org/10.1111/jre.12138
Trindade AC, Figueiredo JAP, Steier L, Weber JBB (2015) Photodynamic therapy in endodontics: a literature review. Photomed Laser Surg 33(3):175–182. https://doi.org/10.1089/pho.2014.3776
Wilson M, Dobson J, Harvey W (1992) Sensitization of oral bacteria to killing by low-power laser radiation. Curr Microbiol 25(2):77–81. https://doi.org/10.1016/0003-9969(92)90058-g
Cieplik F, Tabenski L, Buchalla W et al (2014) Antimicrobial photodynamic therapy for inactivation of biofilms formed by oral key pathogens. 5:1–17. https://doi.org/10.3389/fmicb.2014.00405
Figueiredo RA, Anami LC, Mello I et al (2014) Tooth discoloration induced by endodontic phenothiazine dyes in photodynamic therapy. Photomed Laser Surg 32(8):1–5. https://doi.org/10.1089/pho.2014.3722
Costa LM, Matos FS, Correia AMO et al (2016) Tooth color change caused by photosensitizers after photodynamic therapy: an in vitro study. J Photochem Photobiol 160:225–228. https://doi.org/10.1016/j.jphotobiol.2016.04.019
Hatcher H, Planalp R, Cho J et al (2008) Curcumin: from ancient medicine to current clinical trials. Cell Mol Life Sci 65(11):1631–1652. https://doi.org/10.1007/s00018-008-7452-4
Epstein J, Sanderson IR, Macdonald T (2010) Curcumin as a therapeutic agent: the evidence from in vitro, animal and human studies. Br J Nutr 103(11):1545–1557. https://doi.org/10.1017/S0007114509993667
Hegge ABEE, Nielsen TT, Larsen KL et al (2012) Impact of curcumin supersaturation in antibacterial photodynamic therapy—effect of cyclodextrin type and amount: studies on curcumin and curcuminoides XLV. J Pharm Sci 101(4):1524–1537. https://doi.org/10.1002/jps.23046
Nardini EF, Almeida TS, Yoshimura TM et al (2019) The potential of commercially available phytotherapeutic compounds as new photosensitizers for dental antimicrobial PDT: a photochemical and photobiological in vitro study. Photodiagn Photodyn Ther 27:248–254. https://doi.org/10.1016/j.pdpdt.2019.05.027
Kumari A, Singh DK, Dash D, Singh R (2019) Intranasal curcumin protects against LPS-induced airway remodeling by modulating toll - like receptor-4 (TLR-4) and matrix metalloproteinase-9 (MMP-9) expression via affecting MAP kinases in mouse model. Inflammopharmacology 27(4):731–748. https://doi.org/10.1007/s10787-018-0544-3
Sorrenti V, Contarini G, Sut S et al (2018) Curcumin prevents acute neuroinflammation and long-term memory impairment induced by systemic lipopolysaccharide in mice. Front Pharmacol 9:183. https://doi.org/10.3389/fphar.2018.00183
Zhang J, Zheng Y, Luo Y et al (2019) Curcumin inhibits LPS-induced neuroinflammation by promoting microglial M2 polarization via TREM2 / TLR4 / NF- κ B pathways in BV2 cells. Mol Immunol 116:29–37. https://doi.org/10.1016/j.molimm.2019.09.020
Yan D, He B, Guo J et al (2019) Involvement of TLR4 in the protective effect of intra-articular administration of curcumin on rat. Acta Cir Bras 34(6):e201900604. https://doi.org/10.1590/s0102865020190060000004
Toraya S, Uehara O, Hiraki D et al (2020) Curcumin inhibits the expression of proinflammatory mediators and MMP-9 in gingival epithelial cells stimulated for a prolonged period with lipopolysaccharides derived from Porphyromonas gingivalis. Odontology 108(1):16–24. https://doi.org/10.1007/s10266-019-00432-8
Manoil D, Filieri A, Gameiro C et al (2014) Flow cytometric assessment of Streptococcus mutans viability after exposure to blue light-activated curcumin. Photodiagn Photodyn Ther 11(3):372–379. https://doi.org/10.1016/j.pdpdt.2014.06.003
Konan YN, Gurny R, Allemann E (2002) State of the art in the delivery of photosensitizers for photodynamic therapy. J Photochem Photobiol B Biol 66(2):89–106. https://doi.org/10.1016/S1011-1344(01)00267-6
Tavares LJ, Pavarina AC, Vergani CE, de Avila ED (2017) The impact of antimicrobial photodynamic therapy on peri-implant disease: what mechanisms are involved in this novel treatment? Photodiagn Photodyn Ther 17:236–244. https://doi.org/10.1016/j.pdpdt.2016.11.016
Alvarenga LH, Gomes AC, Carribeiro P et al (2019) Parameters for antimicrobial photodynamic therapy on periodontal pocket—randomized clinical trial. Photodiagn Photodyn Ther 27:132–136. https://doi.org/10.1016/j.pdpdt.2019.05.035
Plotino G, Grande NM, Mercade M (2019) Photodynamic therapy in endodontics. Int Endod J 52(6):760–774. https://doi.org/10.1111/iej.13057
Usacheva MN, Teichert MC, Biel MA (2003) The interaction of lipopolysaccharides with phenothiazine dyes. Lasers Surg Med 33(5):311–319. https://doi.org/10.1002/lsm.10226
Romualdo PC, Guerra TR, Romano FL et al (2017) Bacterial endotoxin adhesion to different types of orthodontic adhesives. J Appl Oral Sci 25(4):436–441. https://doi.org/10.1590/1678-7757-2016-0434
Rocha RA, Silva RAB, Assed S et al (2009) Nitric oxide detection in cell culture exposed to LPS after Er:YAG laser irradiation. Int Endod J 42(11):992–996. https://doi.org/10.1111/j.1365-2591.2009.01608.x
Warren MK, Vogel SN (1985) Bone marrow-derived macrophages: development and regulation of differentiation markers by colony-stimulating factor and interferons. J Immunol 134(2):982–989
de Carvalho RVH, Silva ALN, Santos LL et al (2019) Macrophage priming is dispensable for NLRP3 inflammasome activation and restriction of Leishmania amazonensis replication. J Leukoc Biol 106(3):631–640. https://doi.org/10.1002/JLB.MA1118-471R
de Castro-Jorge LA, de Carvalho RVH, Klein TM et al (2019) The NLRP3 inflammasome is involved with the pathogenesis of Mayaro virus. PLoS Pathog 15(9):e1007934. https://doi.org/10.1371/journal.ppat.1007934
da Frota MF, Guerreiro-Tanomaru JM, Tanomaru-Filho M et al (2015) Photodynamic therapy in root canals contaminated with Enterococcus faecalis using curcumin as photosensitizer. Lasers Med Sci 30(7):1867–1872. https://doi.org/10.1007/s10103-014-1696-z
Wikene KO, Hegge AB, Bruzell E, Tonnesen HH (2015) Formulation and characterization of lyophilized curcumin solid dispersions for antimicrobial photodynamic therapy (aPDT): studies on curcumin and curcuminoids LII. Drug Dev Ind Pharm 41(6):969–977. https://doi.org/10.3109/03639045.2014.919315
Mosmann T (1983) Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods 65(1–2):55–63. https://doi.org/10.1016/0022-1759(83)90303-4
Qiao J, Wang S, Wen Y, Jia H (2014) Photodynamic effects on human periodontal-related cells in vitro. Photodiagn Photodyn Ther 11(3):290–299. https://doi.org/10.1016/j.pdpdt.2014.04.001
Kayagaki N, Wong MT, Stowe IB et al (2013) Noncanonical inflammasome activation by intracellular LPS independent of TLR4. Science 341(6151):1246–1249. https://doi.org/10.5061/dryad.bt51g
Poltorak A, He X, Smirnova I et al (1998) Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in TLR4 gene. Science 282(5396):2085–2089. https://doi.org/10.1126/science.282.5396.2085
Hagar JA, Powell DA, Aachoui Y et al (2013) Cytoplasmic LPS activates caspase-11: implications in TLR4-independent endotoxic shock. Science 341(6151):1250–1253. https://doi.org/10.1126/science.1240988
O’Neill LAJ, Golenbock D, Bowie AG (2013) The history of Toll-like receptors - redefining innate immunity. Nat Publ Gr 13:453–460. https://doi.org/10.1038/nri3446
de Carvalho R, Andrade W, Lima-Junior DS et al (2019) Leishmania lipophosphoglycan triggers caspase-11 and the non-canonical activation of the NLRP3. Cell Rep 26(2):429–437.e5. https://doi.org/10.1016/j.celrep.2018.12.047
Raetz CRH, Whitfield C (2002) Lipopolysaccharide endotoxins. Annu Rev Biochem 71:635–700. https://doi.org/10.1146/annurev.biochem.71.110601.135414
Pulendran B, Kumar P, Cutler CW et al (2001) Lipopolysaccharides from distinct pathogens induce different classes of immune responses in vivo. J Immunol 167(9):5067–5076. https://doi.org/10.4049/jimmunol.167.9.5067
Diamond CE, Khameneh HJ, Brough D, Mortellaro A (2015) Novel perspectives on non-canonical inflammasome activation. ImmunoTargets Ther 4:131–141. https://doi.org/10.2147/ITT.S57976
Fumes AC, Romualdo PC, Monteiro RM et al (2018) Influence of pre-irradiation time employed in antimicrobial photodynamic therapy with diode laser. Lasers Med Sci 33(1):67–73. https://doi.org/10.1007/s10103-017-2336-1
Núñez SC, Garcez AS, Kato IT et al (2014) Effects of ionic strength on the antimicrobial photodynamic efficiency of methylene blue. Photochem Photobiol Sci 13(3):595–602. https://doi.org/10.1039/c3pp50325a
Misba L, Zaidi S, Khan AU (2018) Efficacy of photodynamic therapy against Streptococcus mutans biofilm: role of singlet oxygen. J Photochem Photobiol B Biol 183:16–21. https://doi.org/10.1016/j.jphotobiol.2018.04.024
Moradi Eslami L, Vatanpour M, Aminzadeh N, Mehrvarzfar P (2019) The comparison of intracanal medicaments, diode laser and photodynamic therapy on removing the biofilm of Enterococcus faecalis and Candida albicans in the root canal system (ex-vivo study). Photodiagn Photodyn Ther 26:157–161. https://doi.org/10.1016/j.pdpdt.2019.01.033
Asnaashari M, Mojahedi SM, Asadi Z et al (2016) A comparison of the antibacterial activity of the two methods of photodynamic therapy (using diode laser 810nm and LED lamp 630nm) against Enterococcus faecalis in extracted human anterior teeth. Photodiagn Photodyn Ther 13:233–237. https://doi.org/10.1016/j.pdpdt.2015.07.171
Rabello DGD, Corazza BJM, Ferreira LL et al (2017) Does supplemental photodynamic therapy optimize the disinfection of bacteria and endotoxins in one-visit and two-visit root canal therapy? A randomized clinical trial. Photodiagn Photodyn Ther 19:205–211. https://doi.org/10.1016/j.pdpdt.2017.06.005
Huang TC, Chen CJ, Ding SJ, Chen CC (2019) Antimicrobial efficacy of methylene blue-mediated photodynamic therapy on titanium alloy surfaces in vitro. Photodiagn Photodyn Ther 25:7–16. https://doi.org/10.1016/j.pdpdt.2018.11.008
Jiang C, Yang W, Wang C et al (2019) Methylene blue-mediated photodynamic therapy induces macrophage apoptosis via ROS and reduces bone resorption in periodontitis. Oxidative Med Cell Longev 2019:1529520. https://doi.org/10.1155/2019/1529520
Yilmaz S, Kuru B, Kuru L et al (2002) Effect of gallium arsenide diode laser on human periodontal disease: a microbiological and clinical study. Lasers Surg Med 30(1):60–66. https://doi.org/10.1002/lsm.10010
Hidalgo LR, da Silva LA, Nelson-Filho P et al (2016) Comparison between one-session root canal treatment with aPDT and two-session treatment with calcium hydroxide-based antibacterial dressing, in dog’s teeth with apical periodontitis. Lasers Med Sci 31(7):1481–1491. https://doi.org/10.1007/s10103-016-2014-8
Wilson BC, Patterson MS, Burns DM (1986) Effect of photosensitizer concentration in tissue on the penetration depth of photoactivation light. Lasers Med Sci 1:235–244. https://doi.org/10.1007/BF02032418
Stanford SC, Stanford BJ, Gillman PK (2010) Risk of severe serotonin toxicity following co-administration of methylene blue and serotonin reuptake inhibitors: an update on a case report of post-operative delirium. J Psychopharmacol 24(10):1433–1438. https://doi.org/10.1177/0269881109105450
Gillman PK (2011) CNS toxicity involving methylene blue: the exemplar for understanding and predicting drug interactions that precipitate serotonin toxicity. J Psychopharmacol 25(3):429–436. https://doi.org/10.1177/0269881109359098
NouhzadehMalekshah S, Fekrazad R, Bargrizan M, Kalhori KA (2019) Evaluation of laser fluorescence in combination with photosensitizers for detection of demineralized lesions. Photodiagn Photodyn Ther 26:300–305. https://doi.org/10.1016/j.pdpdt.2019.03.019
Dai T, Bill de Arce VJ, Tegos GP, Hamblin MR (2011) Blue dye and red light, a dynamic combination for prophylaxis and treatment of cutaneous Candida albicans infections in mice. Antimicrob Agents Chemother 55(12):5710–5717. https://doi.org/10.1128/AAC.05404-11
Rodrigues GB, Dias-Baruffi M, Holman N et al (2013) In vitro photodynamic inactivation of Candida species and mouse fibroblasts with phenothiazinium photosensitisers and red light. Photodiagn Photodyn Ther 10(2):141–149. https://doi.org/10.1016/j.pdpdt.2012.11.004
Brancini GTP, Rodrigues GB, Rambaldi MSL et al (2016) The effects of photodynamic treatment with new methylene blue N on Candida albicans proteome. Photochem Photobiol Sci 15(12):1503–1513. https://doi.org/10.1039/C6PP00257A
Fekrazad R, Mir APB, Aghdam M, Barghi VG (2017) Comparison of photoinactivation of T. rubrum by new methylene blue. Photodiagn Photodyn Ther 18:208–212. https://doi.org/10.1016/j.pdpdt.2016.10.013
Tonani L, Morosini NS, de Menezes HD et al (2018) In vitro susceptibilities of Neoscytalidium spp. sequence types to antifungal agents and antimicrobial photodynamic treatment with phenothiazinium photosensitizers. 122(6):436–448. https://doi.org/10.1016/j.funbio.2017.08.009
Usacheva MN, Teichert MC, Biel MA (2001) Comparison of the methylene blue and toluidine blue photobactericidal efficacy against gram-positive and gram-negative microorganisms. Lasers Surg Med 29(2):165–173. https://doi.org/10.1002/lsm.1105
Salminen A, Gursoy UK, Paju S et al (2014) Salivary biomarkers of bacterial burden, inflammatory response, and tissue destruction in periodontitis. J Clin Periodontol 41(5):442–450. https://doi.org/10.1111/jcpe.12234
Sivieri-Araujo G, Queiroz ÍOA, Fabbro RD et al (2017) Rat tissue reaction and cytokine production induced by antimicrobial photodynamic therapy. Photodiagn Photodyn Ther 18:315–318. https://doi.org/10.1016/j.pdpdt.2017.04.002
Curylofo-Zotti FA, Elburki MS, Oliveira PA et al (2018) Differential effects of natural Curcumin and chemically modified curcumin on inflammation and bone resorption in model of experimental periodontitis. Arch Oral Biol 91:42–50. https://doi.org/10.1016/j.archoralbio.2018.04.007
Xiao CJ, Yu XJ, Xie JL et al (2018) Protective effect and related mechanisms of curcumin in rat experimental periodontitis. Head Face Med 14(1):12. https://doi.org/10.1186/s13005-018-0169-1
Li W, Suwanwela NC, Patumraj S (2017) Curcumin prevents reperfusion injury following ischemic stroke in rats via inhibition of NF-κB, ICAM-1, MMP-9 and caspase-3 expression. Mol Med Rep 16(4):4710–4720. https://doi.org/10.3892/mmr.2017.7205
Gursoy H, Ozcakir-Tomruk C, Tanalp J et al (2013) Photodynamic therapy in dentistry: a literature review. Clin Oral Investig 17(4):1113–1125. https://doi.org/10.1007/s00784-012-0845-7
Singh S, Nagpal R, Manuja N, Tyagi SP (2015) Photodynamic therapy: an adjunct to conventional root canal disinfection strategies. Aust Endod J 41(2):54–71. https://doi.org/10.1111/aej.12088
Gomes-Filho JE, Sivieri-Araujo G, Sipert CR et al (2016) Evaluation of photodynamic therapy on fibroblast viability and cytokine production. Photodiagn Photodyn Ther 13:97–100. https://doi.org/10.1016/j.pdpdt.2016.01.007
Hamblin MR, Zahra T, Contag CH et al (2003) Optical monitoring and treatment of potentially lethal wound infections in vivo. J Infect Dis 187(11):1717–1725. https://doi.org/10.1086/375244.Optical
Ahn H, Kang SG, Yoon SI et al (2017) Methylene blue inhibits NLRP3, NLRC4, AIM2, and non-canonical inflammasome activation. Sci Rep 7:1–13. https://doi.org/10.1038/s41598-017-12635-6
Memis D, Karamanlioglu B, Yuksel M et al (2002) The influence of methylene blue infusion on cytokine levels during severe sepsis. Anaesth Intensive Care 30:755–762. https://doi.org/10.1177/0310057x0203000606
Takayama K, Qureshi N, Raetz CR (1984) Influence of fine structure of lipid A on limulus amebocyte lysate clotting and toxic activities. Infect Immun 45(2):350–355. https://doi.org/10.1128/iai.45.2.350-355.1984
Proctor RA, Textor JA (1985) Activation and inhibition of Limulus amebocyte lysate coagulation by chemically defined substructures of lipid A. Infect Immun 49(2):286–290. https://doi.org/10.1128/iai.49.2.286-290.1985
Morrison DC, Ryan JL (1987) Endotoxins and disease. Ann Rev Med 38:417–432. https://doi.org/10.1146/annurev.me.38.020187.002221
Acknowledgments
We are thankful to Prof. Dr. Dario Simões Zamboni for providing reagents and important resources for the development of this work. We also thank Izaíra Ticani Brandão and Nilza Letícia Magalhães for their technical support for this study in LAL Assays. Finally, we are grateful for Prof. Dr. Zeki Naal, Profa. Dra. Lúcia Helena Faccioli, and their lab members for the lab and equipment availability.
Funding
This work was supported by grants from the Coordination for the Improvement of Higher Education Personnel - Academic Excellence Program (CAPES-PROEX process 23038.000712/2018-34) and São Paulo Research Foundation (FAPESP process 2016/113386-5).
Author information
Authors and Affiliations
Contributions
A.C.F.C. and R.V.H.C. designed, generated figures, wrote, and performed experiments. G.U.L.B., M.C.B., and R.A.B.S. provided reagents and tools. A.C.F.C., R.V.H.C., G.T.P.B., F.G.M., C.A.S., R.A.B.S., P.N.F., F.W.G.P.S., G.U.L.B., M.C.B., and A.B.N.J. analyzed the data, discussed hypotheses, and revised the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Role of funding source
Grants from Coordenação de Aperfeiçoamento de Pessoal de Nível Superior-Programa de Excelência Acadêmica (CAPES-PROEX process 23,038.000712/2018-34) and Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP process 2016/113386-5) were crucial for the development of this work.
Ethical approval
The research project was approved by the Ethics Committee on the Use of Animals of the Faculty of Dentistry of Ribeirão Preto, University of São Paulo (process 2019.1.173.58.4) and was carried out following international standards for experimentation on live animals and the rules of the National Council for the Control of Animal Experimentation (CONCEA).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ana Carolina Fernandes Couto and Renan Villanova Homem de Carvalho are joint first authors
Rights and permissions
About this article
Cite this article
Couto, A.C.F., de Carvalho, R.V.H., Brancini, G.T.P. et al. Photosensitizers attenuate LPS-induced inflammation: implications in dentistry and general health. Lasers Med Sci 36, 913–926 (2021). https://doi.org/10.1007/s10103-020-03180-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-020-03180-2