Abstract
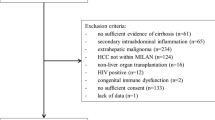
It is unclear whether norfloxacin predisposes to infections by multidrug-resistant organisms (MDROs). We aimed to evaluate if patients with cirrhosis receiving norfloxacin prophylaxis at the time of the diagnosis of bacterial infections were more likely to present a multidrug-resistant isolate than those without prophylaxis. This is a cross-sectional study of hospitalized patients with cirrhosis and bacterial infections from Argentina and Uruguay (NCT03919032) from September 2018 to December 2020. The outcome variable was a multidrug-resistant bacterial infection. We used inverse probability of treatment weighting to estimate the odds ratio (OR) of norfloxacin on infection caused by MDROs considering potential confounders. Among the 472 patients from 28 centers, 53 (11%) were receiving norfloxacin at the time of the bacterial infection. Patients receiving norfloxacin had higher MELD-sodium, were more likely to have ascites or encephalopathy, to receive rifaximin, beta-blockers, and proton-pump inhibitors, to have a nosocomial or health-care-associated infection, prior bacterial infections, admissions to critical care units or invasive procedures, and to be admitted in a liver transplant center. In addition, we found that 13 (24.5%) patients with norfloxacin and 90 (21.5%) of those not receiving it presented infections caused by MDROs (adjusted OR 1.55; 95% CI: 0.60–4.03; p = 0.360). The use of norfloxacin prophylaxis at the time of the diagnosis of bacterial infections was not associated with multidrug resistance. These results help empiric antibiotic selection and reassure the current indication of norfloxacin prophylaxis in well-selected patients.
Study registration number: NCT03919032


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
Abbreviations
- MDRO:
-
Multidrug-resistant organisms
- SBP:
-
Spontaneous bacterial peritonitis
- ESBLs:
-
Extended-spectrum B-lactamase
- MRSA:
-
Methicillin-resistant Staphylococcus aureus
- CNSA:
-
Coagulase-negative Staphylococcus
- VRE:
-
Vancomycin-resistant Enterococci
- CPE:
-
Carbapenemase-producing Enterobacteriaceae
- MDR:
-
Multidrug resistant
- INR:
-
International normalized ratio
- OR:
-
Odds ratio
- ATE:
-
Average treatment effect
- IPTW:
-
Inverse probability of treatment weights
- MAR:
-
Missing at random
- HCA:
-
Health-care-associated
- IQR:
-
Interquartile range
References
World Health Organization (2020, July 31). Antibiotic resistance. https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance
Medina E, Pieper DH (2016) Tackling threats and future problems of multidrug-resistant bacteria. Curr Top Microbiol Immunol 398:3–33
Jalan R, Fernandez J, Wiest R, Schnabl B, Moreau R, Angeli P et al (2014) Bacterial infections in cirrhosis: a position statement based on the EASL Special Conference 2013. J Hepatol 60:1310–1324
Fernández J, Prado V, Trebicka J, Amoros A, Gustot T, Wiest R et al (2019) Multidrug-resistant bacterial infections in patients with decompensated cirrhosis and with acute-on-chronic liver failure in Europe [Internet]. J Hepatol 70:398–411. https://doi.org/10.1016/j.jhep.2018.10.02710.1016/j.jhep.2018.10.027
Piano S, Singh V, Caraceni P, Maiwall R, Alessandria C, Fernandez J et al (2019) Epidemiology and effects of bacterial infections in patients with cirrhosis worldwide. Gastroenterology 156:1368–80.e10
Merli M, Lucidi C, Di Gregorio V, Falcone M, Giannelli V, Lattanzi B et al (2015) The spread of multi drug resistant infections is leading to an increase in the empirical antibiotic treatment failure in cirrhosis: a prospective survey [Internet]. Plos One 10:e0127448. https://doi.org/10.1371/journal.pone.0127448
Fernández J, Acevedo J, Castro M, Garcia O, de Lope CR, Roca D et al (2012) Prevalence and risk factors of infections by multiresistant bacteria in cirrhosis: a prospective study. Hepatology 55:1551–1561
Moreau R, Elkrief L, Bureau C, Perarnau J-M, Thévenot T, Saliba F et al (2018) Effects of long-term norfloxacin therapy in patients with advanced cirrhosis. Gastroenterology 155:1816–27.e9
Magiorakos A-P, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG et al (2012) Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 18:268–281
Arroyo V, Moreau R, Kamath PS, Jalan R, Ginès P, Nevens F et al (2016) Acute-on-chronic liver failure in cirrhosis. Nat Rev Dis Primers 9(2):1–18
Friedman ND, Deborah FN (2002) health care–associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections [Internet]. Ann Intern Med 137:791. https://doi.org/10.7326/0003-4819-137-10-200211190-00007
Lee KJ, Tilling KM, Cornish RP, Little RJA, Bell ML, Goetghebeur E et al (2021) Framework for the treatment and reporting of missing data in observational studies: the treatment and reporting of missing data in observational studies framework. J Clin Epidemiol 134:79–88
Austin PC, Stuart EA (2015) Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies [Internet]. Stat Med 34:3661–3679. https://doi.org/10.1002/sim.660710.1002/sim.6607
Bajaj JS, Tandon P, O’Leary JG, Wong F, Biggins SW, Garcia-Tsao G et al (2019) Outcomes in patients with cirrhosis on primary compared to secondary prophylaxis for spontaneous bacterial peritonitis. Am J Gastroenterol 114:599–606
Kulkarni AV, Premkumar M, Arab JP, Kumar K, Sharma M, Reddy ND et al (2022) Early diagnosis and prevention of infections in cirrhosis. Semin Liver Dis 42:293–312
European Association for the Study of the Liver (2010) EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol 53:397–417
Bush NG, Diez-Santos I, Abbott LR, Maxwell A (2020) Quinolones: mechanism, lethality and their contributions to antibiotic resistance. Molecules [Internet] 1:25. https://doi.org/10.3390/molecules25235662
Ginés P, Rimola A, Planas R, Vargas V, Marco F, Almela M et al (1990) Norfloxacin prevents spontaneous bacterial peritonitis recurrence in cirrhosis: results of a double-blind, placebo-controlled trial. Hepatology 12:716–724
Grangé JD, Roulot D, Pelletier G, Pariente EA, Denis J, Ink O et al (1998) Norfloxacin primary prophylaxis of bacterial infections in cirrhotic patients with ascites: a double-blind randomized trial. J Hepatol 29:430–436
Soriano G, Guarner C, Teixidó M, Such J, Barrios J, Enríquez J et al (1991) Selective intestinal decontamination prevents spontaneous bacterial peritonitis [Internet]. Gastroenterology 100:477–481. https://doi.org/10.1016/0016-5085(91)90219-b
Fernández J, Navasa M, Planas R, Montoliu S, Monfort D, Soriano G et al (2007) Primary prophylaxis of spontaneous bacterial peritonitis delays hepatorenal syndrome and improves survival in cirrhosis. Gastroenterology 133:818–824
Kulkarni AV, Tirumalle S, Premkumar M, Kumar K, Fatima S, Rapole B et al (2022) Primary norfloxacin prophylaxis for APASL-defined acute-on-chronic liver failure: a placebo-controlled double-blind randomized trial. Am J Gastroenterol 1(117):607–616
Acknowledgements
We would like to acknowledge the Argentinean Association for the Study of the Liver, which facilitated this project. In addition, we thank the patients and families who voluntarily agreed to participate in this project.
Author information
Authors and Affiliations
Contributions
Sebastián, Marciano, MD, MsC; Maria, N, Gutierrez-Acevedo, Astrid, Smud, MD; Adrian, C, Gadano, MD, PhD; and Diego, H, Giunta, MD, PhD, contributed to the study conception and design, material preparation, and data collection.
Sebastián, Marciano, MD, and Giunta, MD, PhD, performed the analyses and the first draft of the manuscript.
All authors read and approved the final manuscript and performed data collection.
Corresponding author
Ethics declarations
Ethics approval
Participating centers obtained approval from the corresponding Institutional review board.
Consent to participate
Informed consent was obtained from all patients.
Consent for publication
All authors read and approved the final manuscript and performed data collection.
Competing interests
Sebastián, Marciano, MD, MsC; Maria, N, Gutierrez-Acevedo, MD; Sabrina, Barbero, MD; Lorena, Notari, MD; Marina, Agozino, MD; Jose, L, Fernandez, MD; Maria M, Anders, MD; Nadia, Grigera, MD; Florencia, Antinucci, MD; Orlando, F, Orozco Ganem, MD; Maria, D, Murga, MD; Daniela, Perez, MD; Ana, Palazzo, MD; Liria, Martinez Rejtman, MD; Ivonne, G, Duarte, MD; Julio, Vorobioff, MD; Victoria, Trevizan, MD; Sofía, Bulaty, MD; Fernando, Bessone, MD; Marcelo, Valverde, MD; Martín, Elizondo, MD; José, D, Bosia, MD; Silvia, M, Borzi, MD; Teodoro, E, Stieben, MD; Adriano, Masola, MD; Sebastian, E, Ferretti, MD; Diego, Arufe, MD; Ezequiel, Demirdjian, MD; Maria, P, Raffa, MD; Mirta, Peralta, MD; Hugo, A, Fainboim, MD; Cintia, E, Vazquez, MD; Pablo, Ruiz, MD; José, E, Martínez, MD; Leandro, A, Heffner, MD; Andrea, Odzak, MD; Melisa, Dirchwolf, MD; Astrid, Smud, MD; Manuel, Mendizabal, MD; Carla, Bellizzi, MD; Ana, Martinez, MD; Jesica, Tomatis, MD; Andres, Bruno, MD; Agñel, Ramos, MD; Josefina, Pages, MD; Silvina, Tevez, MD; Adrian, C, Gadano, MD, PhD; and Diego, H, Giunta MD, PhD, have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marciano, S., Gutierrez-Acevedo, M.N., Barbero, S. et al. Norfloxacin prophylaxis effect on multidrug resistance in patients with cirrhosis and bacterial infections. Eur J Clin Microbiol Infect Dis 42, 481–491 (2023). https://doi.org/10.1007/s10096-023-04572-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-023-04572-2