Abstract
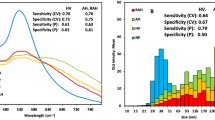
Higher blood pressure level and poor glycemic control in diabetic patients are considered progression factors that cause faster decline in kidney functions leading to kidney damage. The present study aimed to develop a quantification model of biomarkers creatinine, urea, and glucose by means of selected peaks of these compounds, measured by Raman spectroscopy, and to estimate the concentration of these analytes in the urine of normal subjects (G_N), diabetic patients with hypertension (G_WOL) patients with chronic renal failure doing dialysis (G_D). Raman peak intensities at 680 cm−1 (creatinine), 1004 cm−1 (urea), and 1128 cm−1 (glucose) from normal, diabetic, and hypertensive and doing dialysis patients, obtained with a dispersive 830 nm Raman spectrometer, were estimated through Origin software. Spectra of creatinine, urea, and glucose diluted in water were also obtained, and the same peaks were evaluated. A discrimination model based on Mahalanobis distance was developed. It was possible to determine the concentration of creatinine, urea, and glucose by means of the Raman peaks of the selected biomarkers in the urine of the groups G_N, G_WOL, and G_D (r = 0.9). It was shown that the groups G_WOL and G_D had lower creatinine and urea concentrations than the group G_N (p < 0.05). The classification model based on Mahalanobis distance applied to the concentrations of creatinine, urea, and glucose presented a correct classification of 89% for G_N, 86% for G_WOL, and 79% for G_D. It was possible to obtain quantitative information regarding important biomarkers in urine for the assessment of renal impairment in patients with diabetes and hypertension, and this information can be correlated with clinical criteria for the diagnosis of chronic kidney disease.





Similar content being viewed by others
References
Eknoyan G, Lameire N, Barsoum R, Eckardt KU, Levin A, Locatelli F et al (2004) The burden of kidney disease: improving global outcomes. Kidney Int 66:1310–1314
Sesso RCC, Lopes AA, Thomé FS, Lugon JR, Santos DR (2011) Chronic dialysis in Brazil—report of the Brazilian dialysis census. J Bras Nefrol 34:272–277
Hall JE (2011) Guyton and hall textbook of medical physiology, 12th edn. Elsevier Saunders, Philadelphia
Kumar V, Abbas AK, Aster JC (2014) Robbins & Cotran pathologic basis of disease, 9th edn. Elsevier Saunders, Philadelphia
National Kidney Foundation (2003) K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification and stratification. Am J Kidney Dis 39:1–266
Bishop ML, Fody EP, Shoeff LE (2013) Clinical chemistry: principles, techniques, and correlations, 7th edn. Lippincott Williams & Wilkins, Philadelphia
Nelson DL, Cox MM (2008) Lehninger principles of biochemistry, 5th edn. W.H. Freeman, New York
Apps DK, Cohen BB, Steel CM (1992) Biochemistry: a concise text for medical students, 5th edn. Bailliere Tindall, London
Assessment of kidney function serum creatinine, BUN, and GFR, Retrieved Spring, 2008. Available at http://www.uptodate.com. Accessed 04 Dec 2014
Jaffe M (1986) Uber den niederschlag welchen pikrinsaure in normalen harn erzeugt und uber eine neue reaktion des kreatinins. Hoppe Seyler's Z Physiol Chem 10:391–400
Oh MS (2011) Evaluation of renal function, water, electrolytes and acid-base balance. In: McPerson RA, Pincus MR (eds) Henry's clinical diagnosis and management by laboratory methods, 22nd edn. Saunders Elsevier, Philadelphia
Bastos MG, Kirsztajn GM (2011) Chronic kidney disease: importance of early diagnosis, immediate referral and structured interdisciplinary approach to improve outcomes in patients not yet on dialysis. J Bras Nefrol 22:93–108
Hanlon EB, Manoharan R, Koo TW, Shafer KE, Motz JT, Fitzmaurice M et al (2000) Prospects for in vivo Raman spectroscopy. Phys Med Biol 45:R1–R59
De Almeida ML, Saatkamp CJ, Fernandes AB, Pinheiro AL, Silveira L (2016) Estimating the concentration of urea and creatinine in the human serum of normal and dialysis patients through Raman spectroscopy. Lasers Med Sci 31:1415–1423
Silveira L, Borges RC, Navarro RS, Giana HE, Zângaro RA, Pacheco MT, Fernandes AB (2017) Quantifying glucose and lipid components in human serum by Raman spectroscopy and multivariate statistics. Lasers Med Sci (in press)
McMurdy JW, Berger AJ (2003) Raman spectroscopy-based creatinine measurement in urine samples from a multipatient population. Appl Spectrosc 57:522–525
Saatkamp CJ, de Almeida ML, Bispo JA, Pinheiro AL, Fernandes AB, Silveira L (2016) Quantifying creatinine and urea in human urine through Raman spectroscopy aiming at diagnosis of kidney disease. J Biomed Opt 21:37001
Premasiri WR, Clarke RH, Womble ME (2001) Urine analysis by laser Raman spectroscopy. Lasers Surg Med 28:330–334
Teo BW, Loh PT, Wong WK, Ho PJ, Choi KP, Toh QC, Xu H, Saw S, Lau T, Sethi S, Lee EJ (2015) Spot urine estimations are equivalent to 24-hour urine assessments of urine protein excretion for predicting clinical outcomes. Int J Nephrol 2015:156484
Xin G, Wang M, Jiao LL, Xu GB, Wang HY (2004) Protein-to-creatinine ratio in spot urine samples as a predictor of quantitation of proteinuria. Clin Chim Acta 350:35–39
Park C, Kim K, Choi J, Park K (2007) Classification of glucose concentration in diluted urine using the low-resolution Raman spectroscopy and kernel optimization methods. Physiol Meas 28:583–593
Wang H, Malvadkar N, Koytek S, Bylander J, Reeves WB, Demirel MC (2010) Quantitative analysis of creatinine in urine by metalized nanostructured parylene. J Biomed Opt 15:027004
Li M, Du Y, Zhao F, Zeng J, Mohan C, Shih WC (2015) Reagent- and separation-free measurements of urine creatinine concentration using stamping surface enhanced Raman scattering (S-SERS). Biomed Opt Express 6:849–858
Bispo JA, Vieira EES, Silveira L, Fernandes AB (2013) Correlating the amount of urea, creatinine, and glucose in urine from patients with diabetes mellitus and hypertension with the risk of developing renal lesions by means of Raman spectroscopy and principal component analysis. J Biomed Opt 18:1–8
Ciaccio EJ, Dunn SM, Akay M (1994) Biosignal pattern-recognition and interpretation systems. IEEE Eng Med Biol 13:129–135
The MathWorks Inc (2016) Documentation. Classify. The Mathworks Inc. https://www.mathworks.com/help/stats/classify.html. Accessed 20 Oct 2016
Filho AC, Silveira L, Yanai AL, Fernandes AB (2015) Raman spectroscopy for a rapid diagnosis of sickle cell disease in human blood samples: a preliminary study. Lasers Med Sci 30:247–253
Acknowledgments
L. Silveira Jr. thanks the FAPESP (São Paulo Research Foundation) for the partial financial support (process no. 2009/01788-5) and CNPq (National Council for Scientific and Technological Development) for the Productivity Fellowship (process no. 305680/2014-5). E. E. S. Vieira and J. A. M. Bispo thank the Regional Public Hospital of Western Pará and Santarém Municipal Hospital for authorizing this research in the Nephrology Clinic.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Role of funding sources
The project has been supported in part by a public funding agency (São Paulo Research Foundation—FAPESP), Process FAPESP no. 2009/01788-5, that allowed to purchase the Raman spectrometer.
Ethical approval
This study was approved by Research Ethics Committee from UNICASTELO (protocols nos. 64116 and 8926).
Informed consent
All volunteers agreed and signed an informed consent form to participate this study.
Rights and permissions
About this article
Cite this article
de Souza Vieira, E.E., Bispo, J.A.M., Silveira, L. et al. Discrimination model applied to urinalysis of patients with diabetes and hypertension aiming at diagnosis of chronic kidney disease by Raman spectroscopy. Lasers Med Sci 32, 1605–1613 (2017). https://doi.org/10.1007/s10103-017-2288-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-017-2288-5