Abstract
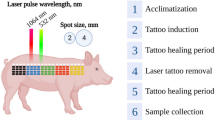
Characteristics such as skin tone and pigmentation color vary among patients, but most researches on laser irradiation in laser ablation have revolved around minimizing damage to reduce pain. Chromophores are the most important factors in photon energy absorption, a key principle of laser ablation. We investigated the influences on ablation depth by different chromophores on the target and modulating duration per laser exposure using an Nd:YVO4 nanosecond 532-nm laser. We used a Fourier-domain optical coherence tomography (Fd-OCT) system combined with a 532-nm Nd:YVO4 laser to observe the ablation process. In addition, an external customized shutter and water-based color pens (red, green, blue, black) were used to determine the effects of modulating the duration per laser exposure and coloring chromophores on porcine skin and hairless mouse models. Experiments with modulating duration per laser exposure demonstrated that shorter duration generated shallower craters than longer one. Painted experimental group showed damaged region as craters in the experiments with coloring various chromophores. In this research, we investigated the effects of modulating duration per laser exposure and different chromophores on the target. Coloring chromophores with water-based dyes using pens increased tissue damage without dyeing cells or tissue.





Similar content being viewed by others
References
Studdert V. P, Gay CC, Blood DC (2007) Saunders comprehensive veterinary dictionary 3rd. Saunders Elsevier, St. Louis, Missouri, USA
Gower MC (2000) Industrial applications of laser micromachining. Opt Express 7(2):56–67. https://doi.org/10.1364/OE.7.000056
Cutroneo M, Torrisi L, Seolaro C (2010) Laser applications in bio-medical field
Ohmi M, Tanizawa M, Fukunaga A, Haruna M (2005) In-situ observation of tissue laser ablation using optical coherence tomography. Opt Quant Electron 37(13–15):1175–1183. https://doi.org/10.1007/s11082-005-4189-2
Hsieh YS, Ho YC, Lee SY, Chuang CC, Tsai J, Lin KF, Sun CW (2013) Dental optical coherence tomography. Sensors 13(7):8928–8949. https://doi.org/10.3390/s130708928
Vogl TJ, Eichler K, Mack MG, Zangos S, Herzog C, Thalhmmer A, Englemann K (2004) Interstitial photodynamic laser therapy in interventional oncology. Eur Radiol 14(6):1063–1073. https://doi.org/10.1007/s00330-004-2290-8
Liao H, Fujiwara K, Ando T, Maruyama T, Kobayashi E, Muragaki Y, Iseki H, Sakuma I (2013) Automatic laser scanning ablation system for high-precision treatment of brain tumors. Lasers Med Sci 28:891–900. https://doi.org/10.1007/s10103-012-1164-6
Ngoi BKA, Hou DX, Koh LHK, Hoh ST (2005) Femtosecond laser for glaucoma treatment: a study on ablation energy in pig iris. Lasers Med Sci 19:218–222. https://doi.org/10.1007/s10103-004-0323-9
Mir M, Meister J, Franzen R, Sabounchi SS, Lampert F, Gutknecht N (2008) Influence of water-layer thickness on Er:YAG laser ablation of enamel of bovine anterior teeth. Lasers Med Sci 23:451–457. https://doi.org/10.1007/s10103-007-0508-0
Beier C, Kaufmann R (1999) Efficacy of erbium:YAG laser ablation in darier disease and Hailey Hailey disease. Arch Dermatol 135(4):423–427. https://doi.org/10.1001/archderm.135.4.423
Kuperman-Beade M, Levine VJ, Ashinoff R (2001) Laser removal of tattoos. Am J Clin Dermatol 2(1):21–25. https://doi.org/10.1177/039463201202500226
Walsh JT, Flotte TJ, Deutsch TF (1989) Er:YAG laser ablation of tissue : effect of pulse duration and tissue type on thermal damage. Lasers Surg Med 9(4):314–326. https://doi.org/10.1002/lsm.1900090403
Walsh JT, Flotte TJ, Anderson RR, Deutsch TF (1988) Pulsed CO2 laser tissue ablation: effect of tissue type and pulse duration on thermal damage. Lasers Surg Med 8(2):108–118. https://doi.org/10.1002/lsm.1900080204
Walsh JT, Deutsch TF (1988) Pulsed CO2 laser tissue ablation: measurement of the ablation rate. Laser Surg Med 8(3):264–275. https://doi.org/10.1002/lsm.1900080308
Cummings JP, Walsh JT (1993) Tissue tearing caused by pulsed laser induced ablation pressure. Appl Opt 32(4):494–503. https://doi.org/10.1364/AO.32.000494
Walsh JT, Van Leeuwen TG, Jansen ED, Motamedi M, Welch AJ (2011) Pulsed laser tissue interaction. In: Welch A, van Gemert M (eds) Optical-thermal response of laser-irradiated tissue. Springer, Dordrecht, pp 617–649
Kang HW, Kim JH, Steven PY (2013) In vitro investigation of wavelength-dependent tissue ablation: laser prostatectomy between 532nm and 2,01um. Lasers Surg Med 42(3):237–244. https://doi.org/10.1007/s10103-012-1235-8
Huang Y, Jivraj J, Zhou J, Ramjist J, Wong R, Gu X, Yang VX (2016) Pulsed and CW adjustable 1942nm single-mode all-fiber Tm-doped fiber laser system for surgical laser soft tissue ablation applications. Opt Express 24(15):11674–11686. https://doi.org/10.1364/OE.24.016674
Steiner R, Kunzi-Rapp K, Scharffetter-Kochanek K (2003) Optical coherence tomography: clinical applications in dermatology. Med Laser Appl 18(3):249–259. https://doi.org/10.1078/1615-1615-00107
Fercher AF, Drexler W, Hitzenberger CK, Lasser T (2003) Optical coherence tomography-principles and applications. Rep Prog Phys 66(2):239–303. https://doi.org/10.1088/0034-4885/66/2/204
Kim BK, Kim DY (2016) Enhanced tissue ablation efficiency with a mid-infrared nonlinear frequency conversion laser system and tissue interaction monitoring using optical coherence tomography. Sensors 16(5):598. https://doi.org/10.3390/s16050598
Wisweh H, Merkel U, Hüller A, Lüerßen K, Lubatschowski H (2007) Optical coherence tomography monitoring of vocal fold femtosecond laser microsurgery. Therapeutic Laser Applications and Laser-Tissue Interactions III Vol 6632_6 of Proceedings of SPIE-OSA Biomedical Optics https://doi.org/10.1364/ECBO.2007.6632_6
Kim DY, Fingler J, Zawadzki RJ, Park SS, Morse LS, Schwartz DM, Fraser SE, Werner JS (2012) Noninvasive imaging of the foveal avascular zone with high-speed, phase-variance optical coherence tomography. Invest Ophthalmol Vis Sci 53(1):85–92. https://doi.org/10.1167/iovs.11-8249
Kim DY, Werner JS, Zawadzki RJ (2012) Complex conjugated artifact-free adaptive optics optical coherence tomography of in vivo human optic nerve head. J Biomed Opt 17(12):126005. https://doi.org/10.1117/1.JBO.17.12.126005
Kim DY, Fingler J, Zawadzki RJ, Park SS, Morse LS, Schwartz DM, Fraser SE, Werner JS (2013) Optical imaging of the chorioretinal vasculature in the living human eye. PNAS 110(35):14354–14359. https://doi.org/10.1073/pnas.1307315110
Cho NH, Park KB, Wijesinghe RE, Shin YS, Jung WG, Kim JH (2014) Development of real-time dual-display handheld and bench-top hybrid-mode SD-OCTs. Sensors 14(2):2171–2181. https://doi.org/10.3390/s140202171
Wessels R, De Bruin DM, Faber DJ, Van Leeuwen TG, Van Beurden M, Ruers TJM (2014) Optical biopsy of epithelial cancers by optical coherence tomography (OCT). Lasers Med Sci 29:1297–1305. https://doi.org/10.1007/s10103-013-1291-8
Cho NH, Lee SH, Jung W, Jang JH, Kim J (2015) Optical coherence tomography for the diagnosis and evaluation of human otitis media. J Korean Med Sci 30(3):328–335. https://doi.org/10.3346/jkms.2015.30.3.328
Murphy MJ, Torstensson PA (2014) Thermal relaxation times: an outdated concept in photothermal treatments. Lasers Med Sci 29(3):973–978. https://doi.org/10.1007/s10103-013-1445-8
Yadav RK (2009) Definitions in laser technology. J Cutan Aesthet Surg 2(1):45–46. https://doi.org/10.4103/0974-2077.53103
Hamblin MR, Demidova TN (2006) Mechanisms of low level light therapy. Proc SPIE 6140:614001. https://doi.org/10.1117/12.646294
Jacobi U, Kaiser M, Toll R, Mangelsdorf S, Audring H, Otberg N, Sterry W, Lademann J (2007) Porcine ear skin: an in vitro model for human skin. Skin Res Technol 13(1):19–24. https://doi.org/10.1111/j.1600-0846.2006.00179.x
Funding
This research was financially supported in INHA UNIVERSITY Research Grant (INHA-55436). The laser used in these studies was provided by Dong Jun Shin (EO Technics Co., Ltd., Anyang, South Korea). This work was presented at the 2017 SPIE Photonics West conference.
Author information
Authors and Affiliations
Contributions
Hang Chan Jo designed and performed the experiments, analyzed the data, and wrote the paper. Dae Yu Kim conceived and designed the experiments, supervised the work, and revised the paper.
Corresponding author
Ethics declarations
Experiments using hairless mouse were approved by the institutional animal care and use committee (IACUC) of Dankook University.
Conflicts of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Jo, H.C., Kim, D.Y. Observations of in vivo laser tissue ablation in animal models with different chromophores on the skin and modulating duration per laser exposure. Lasers Med Sci 34, 1031–1039 (2019). https://doi.org/10.1007/s10103-018-2693-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-018-2693-4