Abstract
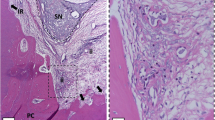
The aim of this study was to compare the rate of tooth displacement, quantity of root resorption, and alveolar bone changes in five groups: corticopuncture (CP), low-level laser therapy (LLLT), CP combined with LLLT (CP + LLLT), control (C), and negative control (NC). A total of 60 half-maxilla from 30 male Wistar rats (10 weeks old) were divided randomly into five groups: three (CP, LLLT, and CP + LLLT) test groups with different stimulation for accelerated-tooth-movement (ATM), one control (C) group, and one negative control (NC) group with no tooth movement. Nickel-titanium coil springs with 50 g of force were tied from the upper left and right first molars to micro-implants placed behind the maxillary incisors. For the CP and CP + LLLT groups, two perforations in the palate and one mesially to the molars were performed. For the LLLT and CP + LLLT groups, GaAlAs diode laser was applied every other day for 14 days (810 nm, 100 mW, 15 s). The tooth displacements were measured directly from the rat’s mouth and indirectly from microcomputer (micro-CT) tomographic images. Bone responses at the tension and compression sites and root resorption were analyzed from micro-CT images. The resulting alveolar bone responses were evaluated by measuring bone mineral density (BMD), bone volume fraction (BV/TV), and trabecular thickness (TbTh). Root resorption crater volumes were measured on both compression and tension sides of mesial and distal buccal roots. The tooth displacement in the CP + LLLT group was the greatest when measured clinically, followed by the CP, LLLT, and control groups (C and NC), respectively (p <0.05). The tooth movements measured from micro-CT images showed statistically higher displacement in the CP and CP + LLLT groups compared to the LLLT and control groups. The BMD, BV/TV, and TbTh values were lower at the compression side and higher at the tension side for all three test groups compared to the control group. The root resorption crater volume of the distal buccal root was higher in the control group, followed by CP, LLLT, and CP + LLLT, mostly at the compression site. Combining corticopuncture and low-level laser therapy (CP + LLLT) produced more tooth displacement and less root resorption at the compression side. The combined technique also promoted higher alveolar bone formation at the tension side.









Similar content being viewed by others
References
Meikle MC (2005) The tissue, cellular, and molecular regulation of orthodontic tooth movement: 100 years after Carl Sandstedt. Eur J Orthod 28:221–240. https://doi.org/10.1093/ejo/cjl001
Yoshida T, Yamaguchi M, Utsunomiya T et al (2009) Low-energy laser irradiation accelerates the velocity of tooth movement via stimulation of the alveolar bone remodeling. Orthod Craniofac Res 12:289–298. https://doi.org/10.1111/j.1601-6343.2009.01464.x
Üretürk SE, Saraç M, Fıratlı S, Can ŞB3, Güven Y FE (2017) The effect of low-level laser therapy on tooth movement during canine distalization. Lasers Med Sci 32:757–764
Nishimura M, Chiba M, Ohashi T, Sato M, Shimizu Y, Igarashi K et al (2008) Periodontal tissue activation by vibration: intermitente stimulation by resonance vibration accelerates experimental tooth movement in rats. Am J Orthod Dentofac Orthop 133:572–583
Ali Darendeliler M, Zea a., Shen G, Zoellner H (2007) Effects of pulsed electromagnetic field vibration on tooth movement induced by magnetic and mechanical forces: a preliminary study. Aust Dent J 52:282–287. doi: https://doi.org/10.1111/j.1834-7819.2007.tb00503.x
Igarashi K, Adachi H, Mitani H, Shinoda H (1996) Inhibitory effect of the topical administration of a bisphosphonate (risedronate) on root resorption incident to orthodontic tooth movement in rats. J Dent Res 75:1644–1649
Wilcko WM, Wilcko T, Bouquot JE, Ferguson DJ (2001) Rapid orthodontics with alveolar reshaping: two case reports of decrowding. Int J Periodontics Restorative Dent 21:9–19
Lee W, Karapetyan G, Moats R, Yamashita DD, Moon HB, Ferguson DJ et al (2008) Corticotomy−/osteotomy-assisted tooth movement microCTs differ. J Dent Res 87:861–867
Wang L, Lee W, Lei DL, Liu YP, Yamashita DDYS (2009) Tisssue responses in corticotomy- and osteotomy-assisted tooth movements in rats: histology and immunostaining. Am J Orthod Dentofac Orthop 136:e1–11
Liou EJHC (1998) Rapid canine retraction through distraction of the periodontal ligament. Am J Orthod Dentofac Orthop 114:372–382
Köle H (1959) Surgical operations on the alveolar ridge to correct occlusal abnormalities. Oral Surg oral med oral Pathol 12:515–529 concl. doi: https://doi.org/10.1016/0030-4220(59)90177-X
Shih M, Norrdin R (1985) Regional acceleration of remodeling during healing of bone defects in beagles of various ages. Bone 6:377–379
Kim SJ, Park YG, Kang SG (2008) Effects of corticision on paradental remodeling in orthodontic tooth movement. Angle Orthod 79:284–291. https://doi.org/10.2319/020308-60.1
Kim YS, Kim SJ, Yoon HJ et al (2013) Effect of piezopuncture on tooth movement and bone remodeling in dogs. Am J Orthod Dentofac Orthop 144:23–31. https://doi.org/10.1016/j.ajodo.2013.01.022
Alikhani M, Raptis M, Zoldan B et al (2013) Effect of micro-osteoperforations on the rate of tooth movement. Am J Orthod Dentofac Orthop 144:639–648. https://doi.org/10.1016/j.ajodo.2013.06.017
Cheung T, Park J, Lee D et al (2016) Ability of mini-implant-facilitated micro-osteoperforations to accelerate tooth movement in rats. Am J Orthod Dentofac Orthop 150:958–967. https://doi.org/10.1016/j.ajodo.2016.04.030
Lim HM, Lew KK, Tay DK (1995) A clinical investigation of the efficacy of low level laser therapy in reducing orthodontic postadjustment pain. Am J Orthod Dentofac Orthop 108:614–622
Rodrigues MT, Ribeiro MS, Groth EBZD (2002) Evaluation of effects of laser therapy (λ=830 nm) on oral ulceration induced by fixed orthodontic appliances. Lasers Lasers Surg Med 30:15
Ozawa Y, Shimizu N, Kariya G, Abiko Y (1998) Low-energy laser irradiation stimulates bone nodule formation at early stages of cell culture in rat calvarial cells. Bone 22:347–354. https://doi.org/10.1016/S8756-3282(97)00294-9
Kawasaki K, Shimizu N (2000) Effects of low-energy laser irradiation on bone remodeling during experimental tooth movement in rats. Lasers Surg Med 26:282–291. https://doi.org/10.1002/(SICI)1096-9101(2000)26:3<282::AID-LSM6>3.0.CO;2-X
Aihara N, Yamaguchi M, Kasai K (2006) Low-energy irradiation stimulates formation of osteoclast-like cells via RANK expression in vitro. Lasers Med Sci 21:24–33. https://doi.org/10.1007/s10103-005-0368-4
Torri S, Weber JBB (2013) Influence of low-level laser therapy on the rate of orthodontic movement: a literature review. Photomed Laser Surg 31:411–421. https://doi.org/10.1089/pho.2013.3497
Ge MK, He WL, Chen J, et al (2015) Efficacy of low-level laser therapy for accelerating tooth movement during orthodontic treatment: a systematic review and meta-analysis. Lasers Med Sci 1–10. doi: doi: https://doi.org/10.1007/s10103-014-1538-z
Suzuki SS, Silva Garcez A, Suzuki H et al (2016) Low-level laser therapy stimulates bone metabolism and inhibits root resorption during tooth movement in a rodent model. J Biophotonics 1235:1222–1235. https://doi.org/10.1002/jbio.201600016
Kim SJ, Moon SU, Kang SG, Park YG (2009) Effects of low-level laser therapy after corticision on tooth movement and paradental remodeling. Lasers Surg Med 41:524–533. https://doi.org/10.1002/lsm.20792
Seifi M, Shafeei HA, Daneshdoost S, Mir M (2007) Effects of two types of low-level laser wave lengths (850 and 630 nm) on the orthodontic tooth movements in rabbits. Lasers Med Sci 22:261–264. https://doi.org/10.1007/s10103-007-0447-9
Han KH, Park JH, Bayome M, et al (2014) Effect of frequent application of low-level laser therapy on corticotomized tooth movement in dogs: a pilot study. J Oral Maxillofac Surg 72:1182.e1–1181182.e12. doi: https://doi.org/10.1016/j.joms.2014.02.028
Grant M, Wilson J, Rock P, Chapple I (2013) Induction of cytokines, MMP9, TIMPs, RANKL and OPG during orthodontic tooth movement. Eur J Orthod 35:644–651. https://doi.org/10.1093/ejo/cjs057
Nakano Y, Yamaguchi M, Fujita S et al (2011) Expressions of RANKL/RANK and M-CSF/c-fms in root resorption lacunae in rat molar by heavy orthodontic force. Eur J Orthod 33:335–343. https://doi.org/10.1093/ejo/cjq068
Taddei SRDA, Moura AP, Andrade I et al (2012) Experimental model of tooth movement in mice: a standardized protocol for studying bone remodeling under compression and tensile strains. J Biomech 45:2729–2735. https://doi.org/10.1016/j.jbiomech.2012.09.006
D’Andrea Fonseca P, De Lima FM, Higashi DT et al (2013) Effects of light emitting diode (LED) therapy at 940 nm on inflammatory root resorption in rats. Lasers Med Sci 28:49–55. https://doi.org/10.1007/s10103-012-1061-z
Youssef M, Ashkar S, Hamade E et al (2008) The effect of low-level laser therapy during orthodontic movement: a preliminary study. Lasers Med Sci 23:27–33. https://doi.org/10.1007/s10103-007-0449-7
Garcez AS, Suzuki SS, Martinez EF, et al (2015) Effects of low-intensity laser therapy over mini-implants success rate in pigs. Lasers Med Sci 30:727–732. https://doi.org/10.1007/s10103-013-1367-5
Kwak J, Zara JN, Chiang M et al (2013) NELL-1 injection maintains long-bone quantity and quality in an ovariectomy-induced osteoporotic senile rat model. Tissue Eng Part A 19:426–436. https://doi.org/10.1089/ten.TEA.2012.0042
Al-Daghreer S, Doschak M, Sloan AJ et al (2014) Effect of low-intensity pulsed ultrasound on orthodontically induced root resorption in beagle dogs. Ultrasound Med Biol 40:1187–1196. https://doi.org/10.1016/j.ultrasmedbio.2013.12.016
Kim YS, Kim SJ, Yoon HJ et al (2013) Effect of piezopuncture on tooth movement and bone remodeling in dogs. Am J Orthod Dentofac Orthop 144:23–31. https://doi.org/10.1016/j.ajodo.2013.01.022
Tsai CY, Yang TK, Hsieh HY, Yang LY (2016) Comparison of the effects of micro-osteoperforation and corticision on the rate of orthodontic tooth movement in rats. Angle Orthod 86:558–564. https://doi.org/10.2319/052015-343.1
Cruz DR, Kohara EK, Ribeiro MS, Wetter NU (2004) Effects of low-intensity laser therapy on the orthodontic movement velocity of human teeth: a preliminary study. Lasers Surg Med 35:117–120. https://doi.org/10.1002/lsm.20076
Sonesson M, De Geer E, Subraian J, Petrén S (2017) Efficacy of low-level laser therapy in accelerating tooth movement, preventing relapse and managing acute pain during orthodontic treatment in humans: a systematic review. BMC Oral Health 17:11. https://doi.org/10.1186/s12903-016-0242-8
Baloul SS, Gerstenfeld LC, Morgan EF, et al Mechanism of action and morphologic changes in the alveolar bone in response to selective alveolar decortication-facilitated tooth movement. Am J Orthod Dentofac Orthop 139:S83–S101. doi: https://doi.org/10.1016/j.ajodo.2010.09.026
Yoshida T, Yamaguchi M, Utsunomiya T et al (2009) Low-energy laser irradiation accelerates the velocity of tooth movement via stimulation of the alveolar bone remodeling. Orthod Craniofacial Res 12:289–298. https://doi.org/10.1111/j.1601-6343.2009.01464.x
Fujita S, Yamaguchi M, Utsunomiya T et al (2008) Low-energy laser stimulates tooth movement velocity via expression of RANK and RANKL. Orthod Craniofacial Res 11:143–155. https://doi.org/10.1111/j.1601-6343.2008.00423.x
Marquezan M, Bolognese AM, Araújo MTDS (2010) Effects of two low-intensity laser therapy protocols on experimental tooth movement. Photomed Laser Surg 28:757–762. https://doi.org/10.1089/pho.2009.2694
Cossetin E, Janson G, De CMGF et al (2013) Influence of low-level laser on bone remodeling during induced tooth movement in rats. Angle Orthod 83:1015–1021. https://doi.org/10.2319/100812-789.1
Ekizer A, Uysal T, Güray E, Akkuş D (2015) Effect of LED-mediated-photobiomodulation therapy on orthodontic tooth movement and root resorption in rats. Lasers Med Sci:779–785. https://doi.org/10.1007/s10103-013-1405-3
Vasconcelos EC, Henriques JF, Sousa MV, de Oliveira RC, Consolaro A, Pinzan A, Henriques FPBA (2016) Low-level laser action on orthodontically induced root resorption: histological and histomorphometric evaluation. J Lasers Med Sci 7:146–151
Rodrigo SM, Cunha A, Pozza DH, Blaya DS, Moraes JFWJ et al (2009) Analysis of the systemic effect of red and infrared laser therapy on wound repair. Photomed Laser Surg 27:929–935
Shirazi M, Ahmad Akhoundi MS, Javadi E et al (2015) The effects of diode laser (660nm) on the rate of tooth movements: an animal study. Lasers Med Sci:713–718. https://doi.org/10.1007/s10103-013-1407-1
Acknowledgements
The authors thank FAPESP (grant # 2013/06079-8) for financial support and Selly S. Suzuki thanks CAPES for scholarship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This research was conducted in accordance with the ethical principles of animal experimentation and the Brazilian norms for the practical, educational, and scientific uses of vivisection. The Animal Research and Ethic Committee of IPEN/CNEN-SP evaluated and approved this study (Animal Care and Use Committee IPEN-CNEN/SP #100/12).
Informed consent
No informed consent was needed in this study.
Rights and permissions
About this article
Cite this article
Suzuki, S.S., Garcez, A.S., Reese, P.O. et al. Effects of corticopuncture (CP) and low-level laser therapy (LLLT) on the rate of tooth movement and root resorption in rats using micro-CT evaluation. Lasers Med Sci 33, 811–821 (2018). https://doi.org/10.1007/s10103-017-2421-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-017-2421-5