Abstract
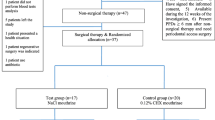
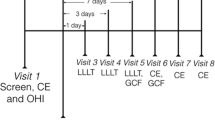
The aim of this study was to evaluate the effects of photobiomodulation therapy (PBM) and ozone applications on patients’ quality of life after gingivectomy and gingivoplasty. In this study, 36 patients with chronic inflammatory gingival enlargement underwent gingivectomy and gingivoplasty. The groups were randomly divided into control (n = 12), PBM (n = 12) and ozone (n = 12) groups. GaAlAs diode laser 810 nm wavelength at a non-contact and continuous mode with a power of 0.3 W and a density of 4 J/cm2 used for PBM for 1 min. Ozone was applied for 1 min for every 5 mm2 in contact mode at power level 9 using probe number 3. PBM and ozone applications were performed immediately after the operation, on the 3rd and 7th days. Pain assessment was performed at 3rd, 7th, 14th and 28th days after gingivectomy and gingivoplasty by using visual analogue scale (VAS). Oral Health Impact Profile (OHIP-14) records were obtained from the patients before gingivectomy and gingivoplasty and postoperative 7th and 14th days. OHIP-14 questions were also evaluated individually. VAS pain levels of the control group measured on the 3rd day were higher than the PBM group and on the 7th day were found to be significantly higher than both groups (p < 0.05). The total OHIP-14 score of the control group on the 7th postoperative day was found to be higher than the PBM group (p < 0.05). The mean score obtained from the third question of OHIP-14 at 7th and 14th day of the PBM group was found to be lower than the control and ozone groups (p < 0.05). The PBM and ozone applications after gingivectomy and gingivoplasty reduce the pain levels of patients and have a positive effect on patients’ quality of life.







Similar content being viewed by others
References
Fay AA, Satheesh K, Gapski R (2005) Felodipine-influenced gingival enlargement in an uncontrolled type 2 diabetic patient. J Periodontol 76:1217–1222
Seymour RA (2006) Effects of medications on the periodontal tissues in health and disease. Periodontol 2000(40):120–129
Goldman HM (1950) The development of physiologic gingival contours by gingivoplasty. Oral Surg Oral Med Oral Pathol 3:879–888
Witte MB, Barbul A (1997) General principles of wound healing. Surg Clin North Am 77:509–528
Akgul S, Kiziltoprak M, Uslu MO (2018) Ozone therapy in periodontology. Sci J Research & Rev 1:1–3
Gupta G, Mansi B (2012) Ozone therapy in periodontics. J Med Life 5:59–67
Walsh LJ (1997) The current status of low level laser therapy in dentistry. Part 1. Soft tissue applications. Aust Dent J 42:247–254
Carlsson AM (1983) Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain 16:87–101
Crichton N (2001) Information point: visual analogue scale (VAS). J Clin Nurs 10:697–706
WHOQOL group (1993) Study protocol for the World Health Organization project to develop a quality of life assessment instrument (WHOQOL). Qual Life Res 2:153–159
John MT, Hujoel P, Miglioretti DL, LeResche L, Koepsell TD, Micheelis W (2004) Dimensions of oral-health-related quality of life. J Dent Res 83:956–960
Basol ME, Karaagaclioglu L, Yilmaz B (2014) Türkçe ağız sağlığı etki ölçeğinin geliştirilmesi-OHIP-14-TR. Turkiye Klinikleri J Dental Sci 20:85–92
Slade GD, Spencer AJ (1994) Development and evaluation of the oral health impact profile. Community Dent Health 11:3–11
Jenkins PA, Carroll JD (2011) How to report low-level laser therapy (LLLT)/photomedicine dose and beam parameters in clinical and laboratory studies. Photomed Laser Surg 29:785–787
Kelly AM (2001) The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J 18:205–207
Locker D (1988) Measuring oral health:a conceptual framework. Community Dent Health 5:3–18
Slade GD (1997) Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol 25:284–290
Taskan MM (2015) Laser-assisted gingivectomy techniques used in treatment of chronic inflammatory gingival enlargement: a review. Cumhuriyet Dent J 18:370–379
Sobouti F, Rakhshan V, Chiniforush N, Khatami M (2014) Effects of laser-assisted cosmetic smile lift gingivectomy on postoperative bleeding and pain in fixed orthodontic patients: a controlled clinical trial. Prog Orthod 15:66
Rivera AE, Spencer JM (2007) Clinical aspects of full-thickness wound healing. Clin Dermatol 25:39–48
Enoch S, Leaper DJ (2008) Basic science of wound healing. Surgery (Oxford) 26:31–37
Dogan GE, Demir T, Orbak R (2014) Periodontolojide düşük doz lazer uygulamaları. Clin Exp Health Sci 4:43–50
Tarhan K, Alkan BA (2015) Periodontal tedavide düşük doz lazer tedavisi uygulamaları. J Dent Fac Atatürk Uni 24:61–66
Bjordal JM, Johnson MI, Iversen V, Aimbire F, Lopes-Martins RA (2006) Photoradiation in acute pain: a systematic review of possible mechanisms of action and clinical effects in randomized placebo-controlled trials. Photomed Laser Surg 24:158–168
Kohale BR, Agrawal AA, Raut CP (2018) Effect of low-level laser therapy on wound healing and patients' response after scalpel gingivectomy: a randomized clinical split-mouth study. J Indian Soc Periodontol 22:419–426
Amorim JC, de Sousa GR, de Barros SL, Prates RA, Pinotti M, Ribeiro MS (2006) Clinical study of the gingiva healing after gingivectomy and low-level laser therapy. Photomed Laser Surg 24:588–594
Ozcelik O, Cenk Haytac M, Kunin A, Seydaoglu G (2008) Improved wound healing by low-level laser irradiation after gingivectomy operations: a controlled clinical pilot study. J Clin Periodontol 35:250–254
Lingamaneni S, Mandadi LR, Pathakota KR (2019) Assessment of healing following low-level laser irradiation after gingivectomy operations using a novel soft tissue healing index: a randomized, double-blind, split-mouth clinical pilot study. J Indian Soc Periodontol 23:53–57
Masse JF, Landry RG, Rochette C, Dufour L, Morency R, d'Aoust P (1993) Effectiveness of soft laser treatment in periodontal surgery. Int Dent J 43:121–127
Slade GD, Spencer AJ (1994) Social impact of oral conditions among older adults. Aust Dent J 39:358–364
Bocci V (1999) Biological and clinical effects of ozone. Has ozone therapy a future in medicine? Br J Biomed Sci 56:270–279
Tasdemir Z, Alkan BA, Albayrak H (2016) Effects of ozone therapy on the early healing period of deepithelialized gingival grafts: a randomized placebo-controlled clinical trial. J Periodontol 87:663–671
Ozcelik O, Haytac MC, Seydaoglu G (2007) Immediate post-operative effects of different periodontal treatment modalities on oral health-related quality of life: a randomized clinical trial. J Clin Periodontol 34:788–796
Kazancioglu HO, Ezirganli S, Demirtas N (2014) Comparison of the influence of ozone and laser therapies on pain, swelling, and trismus following impacted third-molar surgery. Lasers Med Sci 29:1313–1319
Acknowledgments
The authors thank statistician Hande Emir, SWOT Statistics, Istanbul, for the help in statistical analysis.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics statement/confirmation of patients’ permission
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board of Malatya Clinical Research Ethics Committee (Protocol No: 2018/113) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed and written consent was obtained from all participants individual included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Uslu, M.Ö., Akgül, S. Evaluation of the effects of photobiomodulation therapy and ozone applications after gingivectomy and gingivoplasty on postoperative pain and patients’ oral health-related quality of life. Lasers Med Sci 35, 1637–1647 (2020). https://doi.org/10.1007/s10103-020-03037-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-020-03037-8