Abstract
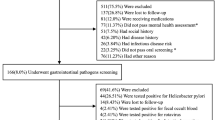
The safety of fecal microbiota transplantation (FMT) has been highlighted by extended-spectrum β-lactamase (ESBL)-producing Escherichia coli bacteremia transmitted from donors and acquisition of diarrheagenic E. coli (Shiga toxin-producing E. coli (STEC) and enteropathogenic E. coli (EPEC)) via FMT. The use of donor screening criteria to lower the risk of pathogen transmission via FMT is essential. This study aimed to demonstrate the outcomes of our strict donor screening program. This study was conducted at our FMT center between January 2019 and June 2022. Our donor screening program included an initial questionnaire and subsequent blood and stool testing. We further used selective culture for third-generation cephalosporin-resistant (3GCR) Enterobacterales and multiplex PCR to detect diarrheagenic E. coli in stools. The resistance mechanisms and sequence type of 3GCR Enterobacterales were determined. A total of 742 individuals were assessed, and 583 participants (78.6%) were excluded after questionnaire. Of the remaining 159 participants undergoing stool and blood tests, 37 participants were finally qualified (5.0%, 37/742). A high fecal carriage rate of ESBL-producing Enterobacterales (35.2%, 56/159), including E. coli (n=53) and Klebsiella pneumoniae (n=5), and diarrheagenic E. coli (31.4%, 50/159), including EPEC (n=41), enteroaggregative E. coli (n=11), enterotoxigenic E. coli (n=4), and STEC (n=1), was noted. CTX-M-79 and CTX-M-15 were dominant in E. coli and K. pneumoniae, respectively. The sequence types of the ESBL-producing strains were diverse. The screening for 3GCR Enterobacterales and diarrheagenic E. coli in stool is necessary. Our findings also support the effectiveness of multiplex PCR panels in FMT donor screening programs.

Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Hvas CL, Dahl Jørgensen SM, Jørgensen SP et al (2019) Fecal microbiota transplantation is superior to fidaxomicin for treatment of recurrent Clostridium difficile infection. Gastroenterology 156:1324–32.e3
van Prehn J, Reigadas E, Vogelzang EH et al (2021) European Society of Clinical Microbiology and Infectious Diseases: 2021 update on the treatment guidance document for Clostridioides difficile infection in adults. Clin Microbiol Infect 27(Suppl 2):S1–S21
Bakken JS, Borody T, Brandt LJ et al (2011) Treating Clostridium difficile infection with fecal microbiota transplantation. Clin Gastroenterol Hepatol 9(12):1044–9
DeFilipp Z, Bloom PP, Torres Soto M et al (2019) Drug-resistant E. coli bacteremia transmitted by fecal microbiota transplant. N Engl J Med 381:2043–2050
Zellmer C, Sater MRA, Huntley MH et al (2021) Shiga toxin-producing E. coli transmission via fecal microbiota transplant. Clin Infect Dis 72:e876–e880
OpenBiome. OpenBiome announces enhanced donor screening protocols following FDA alert. March 13, 2020. https://www.openbiome.org/press-releases/2020/3/12/openbiome-announces-enhanced-donor-screening-protocols-following-fda-alert. Accessed 7 December 2022
US Food and Drug Administration. Important safety alert regarding use of fecal microbiota for transplantation and risk of serious adverse reactions due to transmission of multi-drug resistant organisms. June 13, 2019. https://www.fda.gov/vaccines-blood-biologics/safety-availability-biologics/important-safety-alert-regarding-use-fecal-microbiota-transplantation-and-risk-serious-adverse. Accessed 7 December 2022
US Food and Drug Administration. Information pertaining to additional safety protections regarding use of fecal microbiota for transplantation - testing of stool donors for enteropathogenic Escherichia coli and Shigatoxin-producing Escherichia coli. April 6, 2020. https://www.fda.gov/vaccines-blood-biologics/safety-availability-biologics/information-pertaining-additional-safety-protections-regarding-use-fecal-microbiota-transplantation-0. Accessed 7 December 2022
Lin TC, Hung YP, Ko WC et al (2019) Fecal microbiota transplantation for Clostridium difficile infection in Taiwan: establishment and implementation. J Microbiol Immunol Infect 52:841–50
Woodworth MH, Neish EM, Miller NS et al (2017) Laboratory testing of donors and stool samples for fecal microbiota transplantation for recurrent Clostridium difficile infection. J Clin Microbiol 55:1002–10
Ianiro G, Porcari S, Bibbò S et al (2021) Donor program for fecal microbiota transplantation: a 3-year experience of a large-volume Italian stool bank. Dig Liver Dis 53:1428–32
Clinical and Laboratory Standards Institute (2021) M100-S31. Performance standards for antimicrobial susceptibility testing: 31th informational supplement. CLSI, Wayne, PA
Ma L, Lu PL, Siu LK et al (2013) Molecular typing and resistance mechanisms of imipenem-non-susceptible Klebsiella pneumoniae in Taiwan: results from the Taiwan surveillance of antibiotic resistance (TSAR) study, 2002–2009. J Med Microbiol 62:101–7
Chen PA, Hung CH, Huang PC et al (2016) Characteristics of CTX-M extended-spectrum β-lactamase-producing Escherichia coli strains isolated from multiple rivers in southern Taiwan. Appl Environ Microbiol 82:1889–97
Diancourt L, Passet V, Verhoef J et al (2005) Multilocus sequence typing of Klebsiella pneumoniae nosocomial isolates. J Clin Microbiol 43:4178–82
Svenungsson B, Lagergren A, Ekwall E et al (2000) Enteropathogens in adult patients with diarrhea and healthy control subjects: a 1-year prospective study in a Swedish clinic for infectious diseases. Clin Infect Dis 30:770–8
Craven LJ, Nair Parvathy S, Tat-Ko J et al (2017) Extended screening costs associated with selecting donors for fecal microbiota transplantation for treatment of metabolic syndrome-associated diseases. Open Forum Infect Dis 4:ofx243
Kassam Z, Dubois N, Ramakrishna B et al (2019) Donor screening for fecal microbiota transplantation. N Engl J Med 381:2070–2
Terveer EM, Vendrik KE, Ooijevaar RE et al (2020) Faecal microbiota transplantation for Clostridioides difficile infection: four years’ experience of the Netherlands Donor Feces Bank. United Eur Gastroenterol J 8:1236–1247
van Nood E, Vrieze A, Nieuwdorp M et al (2013) Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med 368:407–15
Paramsothy S, Borody TJ, Lin E et al (2015) Donor recruitment for fecal microbiota transplantation. Inflamm Bowel Dis 21:1600–6
Costello SP, Tucker EC, La Brooy J et al (2016) Establishing a fecal microbiota transplant service for the treatment of Clostridium difficile infection. Clin Infect Dis 62:908–14
Terveer EM, van Beurden YH, Goorhuis A et al (2017) How to: establish and run a stool bank. Clin Microbiol Infect 23:924–30
Zhang S, Chen Q, Kelly CR et al (2022) Donor screening for fecal microbiota transplantation in China: evaluation of 8483 candidates. Gastroenterology 162:966-968.e3
Yau YK, Mak WYJ, Lui NSR et al (2021) High prevalence of extended-spectrum beta-lactamase organisms and the COVID-19 pandemic impact on donor recruitment for fecal microbiota transplantation in Hong Kong. United Eur Gastroenterol J 9:1027–38
Seo HS, Chin HS, Kim YH et al (2021) Laboratory aspects of donor screening for fecal microbiota transplantation at a Korean fecal microbiota bank. Ann Lab Med 41:424–8
Vendrik KEW, Terveer EM, Kuijper EJ et al (2021) Periodic screening of donor faeces with a quarantine period to prevent transmission of multidrug-resistant organisms during faecal microbiota transplantation: a retrospective cohort study. Lancet Infect Dis 21:711–21
Bezabih YM, Bezabih A, Dion M et al (2022) Comparison of the global prevalence and trend of human intestinal carriage of ESBL-producing Escherichia coli between healthcare and community settings: a systematic review and meta-analysis. JAC Antimicrob Resist 4:dlac048
Huang YS, Lai LC, Chen YA et al (2020) Colonization with multidrug-resistant organisms among healthy adults in the community setting: prevalence, risk factors, and composition of gut microbiome. Front Microbiol 11:1402
Chung HC, Lai CH, Lin JN et al (2012) Bacteremia caused by extended-spectrum-β-lactamase-producing Escherichia coli sequence type ST131 and non-ST131 clones: comparison of demographic data, clinical features, and mortality. Antimicrob Agents Chemother 56:618–22
Tsai WL, Hung CH, Chen HA et al (2018) Extended-spectrum β-lactamase-producing Escherichia coli bacteremia: comparison of pediatric and adult populations. J Microbiol Immunol Infect 51:723–31
US Food and Drug Administration. Information pertaining to additional safety protections regarding use of fecal microbiota for transplantation – screening and testing of stool donors for multi-drug resistant organisms. June 18, 2019. https://www.fda.gov/vaccines-blood-biologics/safety-availability-biologics/information-pertaining-additional-safety-protections-regarding-use-fecal-microbiota-transplantation. Accessed 7 December 2022
Decker BK, Lau AF, Dekker JP et al (2018) Healthcare personnel intestinal colonization with multidrug-resistant organisms. Clin Microbiol Infect 24:82.e1-82.e4
Campos-Madueno EI, Moradi M, Eddoubaji Y et al (2023) Intestinal colonization with multidrug-resistant Enterobacterales: screening, epidemiology, clinical impact, and strategies to decolonize carriers. Eur J Clin Microbiol Infect Dis 42(3):229–254
Funding
This study was supported by grants from the Taipei Veterans General Hospital [V107E-007-1 (108), V108E-007-1 (108), V108E-007-1 (109), V110E-002-1].
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
The study was approved by the Institution Review Board of Taipei Veterans General Hospital. All subjects that participated in this study gave a written informed consent.
Conflict of interest
The authors declare no competing interests.
Disclaimer
The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Additional information
The preliminary data of this study were presented at the annual meeting of the Infectious Diseases Society of Taiwan in March 2022.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chuang, C., Lee, KC., Wang, YP. et al. High carriage rate of extended‐spectrum β‐lactamase Enterobacterales and diarrheagenic Escherichia coli in healthy donor screening for fecal microbiota transplantation. Eur J Clin Microbiol Infect Dis 42, 1103–1113 (2023). https://doi.org/10.1007/s10096-023-04644-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-023-04644-3