Abstract
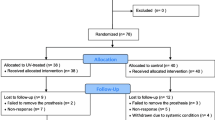
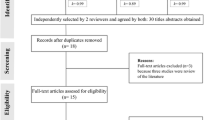
The purpose of the present study is to evaluate the effects of low-level laser therapy on the osseointegration process by comparing resonance frequency analysis measurements performed at implant placement and after 30 days and micro-computed tomography images in irradiated vs nonirradiated rabbits. Fourteen male New Zealand rabbits were randomly divided into two groups of seven animals each, one control group (nonirradiated animals) and one experimental group that received low-level laser therapy (Thera Lase®, aluminum-gallium-arsenide laser diode, 10 J per spot, two spots per session, seven sessions, 830 nm, 50 mW, CW, Ø 0.0028 cm2). The mandibular left incisor was surgically extracted in all animals, and one osseointegrated implant was placed immediately afterward (3.25ø × 11.5 mm; NanoTite, BIOMET 3i). Resonance frequency analysis was performed with the Osstell® device at implant placement and at 30 days (immediately before euthanasia). Micro-computed tomography analyses were then conducted using a high-resolution scanner (SkyScan 1172 X-ray Micro-CT) to evaluate the amount of newly formed bone around the implants. Irradiated animals showed significantly higher implant stability quotients at 30 days (64.286 ± 1.596; 95 % confidence interval (CI) 60.808–67.764) than controls (56.357 ± 1.596; 95 %CI 52.879–59.835) (P = .000). The percentage of newly formed bone around the implants was also significantly higher in irradiated animals (75.523 ± 8.510; 95 %CI 61.893–89.155) than in controls (55.012 ± 19.840; 95 %CI 41.380–68.643) (P = .027). Laser therapy, based on the irradiation protocol used in this study, was able to provide greater implant stability and increase the volume of peri-implant newly formed bone, indicating that laser irradiation effected an improvement in the osseointegration process.



Similar content being viewed by others
References
Muller F (2014) Interventions for edentate elders—what is the evidence? Gerodontology 31(Suppl 1):44–51. doi:10.1111/ger.12083
Chen ST, Buser D (2014) Esthetic outcomes following immediate and early implant placement in the anterior maxilla—a systematic review. Int J Oral Maxillofac Implants 29 Suppl:186–215. doi:10.11607/jomi.2014suppl.g3.3
Carlsson L, Rostlund T, Albrektsson B, Albrektsson T, Branemark PI (1986) Osseointegration of titanium implants. Acta Orthop Scand 57:285–289
Coelho RC, Zerbinati LP, de Oliveira MG, Weber JB (2014) Systemic effects of LLLT on bone repair around PLLA-PGA screws in the rabbit tibia. Lasers Med Sci 29:703–708. doi:10.1007/s10103-013-1384-4
de Vasconcellos LM, Barbara MA, Deco CP, Junqueira JC, do Prado RF, Anbinder AL, de Vasconcellos LG, Cairo CA, Carvalho YR (2014) Healing of normal and osteopenic bone with titanium implant and low-level laser therapy (GaAlAs): a histomorphometric study in rats. Lasers Med Sci 29:575–580. doi:10.1007/s10103-013-1326-1
Demirkol N, Sari F, Bulbul M, Demirkol M, Simsek I, Usumez A (2015) Effectiveness of occlusal splints and low-level laser therapy on myofascial pain. Lasers Med Sci 30:1007–1012. doi:10.1007/s10103-014-1522-7
Fronza B, Somacal T, Mayer L, de Moraes JF, de Oliveira MG, Weber JB (2013) Assessment of the systemic effects of low-level laser therapy (LLLT) on thyroid hormone function in a rabbit model. Int J Oral Maxillofac Surg 42:26–30. doi:10.1016/j.ijom.2012.06.017
Gasperini G, Rodrigues de Siqueira IC, Rezende Costa L (2014) Does low-level laser therapy decrease swelling and pain resulting from orthognathic surgery? Int J Oral Maxillofac Surg 43:868–873. doi:10.1016/j.ijom.2014.02.015
Park JB, Ahn SJ, Kang YG, Kim EC, Heo JS, Kang KL (2015) Effects of increased low-level diode laser irradiation time on extraction socket healing in rats. Lasers Med Sci 30:719–726. doi:10.1007/s10103-013-1402-6
Tang E, Arany P (2013) Photobiomodulation and implants: implications for dentistry. J Periodontal Implant Sci 43:262–268. doi:10.5051/jpis.2013.43.6.262
Mayer L, Gomes FV, Carlsson L, Gerhardt-Oliveira M (2015) Histologic and resonance frequency analysis of peri-implant bone healing after low-level laser therapy: an in vivo study. Int J Oral Maxillofac Implants 30:1028–1035. doi:10.11607/jomi.3382
Khadra M, Ronold HJ, Lyngstadaas SP, Ellingsen JE, Haanaes HR (2004) Low-level laser therapy stimulates bone-implant interaction: an experimental study in rabbits. Clin Oral Implants Res 15:325–332. doi:10.1111/j.1600-0501.2004.00994.x
Maluf AP, Maluf RP, Brito Cda R, Franca FM, De Brito RB Jr (2010) Mechanical evaluation of the influence of low-level laser therapy in secondary stability of implants in mice shinbones. Lasers Med Sci 25:693–698. doi:10.1007/s10103-010-0778-9
Primo BT, da Silva RC, Grossmann E, Miguens SA Jr, Hernandez PA, Silva AN Jr (2013) Effect of surface roughness and low-level laser therapy on removal torque of implants placed in rat femurs. J Oral Implantol 39:533–538. doi:10.1563/AAID-JOI-D-10-00141
Campanha BP, Gallina C, Geremia T, Loro RC, Valiati R, Hubler R, de Oliveira MG (2010) Low-level laser therapy for implants without initial stability. Photomed Laser Surg 28:365–369. doi:10.1089/pho.2008.2429
Rea M, Lang NP, Ricci S, Mintrone F, Gonzalez Gonzalez G, Botticelli D (2015) Healing of implants installed in over- or under-prepared sites—an experimental study in dogs. Clin Oral Implants Res 26:442–446. doi:10.1111/clr.12390
Friedmann A, Friedmann A, Grize L, Obrecht M, Dard M (2014) Convergent methods assessing bone growth in an experimental model at dental implants in the minipig. Ann Anat 196:100–107. doi:10.1016/j.aanat.2014.02.001
Lee SW, Hahn BD, Kang TY, Lee MJ, Choi JY, Kim MK, Kim SG (2014) Hydroxyapatite and collagen combination-coated dental implants display better bone formation in the peri-implant area than the same combination plus bone morphogenetic protein-2-coated implants, hydroxyapatite only coated implants, and uncoated implants. J Oral Maxillofac Surg 72:53–60. doi:10.1016/j.joms.2013.08.031
Ostman PO, Hellman M, Wendelhag I, Sennerby L (2006) Resonance frequency analysis measurements of implants at placement surgery. Int J Prosthodont 19:77–83, discussion 84
Pagliani L, Sennerby L, Petersson A, Verrocchi D, Volpe S, Andersson P (2013) The relationship between resonance frequency analysis (RFA) and lateral displacement of dental implants: an in vitro study. J Oral Rehabil 40:221–227. doi:10.1111/joor.12024
Parsa A, Ibrahim N, Hassan B, van der Stelt P, Wismeijer D (2015) Bone quality evaluation at dental implant site using multislice CT, micro-CT, and cone beam CT. Clin Oral Implants Res 26:e1–7. doi:10.1111/clr.12315
Anil S, Cuijpers VM, Preethanath RS, Aldosari AA, Jansen JA (2013) Osseointegration of oral implants after delayed placement in rabbits: a microcomputed tomography and histomorphometric study. Int J Oral Maxillofac Implants 28:1506–1511. doi:10.11607/jomi.3133
Finelle G, Papadimitriou DE, Souza AB, Katebi N, Gallucci GO, Araujo MG (2015) Peri-implant soft tissue and marginal bone adaptation on implant with non-matching healing abutments: micro-CT analysis. Clin Oral Implants Res 26:e42–46. doi:10.1111/clr.12328
Gomes FV, Mayer L, Massotti FP, Baraldi CE, Ponzoni D, Webber JB, de Oliveira MG (2015) Low-level laser therapy improves peri-implant bone formation: resonance frequency, electron microscopy, and stereology findings in a rabbit model. Int J Oral Maxillofac Surg 44:245–251. doi:10.1016/j.ijom.2014.09.010
Ohta K, Takechi M, Minami M, Shigeishi H, Hiraoka M, Nishimura M, Kamata N (2010) Influence of factors related to implant stability detected by wireless resonance frequency analysis device. J Oral Rehabil 37:131–137. doi:10.1111/j.1365-2842.2009.02032.x
Eslamian L, Borzabadi-Farahani A, Hassanzadeh-Azhiri A, Badiee MR, Fekrazad R (2014) The effect of 810-nm low-level laser therapy on pain caused by orthodontic elastomeric separators. Lasers Med Sci 29:559–564. doi:10.1007/s10103-012-1258-1
Massotti FP, Gomes FV, Mayer L, de Oliveira MG, Baraldi CE, Ponzoni D, Puricelli E (2015) Histomorphometric assessment of the influence of low-level laser therapy on peri-implant tissue healing in the rabbit mandible. Photomed Laser Surg 33:123–128. doi:10.1089/pho.2014.3792
Mangione F, Meleo D, Talocco M, Pecci R, Pacifici L, Bedini R (2013) Comparative evaluation of the accuracy of linear measurements between cone beam computed tomography and 3D microtomography. Ann Ist Super Sanita 49:261–265. doi:10.4415/ANN_13_03_05
Pyo SW, Kim YM, Kim CS, Lee IS, Park JU (2014) Bone formation on biomimetic calcium phosphate-coated and zoledronate-immobilized titanium implants in osteoporotic rat tibiae. Int J Oral Maxillofac Implants 29:478–484. doi:10.11607/jomi.3423
Bouxsein ML, Boyd SK, Christiansen BA, Guldberg RE, Jepsen KJ, Müller R (2010) Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J Bone Miner Res 25:1468–1486. doi:10.1002/jbmr.141
Le BT, Borzabadi-Farahani A (2014) Simultaneous implant placement and bone grafting with particulate mineralized allograft in sites with buccal wall defects, a three-year follow-up and review of literature. J Craniomaxillofac Surg 42:552–559. doi:10.1016/j.jcms.2013.07.026
Lopes CB, Pinheiro AL, Sathaiah S, Duarte J, Cristinamartins M (2005) Infrared laser light reduces loading time of dental implants: a Raman spectroscopic study. Photomed Laser Surg 23:27–31
Khadra M (2005) The effect of low level laser irradiation on implant-tissue interaction. In vivo and in vitro studies. Swed Dent J Suppl 172:1–63
Kim YD, Kim SS, Hwang DS, Kim SG, Kwon YH, Shin SH, Kim UK, Kim JR, Chung IK (2007) Effect of low-level laser treatment after installation of dental titanium implant-immunohistochemical study of RANKL, RANK, OPG: an experimental study in rats. Lasers Surg Med 39:441–450
Lopes CB, Pinheiro AL, Sathaiah S, Da Silva NS, Salgado MA (2007) Infrared laser photobiomodulation (lambda 830 nm) on bone tissue around dental implants: a Raman spectroscopy and scanning electronic microscopy study in rabbits. Photomed Laser Surg 25:96–101
Boldrini C, de Almeida JM, Fernandes LA, Ribeiro FS, Garcia VG, Theodoro LH, Pontes AE (2013) Biomechanical effect of one session of low-level laser on the bone-titanium implant interface. Lasers Med Sci 28:349–352. doi:10.1007/s10103-012-1167-3
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial disclosure
The authors have no financial relationships relevant to this article to disclose.
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted.
Rights and permissions
About this article
Cite this article
Mayer, L., Gomes, F.V., de Oliveira, M.G. et al. Peri-implant osseointegration after low-level laser therapy: micro-computed tomography and resonance frequency analysis in an animal model. Lasers Med Sci 31, 1789–1795 (2016). https://doi.org/10.1007/s10103-016-2051-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-016-2051-3