Abstract
Purpose
To identify the predictors of morbidity and mortality in matched COVID-19 positive and negative patients who were septic with Gram positive or Gram negative infections.
Methods
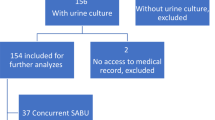
We conducted a retrospective review, from March to October 2020, of matched septic patients at five Hackensack Meridian Health hospitals who had bacteremia with Staphylococcus aureus, Klebsiella pneumoniae or Escherichia coli with and without COVID-19. We extracted patient demographics, comorbidities and clinical outcomes data using ICD-10 codes. Bacterial isolates were compared by whole genome sequencing analysis. Multivariate logistic regression was used to analyze independent predictors of morbidity and mortality.
Results
A total of 208 patients were grouped by positive bloodstream infection (BSI) with COVID-19 (n = 104) and without COVID-19 (n = 104). Most patients were over age 50 (90% vs. 89%) and Caucasian (78% vs. 86%). Inpatient mortality was higher in patients with COVID-19 for both GP (35% vs. 8%, p < 0.05) and GN (28% vs. 10%, p < 0.05) BSIs. Patients with Gram positive (GP) BSIs had a significant increase in mortality risk (OR 4.5, CI 1.4–14.5, p < 0.05) in contrast to those with Gram negative (GN) infections (OR 0.4, CI 0.4–4.0, p = 0.4).
Conclusion
Concurrent COVID-19 infection is associated with a significant increase in morbidity and mortality in patients with GP and GN BSIs. Patients with S. aureus BSIs with COVID-19 are more likely to develop shock and respiratory failure and have higher rates and odds of mortality than those without COVID-19. These findings provide an essential insight into the care of these patients, especially those co-infected with Staphylococcus aureus.


Similar content being viewed by others
Data availability
The datasets in this paper will be made available from the corresponding authors upon requests.
References
WHO Coronavirus (COVID-19) Dashboard. World Health Organization https://covid19.who.int/
Bonazzetti C, Morena V, Giacomelli A et al (2021) Unexpectedly high frequency of enterococcal bloodstream infections in coronavirus disease 2019 patients admitted to an Italian ICU: an observational study. Crit Care Med 49(1):e31–e40. https://doi.org/10.1097/CCM.0000000000004748
Puzniak L, Finelli L, Yu KC et al (2021) A multicenter analysis of the clinical microbiology and antimicrobial usage in hospitalized patients in the US with or without COVID-19. BMC Infect Dis 21(1):227. https://doi.org/10.1186/s12879-021-05877-3
Bhatt PJ, Shiau S, Brunetti L et al (2021) Risk factors and outcomes of hospitalized patients with severe coronavirus disease 2019 (COVID-19) and secondary bloodstream infections: a multicenter case-control study. Clin Infect Dis Off Publ Infect Dis Soc Am 72(12):e995–e1003. https://doi.org/10.1093/cid/ciaa1748
Adalbert JR, Varshney K, Tobin R, Pajaro R (2021) Clinical outcomes in patients co-infected with COVID-19 and Staphylococcus aureus: a scoping review. BMC Infect Dis 21(1):985. https://doi.org/10.1186/s12879-021-06616-4
Nori P, Cowman K, Chen V et al (2021) Bacterial and fungal coinfections in COVID-19 patients hospitalized during the New York City pandemic surge. Infect Control Hosp Epidemiol 42(1):84–88. https://doi.org/10.1017/ice.2020.368
Goto M, Al-Hasan MN (2013) Overall burden of bloodstream infection and nosocomial bloodstream infection in North America and Europe. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis 19(6):501–509. https://doi.org/10.1111/1469-0691.12195
Viscoli C (2016) Bloodstream Infections: the peak of the iceberg. Virulence 7(3):248–251. https://doi.org/10.1080/21505594.2016.1152440
Giacobbe DR, Battaglini D, Ball L et al (2020) Bloodstream infections in critically ill patients with COVID-19. Eur J Clin Invest 50(10):e13319. https://doi.org/10.1111/eci.13319
Bolger AM, Lohse M, Usadel B (2014) Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinforma Oxf Engl 30(15):2114–2120. https://doi.org/10.1093/bioinformatics/btu170
Bankevich A, Nurk S, Antipov D et al (2012) SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J Comput Biol J Comput Mol Cell Biol 19(5):455–477. https://doi.org/10.1089/cmb.2012.0021
Gurevich A, Saveliev V, Vyahhi N, Tesler G (2013) QUAST: quality assessment tool for genome assemblies. Bioinforma Oxf Engl 29(8):1072–1075. https://doi.org/10.1093/bioinformatics/btt086
Seemann T. mlst Github https://github.com/tseemann/mlst
Jolley KA, Maiden MC (2010) BIGSdb: Scalable analysis of bacterial genome variation at the population level. BMC Bioinformatics 11(1):595. https://doi.org/10.1186/1471-2105-11-595
Feldgarden M, Brover V, Haft DH et al (2019) Validating the AMRFinder tool and resistance gene database by using antimicrobial resistance genotype-phenotype correlations in a collection of isolates. Antimicrob Agents Chemother. 63(11). https://doi.org/10.1128/AAC.00483-19
Zankari E, Hasman H, Cosentino S et al (2012) Identification of acquired antimicrobial resistance genes. J Antimicrob Chemother 67(11):2640–2644. https://doi.org/10.1093/jac/dks261
Seemann T. Snippy. https://github.com/tseemann/snippy
Arndt D, Grant JR, Marcu A et al (2016) PHASTER: a better, faster version of the PHAST phage search tool. Nucleic Acids Res 44(W1):W16-21. https://doi.org/10.1093/nar/gkw387
Kurtz S, Phillippy A, Delcher AL et al (2004) Versatile and open software for comparing large genomes. Genome Biol 5(2):R12. https://doi.org/10.1186/gb-2004-5-2-r12
Siguier P, Perochon J, Lestrade L, Mahillon J, Chandler M (2006) ISfinder: the reference centre for bacterial insertion sequences. Nucleic Acids Res 34(Database issue):D32-36. https://doi.org/10.1093/nar/gkj014
Croucher NJ, Page AJ, Connor TR et al (2015) Rapid phylogenetic analysis of large samples of recombinant bacterial whole genome sequences using Gubbins. Nucleic Acids Res 43(3):e15. https://doi.org/10.1093/nar/gku1196
Seemann T. snp-dists. https://github.com/tseemann/snp-dists
Pitout JDD, DeVinney R (2017) Escherichia coli ST131: a multidrug-resistant clone primed for global domination. F1000Research 6:F1000 Faculty Rev-195. https://doi.org/10.12688/f1000research.10609.1
Challagundla L, Luo X, Tickler IA et al (2018) Range Expansion and the Origin of USA300 North American Epidemic Methicillin-Resistant Staphylococcus aureus. mBio 9(1). https://doi.org/10.1128/mBio.02016-17
Kourtis AP, Hatfield K, Baggs J et al (2019) Vital signs: epidemiology and recent trends in methicillin-resistant and in methicillin-susceptible staphylococcus aureus bloodstream infections - United States. MMWR Morb Mortal Wkly Rep 68(9):214–219. https://doi.org/10.15585/mmwr.mm6809e1
Cusumano JA, Dupper AC, Malik Y et al (2020) Staphylococcus aureus bacteremia in patients infected with COVID-19: a case series. Open Forum Infect Dis 7(11):ofaa518. https://doi.org/10.1093/ofid/ofaa518
Yap FHY, Gomersall CD, Fung KSC et al (2004) Increase in methicillin-resistant Staphylococcus aureus acquisition rate and change in pathogen pattern associated with an outbreak of severe acute respiratory syndrome. Clin Infect Dis Off Publ Infect Dis Soc Am 39(4):511–516. https://doi.org/10.1086/422641
Morens DM, Taubenberger JK, Fauci AS (2008) Predominant role of bacterial pneumonia as a cause of death in pandemic influenza: implications for pandemic influenza preparedness. J Infect Dis 198(7):962–970. https://doi.org/10.1086/591708
Leung CH, Tseng HK, Wang WS, Chiang HT, Wu AYJ, Liu CP (2014) Clinical characteristics of children and adults hospitalized for influenza virus infection. J Microbiol Immunol Infect Wei Mian Yu Gan Ran Za Zhi 47(6):518–525. https://doi.org/10.1016/j.jmii.2013.06.002
Lew TWK, Kwek TK, Tai D et al (2003) Acute respiratory distress syndrome in critically ill patients with severe acute respiratory syndrome. JAMA 290(3):374–380. https://doi.org/10.1001/jama.290.3.374
Shi H, Han X, Jiang N et al (2020) Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis 20(4):425–434. https://doi.org/10.1016/S1473-3099(20)30086-4
Mehta AA, Haridas N, Belgundi P, Jose WM (2021) A systematic review of clinical and laboratory parameters associated with increased severity among COVID-19 patients. Diabetes Metab Syndr 15(2):535–541. https://doi.org/10.1016/j.dsx.2021.02.020
Qin C, Zhou L, Hu Z et al (2020) Dysregulation of immune response in patients with coronavirus 2019 (COVID-19) in Wuhan, China. Clin Infect Dis Off Publ Infect Dis Soc Am 71(15):762–768. https://doi.org/10.1093/cid/ciaa248
Ripa M, Galli L, Poli A et al (2021) Secondary infections in patients hospitalized with COVID-19: incidence and predictive factors. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis 27(3):451–457. https://doi.org/10.1016/j.cmi.2020.10.021
Diao B, Wang C, Tan Y et al (2020) Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID-19). Front Immunol 11:827. https://doi.org/10.3389/fimmu.2020.00827
Dupper AC, Malik Y, Cusumano JA et al (2022) Longer steroid treatment increases secondary bloodstream infection risk among patients with COVID-19 requiring intensive care. Infect Dis Clin Pract 30(4). https://journals.lww.com/infectdis/Fulltext/2022/07000/Longer_Steroid_Treatment_Increases_Secondary.7.aspx
Campochiaro C, Della-Torre E, Cavalli G et al (2020) Efficacy and safety of tocilizumab in severe COVID-19 patients: a single-centre retrospective cohort study. Eur J Intern Med 76:43–49. https://doi.org/10.1016/j.ejim.2020.05.021
Bengoechea JA, Bamford CG (2020) SARS-CoV-2, bacterial co-infections, and AMR: the deadly trio in COVID-19? EMBO Mol Med 12(7):e12560. https://doi.org/10.15252/emmm.202012560
Acknowledgements
We are grateful to the effort of the Microbiology Laboratory at Jersey Shore University Medical Center in supporting this study.
Funding
This work was funded by Merck’s Investigator Studies Program (MISP) SARS CoV-2/COVID-19 award MISP 60453 to B.N.K. and M.K. (“Drug resistance profiles of bacterial and fungal isolates from super-infections in hospitalized COVID-19 patients”).
Author information
Authors and Affiliations
Contributions
The corresponding author (B. Kreiswirth) and Drs. Rojtman and Kordalewska were involved in the research design, overseeing the study and editing the manuscript. The two co-first authors (Dar and Erickson) collected and analyzed the data in collaboration with Dr. Manca and prepared the initial draft of the manuscript. Dr. Lozy provided guidance in the statistical analysis. The other authors generated the laboratory data including the preparation, sequencing, and analysis of the strains.
Corresponding author
Ethics declarations
Ethics approval
This study was approved on 11/1/2021 by Hackensack Meridian Health Institutional Review Board (IRB) under protocol Pro2021-0519.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sophia Dar and Daniel Erickson are co-first authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dar, S., Erickson, D., Manca, C. et al. The impact of COVID on bacterial sepsis. Eur J Clin Microbiol Infect Dis 42, 1173–1181 (2023). https://doi.org/10.1007/s10096-023-04655-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-023-04655-0