Abstract
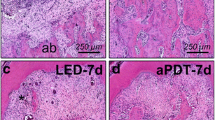
The aim of this study was to compare the use of antimicrobial photodynamic therapy (aPDT) as an adjunct to scaling and root planing (SRP) in the treatment of experimentally induced periodontitis in female rats that were systemically treated with or without nicotine. Female rats (n = 180) were divided into two groups: vehicle administration (Veh) and nicotine administration (Nic). Mini-pumps containing either vehicle or nicotine were implanted in the rats 30 days before the induction of experimental periodontitis (EP). EP was induced by placing a cotton ligature around the left mandibular first molar. After 7 days, the ligature was removed, and the rats were randomly divided into three treatment subgroups: SRP (only SRP), DL (SRP plus diode laser), and aPDT (SRP plus aPDT). The aPDT consisted of phenothiazine photosensitizer deposition followed by diode laser irradiation. Ten rats from each subgroup were euthanized at 7, 15, and 30 days after treatment. Alveolar bone loss (ABL) in the furcation region was evaluated using histological, histometric, and immunohistochemical analyses. The rats that were treated with nicotine showed more ABL compared to those treated with vehicle. In both the Veh and Nic groups, SRP plus aPDT treatment resulted in reduced ABL, smaller numbers of both TRAP- and RANKL-positive cells, and higher numbers of PCNA-positive cells compared to SRP treatment alone. aPDT was an effective adjunctive therapy for the treatment of periodontitis in female rats regardless of whether they received nicotine.






Similar content being viewed by others
References
Johannsen A, Susin C, Gustafsson A (2014) Smoking and inflammation: evidence for a synergistic role in chronic disease. Periodontol 64:111–126
Hebert R (2003) What’s new in nicotine & tobacco research? Nicotine Tob Res 5:427–433
Benowitz NL, Lessov-Schlaggar CN, Swan GE, Jacob P (2006) 3rd. Female sex and oral contraceptive use accelerate nicotine metabolism. Clin Pharmacol Ther 79:480–488
Johnstone E, Benowitz N, Cargill A et al (2006) Determinants of the rate of nicotine metabolism and effects on smoking behavior. Clin Pharmacol Ther 80:319–330
Higashi E, Fukami T, Itoh M et al (2007) Human CYP2A6 is induced by estrogen via estrogen receptor. Drug Metab Dispos 35:1935–1941
Nakajima M, Yamamoto T, Nunoya K et al (1996) Role of human cytochrome P4502A6 in C-oxidation of nicotine. Drug Metab Dispos 24:1212–1217
Jensen J, Christiansen C, Rødbro P (1985) Cigarette smoking, serum estrogens, and bone loss during hormone-replacement therapy early after menopause. N Engl J Med 17(313):973–975
Mueck AO, Seeger H (2005) Smoking, estradiol metabolism and hormone replacement therapy. Curr Med Chem Cardiovasc Hematol Agents 3:45–54
Ma L, Zwahlen RA, Zheng LW, Sham MH (2011) Influence of nicotine on the biological activity of rabbit osteoblasts. Clin Oral Implants Res 22:338–342
Kim SJ, Kim HJ, Lee SJ, Park YJ, Lee J, You HK (2006) Effects of nicotine on proliferation and osteoblast differentiation in human alveolar bone marrow-derived mesenchymal stem cells. Acta Biochim Biophys Sin (Shanghai) 38:874–882
Henemyre CL, Scales DK, Hokett SD et al (2003) Nicotine stimulates osteoclast resorption in a porcine marrow cell model. J Periodontol 74:1440–1446
Tanaka H, Tanabe N, Shoji M et al (2006) Nicotine and lipopolysaccharide stimulate the formation of osteoclast-like cells by increasing macrophage colony-stimulating factor and prostaglandin E2 production by osteoblasts. Life Sci 78:1733–1740
Jimi E, Shuto T, Koga T (1995) Macrophage colony-stimulating factor and interleukin-1a maintain the survival of osteoclast-like cells. Endocrinology 136:808–811
Lee SK, Chung JH, Choi SC et al (2013) Sodium hydrogen sulfide inhibits nicotine and lipopolysaccharide-induced osteoclastic differentiation and reversed osteoblastic differentiation in human periodontal ligament cells. J Cell Biochem 114:1183–1193
Theoleyre S, Wittrant Y, Tat SK, Fortun Y, Redini F, Heymann D (2004) The molecular triad OPG/RANK/RANKL:Involvement in the orchestration of pathophysiological bone remodeling. Cytokine Growth Factor Rev 15:457–475
Wu LZ, Duan DM, Liu YF, Ge X, Zhou ZF, Wang XJ (2013) Nicotine favors osteoclastogenesis in human periodontal ligament cells co-cultured with CD4(+) T cells by upregulating IL-1β. Int J Mol Med 31:938–942
Lee HJ, Pi SH, Kim Y et al (2009) Effects of nicotine on antioxidant defense enzymes and RANKL expression in human periodontal ligament cells. J Periodontol 80:1281–1288
Sorkhdini P, Moslemi N, Jamshidi S, Jamali R, Amirzargar AA, Fekrazad R (2013) Effect of hydrosoluble chlorine-mediated antimicrobial photodynamic therapy on clinical parameters and cytokine profile in ligature-induced periodontitis in dogs. J Periodontol 84:793–800
Oda S, Nitta H, Setoguchi T, Izumi Y, Ishikawa I (2004) Current concepts and advances in manual and power-driven instrumentation. Periodontol 36:45–58
Braham P, Herron C, Street C, Darveau R (2009) Antimicrobial photodynamic therapy may promote periodontal healing through multiple mechanisms. J Periodontol 80:1790–1798
Garcia VG, Fernandes LA, Macarini VC et al (2011) Treatment of experimental periodontal disease with antimicrobial photodynamic therapy in nicotine-modified rats. J Clin Periodontol 38:1106–1114
Garcia VG, Gualberto Júnior EC, Fernandes LA et al (2013) Adjunctive antimicrobial photodynamic treatment of experimentally induced periodontitis in rats with ovariectomy. J Periodontol 84:556–565
Yamano S, Berley JA, Kuo WP et al (2010) Effects of nicotine on gene expression and osseointegration in rats. Clin Oral Implants Res 21:1353–1359
Garcia VG, Longo M, Gualberto Júnior EC et al (2014) Effect of the concentration of phenothiazine photosensitizers in antimicrobial photodynamic therapy on bone loss and the immune inflammatory response of induced periodontitis in rats. J Periodontal Res 49:584–594
Ström JO, Theodorsson E, Theodorsson A (2008) Order of magnitude differences between methods for maintaining physiological 17beta-oestradiol concentrations in ovariectomized rats. Scand J Clin Lab Invest 68:814–822
Raval AP, Hirsch N, Dave KR, Yavagal DR, Bramlett H, Saul I (2011) Nicotine and strogen synergistically exacerbate cerebral ischemic injury. Neuroscience 181:216–225
Bosco AF, Bonfante S, de Almeida JM, Luize DS, Nagata MJ, Garcia VG (2007) A histologic and histometric assessment of the influence of nicotine on alveolar bone loss in rats. J Periodontol 78:527–532
Hapidin H, Othman F, Soelaiman IN, Shuid AN, Luke DA, Mohamed N (2007) Negative effects of nicotine on bone-resorbing cytokines and bone histomorphometric parameters in male rats. J Bone Miner Metab 25:93–98
Müller Campanile VS, Giannopoulou C, Campanile G, Cancela JA, Mombelli A (2015) Single or repeated antimicrobial photodynamic therapy as adjunct to ultrasonic debridement in residual periodontal pockets: clinical, microbiological, and local biological effects. Lasers Med Sci 30:27–34
Tardivo JP, Del Giglio A, de Oliveira CS et al (2005) Methylene blue in photodynamic therapy: from basic mechanisms to clinical applications. Photodiagnosis Photododyn Ther 2:175–191
Ochsner M (1997) Photophysical and photobiological processes in the photodynamic therapy of tumors. J Photochem Photobiol B 39:1–18
Kömerik N, Nakanishi H, MacRobert AJ, Henderson B, Speight P, Wilson M (2003) In vivo killing of Porphyromonas gingivalis by toluidine blue-mediated photosensitization in an animal model. Antimicrob Agents Chemother 47:932–940
Wainwright M (1998) Photodynamic antimicrobial chemotherapy (PACT). J Antimicrob Chemother 42:13–28
Usacheva M, Teichert MC, Biel MA (2001) Comparison of the methylene blue and toluidine blue photobactericidal efficacy against gram-positive and gram-negative microorganisms. Lasers Surg Med 29:165–173
Komerik N, Wilson M, Poole S (2000) The effect of photodynamic action on two virulence factors of gram-negative bacteria. Photochem Photobiol 72:676–680
Asagiri M, Takayanagi H (2007) The molecular understanding of osteoclast differentiation. Bone 40:251–264
Cochran DL (2008) Inflammation and bone loss in periodontal disease. J Periodontol 79:1569–1576
Graves DT, Cochran D (2003) The contribution of interleukin-1 and tumor necrosis factor to periodontal tissue destruction. J Periodontol 74:391–401
Lerner UH (2006) Inflammation-induced bone remodeling in periodontal disease and the influence of postmenopausal osteoporosis. J Dent Res 85:596–607
Boyle WJ, Simonet WS, Lacey DL (2003) Osteoclast differentiation and activation. Nature 423:337–342
Séguier S, Souza SL, Sverzut AC et al (2010) Impact of photodynamic therapy on inflammatory cells during human chronic periodontitis. J Photochem Photobiol B 101:348–354
Acknowledgments
This study was financially supported by the São Paulo Research Foundation (FAPESP), São Paulo, SP, Brazil (FAPESP processes no. 2011/00936-0 and no. 2010/15094-2). The authors are grateful to Prof. Dr. Guilherme de Paula Nogueira (Faculty of Veterinary Medicine, UNESP, Araçatuba, SP, Brazil) for his guidance in the use of radioimmunoassay. The authors report no conflicts of interest related to this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All protocols were approved by the Institutional Review Board of Araçatuba Dental School, São Paulo State University, Araçatuba, São Paulo, Brazil (no. 2010/005074).
Rights and permissions
About this article
Cite this article
Gualberto, E.C., Theodoro, L.H., Longo, M. et al. Antimicrobial photodynamic therapy minimizes the deleterious effect of nicotine in female rats with induced periodontitis. Lasers Med Sci 31, 83–94 (2016). https://doi.org/10.1007/s10103-015-1820-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-015-1820-8