Abstract
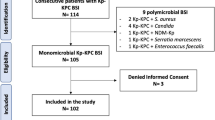
This study was aimed at investigating risk factors for mortality in patients suffering from KPC-producing Klebsiella pneumoniae (KPC-Kp) bloodstream infections (BSIs), evaluating the impact of rapid diagnostics and ceftazidime/avibactam use. This observational retrospective study (January 2017–May 2021) included all patients with a KPC-Kp BSI. Uni-multivariable analyses were carried out to evaluate the effect of clinical variables on both in-hospital death (IHD) and 30-day all-cause mortality, and the role of the combination of ceftazidime/avibactam plus polymyxin. One hundred and ninety-six patients met the study’s inclusion criteria. Older age, having undergone renal replacement therapy during the 30 days preceding the KPC-Kp BSI onset, having an INCREMENT-CPE score ≥ 8, and having suffered from a superimposed and/or following KPC-Kp BSI treatment candidemia were found to be the main factors associated with both mortality rates. Among protective factors, the centrality of ceftazidime/avibactam in monotherapy (IHD: OR: 0.34; CI 95%: 0.11–1.00—30-day all-cause mortality: OR: 0.18; CI 95%: 0.04–0.77) or combination (IHD: OR: 0.51; CI 95%: 0.22–1.19—30-day all-cause mortality: OR: 0.62; CI 95%: 0.21–1.84) emerged and became even more evident once the effect of ceftazidime/avibactam plus polymyxin was removed. Rapid diagnostics may be useful to adopt more effective strategies for the treatment of KPC-Kp BSI patients and implement infection control measures, even if not associated with higher patient survival. Ceftazidime/avibactam, even when used alone, represents an important option against KPC-Kp, while combined use with polymyxin might not have altered its efficacy. Patient comorbidities, severity of BSI, and complications such as candidemia were confirmed to have a significant burden on survival.
Similar content being viewed by others
Data availability
The authors confirm that the data supporting the findings of this study are available within the article.
References
Albiger B, Glasner C, Struelens MJ, Grundmann H, Monnet DL, European survey of carbapenemase-producing enterobacteriaceae (EuSCAPE) working group (2015) Carbapenemase-producing Enterobacteriaceae in Europe: assessment by national experts from 38 countries, May 2015. Euro Surveill 20 pii=30062
Munoz-Price LS, Poirel L, Bonomo RA, Schwaber MJ, Daikos GL, Cormican M et al (2013) Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect Dis 13:785–796
Tzouvelekis LS, Markogiannakis A, Piperaki E, Souli M, Daikos GL (2014) Treating infections caused by carbapenemase-producing enterobacteriaceae. Clin Microbiol Infect 20:862–872
Iacchini S, Sabbatucci M, Gagliotti C, Rossolini GM, Moro ML, Iannazzo S et al (2019) Bloodstream infections due to carbapenemase-producing enterobacteriaceae in Italy: results from nationwide surveillance, 2014 to 2017. Euro Surveill 24:1800159. https://doi.org/10.2807/1560-7917.ES.2019.24.5.1800159
Boattini M, Bianco G, Iannaccone M, Ghibaudo D, Almeida A, Cavallo R et al (2021) Fast-track identification of CTX-M-extended-spectrum-β-lactamase- and carbapenemase-producing Enterobacterales in bloodstream infections: implications on the likelihood of deduction of antibiotic susceptibility in emergency and internal medicine departments. Eur J Clin Microbiol Infect Dis 40:1495–1501. https://doi.org/10.1007/s10096-021-04192-8
Fiori B, D'Inzeo T, Posteraro B, Menchinelli G, Liotti FM, De Angelis G et al (2019) Direct use of eazyplex® SuperBug CRE assay from positive blood cultures in conjunction with inpatient infectious disease consulting for timely appropriate antimicrobial therapy in Escherichia coli and Klebsiella pneumoniae bloodstream infections. Infect Drug Resist 12:1055–1062. https://doi.org/10.2147/IDR.S206323
Bianco G, Boattini M, Iannaccone M, Pastrone L, Bondi A, Peradotto M et al (2021) Integrating rapid diagnostics in Gram-negative bloodstream infections of patients colonized by carbapenemase-producing Enterobacterales. J Hosp Infect 110:84–88. https://doi.org/10.1016/j.jhin.2021.01.015
Giacobbe DR, Giani T, Bassetti M, Marchese A, Viscoli C, Rossolini GM (2019) Rapid microbiological tests for bloodstream infections due to multidrug resistant Gram-negative bacteria: therapeutic implications. Clin Microbiol Infect S1198e743X:30524e5
Shields RK, Nguyen MH, Chen L et al (2017) Ceftazidime-avibactam is superior to other treatment regimens against carbapenem-resistant Klebsiella pneumoniae bacteremia. Antimicrob Agents Chemother 61:e00883-17
van Duin D, Lok JJ, Earley M, Cober E, Richter SS, Perez F et al (2018) Colistin versus ceftazidime-avibactam in the treatment of infections due to carbapenem-resistant enterobacteriaceae. Clin Infect Dis 66:163–171. https://doi.org/10.1093/cid/cix783
Tumbarello M, Trecarichi EM, Corona A et al (2019) Efficacy of ceftazidime-avibactam salvage therapy in patients with infections caused by Klebsiella pneumoniae carbapenemase-producing K. pneumoniae. Clin Infect Dis 68:355–364
Karaiskos I, Daikos GL, Gkoufa A, Adamis G, Stefos A, Symbardi S et al (2021) Ceftazidime/avibactam in the era of carbapenemase-producing Klebsiella pneumoniae: experience from a national registry study. J Antimicrob Chemother 76:775–783. https://doi.org/10.1093/jac/dkaa503
Castón JJ, Cano A, Pérez-Camacho I, Aguado JM, Carratalá J, Ramasco F et al (2022) Impact of ceftazidime/avibactam versus best available therapy on mortality from infections caused by carbapenemase-producing enterobacterales (CAVICOR study). J Antimicrob Chemother 77:1452–1460. https://doi.org/10.1093/jac/dkac049
Fiore M, Alfieri A, Di Franco S, Pace MC, Simeon V, Ingoglia G et al (2020) Ceftazidime-avibactam combination therapy compared to ceftazidime-avibactam monotherapy for the treatment of severe infections due to carbapenem-resistant pathogens: a systematic review and network meta-analysis. Antibiotics 9:388. https://doi.org/10.3390/antibiotics9070388
Meini S, Viaggi B, Tascini C (2021) Mono vs. combo regimens with novel beta-lactam/beta-lactamase inhibitor combinations for the treatment of infections due to carbapenemase-producing enterobacterales: insights from the literature. Infection 49:411–421. https://doi.org/10.1007/s15010-021-01577-x
Tumbarello M, Raffaelli F, Giannella M, Mantengoli E, Mularoni A, Venditti M et al (2021) ceftazidime-avibactam use for Klebsiella pneumoniae Carbapenemase-producing K. pneumoniae infections: a retrospective observational multicenter study. Clin Infect Dis 73:1664–1676. https://doi.org/10.1093/cid/ciab176
Shields RK, Nguyen MH, Hao B, Kline EG, Clancy CJ (2018) Colistin does not potentiate ceftazidime-avibactam killing of carbapenem-resistant enterobacteriaceae in vitro or suppress emergence of ceftazidime-avibactam resistance. Antimicrob Agents Chemother 62:e01018–e01018. https://doi.org/10.1128/AAC.01018-18
Borjan J, Meyer KA, Shields RK, Wenzler E (2020) Activity of ceftazidime-avibactam alone and in combination with polymyxin B against carbapenem-resistant Klebsiella pneumoniae in a tandem in vitro time-kill/in vivo Galleria mellonella survival model analysis. Int J Antimicrob Agents 55:105852. https://doi.org/10.1016/j.ijantimicag.2019.11.009
CDC/NHSN Surveillance definitions for specific types of infections. Available at: https://www.cdc.gov/nhsn/PDFs/pscManual/17pscNosInfDef_current.pdf. Accessed 22 February 2022.
https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_12.0_Breakpoint_Tables.pdf. Accessed 10 February 2022.
Bianco G, Boattini M, van Asten SAV, Iannaccone M, Zanotto E, Zaccaria T et al (2020) RESIST-5 O.O.K.N.V. and NG-Test Carba 5 assays for the rapid detection of carbapenemase-producing enterobacterales from positive blood cultures: a comparative study. J Hosp Infect 105:162–166. https://doi.org/10.1016/j.jhin.2020.03.022
Satlin MJ, Chen L, Gomez-Simmonds A, Marino J, Weston G, Bhowmick T et al (2022) Impact of a rapid molecular test for Klebsiella pneumoniae carbapenemase and ceftazidime-avibactam use on outcomes after bacteremia caused by carbapenem-resistant Enterobacterales. Clin Infect Dis 75:ciac354. https://doi.org/10.1093/cid/ciac354
Campos AF, Arantes T, Cambiais AMVB, Cury AP, Tiroli CG, Rossi F et al (2022) Impact of an antimicrobial stewardship program intervention associated with the rapid identification of microorganisms by MALDI-TOF and detection of resistance genes in ICU patients with Gram-negative bacteremia. Antibiotics 11:1226. https://doi.org/10.3390/antibiotics11091226
Bianco G, Boattini M, Comini S, Iannaccone M, Bondi A, Cavallo R et al (2022) In vitro activity of cefiderocol against ceftazidime-avibactam susceptible and resistant KPC-producing enterobacterales: cross-resistance and synergistic effects. Eur J Clin Microbiol Infect Dis 41:63–70. https://doi.org/10.1007/s10096-021-04341-z
Poirel L, Sadek M, Kusaksizoglu A, Nordmann P (2022) Co-resistance to ceftazidime-avibactam and cefiderocol in clinical isolates producing KPC variants. Eur J Clin Microbiol Infect Dis 41:677–680. https://doi.org/10.1007/s10096-021-04397-x
Bianco G, Boattini M, Bondi A, Comini S, Zaccaria T, Cavallo R et al (2022) Outbreak of ceftazidime-avibactam resistant Klebsiella pneumoniae carbapenemase (KPC)-producing Klebsiella pneumoniae in a COVID-19 intensive care unit, Italy: urgent need for updated diagnostic protocols of surveillance cultures. J Hosp Infect 122:217–219. https://doi.org/10.1016/j.jhin.2022.02.001
Gaibani P, Lombardo D, Foschi C, Re MC, Ambretti S (2020) Evaluation of five carbapenemase detection assays for enterobacteriaceae harbouring blaKPC variants associated with ceftazidime/avibactam resistance. J Antimicrob Chemother 75:2010–2013. https://doi.org/10.1093/jac/dkaa079
Bianco G, Boattini M, Iannaccone M, Bondi A, Ghibaudo D, Zanotto E et al (2021) Carbapenemase detection testing in the era of ceftazidime/avibactam-resistant KPC-producing Enterobacterales: a 2-year experience. J Glob Antimicrob Resist 24:411–414. https://doi.org/10.1016/j.jgar.2021.02.008
Hernández-García M, Castillo-Polo JA, Cordero DG, Pérez-Viso B, García-Castillo M, Saez de la Fuente J, Morosini MI et al (2022) Impact of ceftazidime-avibactam treatment in the emergence of novel KPC variants in the ST307-Klebsiella pneumoniae high-risk clone and consequences for their routine detection. J Clin Microbiol 60:e0224521. https://doi.org/10.1128/jcm.02245-21
Falcone M, Bassetti M, Tiseo G, Giordano C, Nencini E, Russo A et al (2020) Time to appropriate antibiotic therapy is a predictor of outcome in patients with bloodstream infection caused by KPC-producing Klebsiella pneumoniae. Crit Care 24:29. https://doi.org/10.1186/s13054-020-2742-9
Gutiérrez-Gutiérrez B, Salamanca E, de Cueto M, Hsueh PR, Viale P, Paño-Pardo JR et al (2017) REIPI/ESGBIS/INCREMENT Investigators. Effect of appropriate combination therapy on mortality of patients with bloodstream infections due to carbapenemase-producing Enterobacteriaceae (INCREMENT): a retrospective cohort study. Lancet Infect Dis 17:726–734
Bassetti M, Giacobbe DR, Vena A, Wolff M (2019) Diagnosis and treatment of candidemia in the intensive care unit. Semin Respir Crit Care Med 40:524–539. https://doi.org/10.1055/s-0039-1693704
Author information
Authors and Affiliations
Contributions
Boattini M, Bianco G, Almeida A, De Rosa FG, Costa C, and Cavallo R designed the study; Boattini M, Bianco G, Comini S, and Iannaccone M acquired data; Boattini M, Bianco G, and Charrier L analyzed and interpreted data; Boattini M wrote the paper; all authors revised the article critically and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki. Formal ethical approval was obtained by our Center’s institutional review board (Protocol No. 0029345).
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Boattini, M., Bianco, G., Charrier, L. et al. Rapid diagnostics and ceftazidime/avibactam for KPC-producing Klebsiella pneumoniae bloodstream infections: impact on mortality and role of combination therapy. Eur J Clin Microbiol Infect Dis 42, 431–439 (2023). https://doi.org/10.1007/s10096-023-04577-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-023-04577-x