Abstract
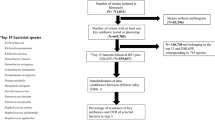
The increasing resistance of gram-negative bacteria is a serious global public health concern. One way to prevent increasing antibiotic resistance is by implementing the antibiotic stewardship program. This study aimed to assess the changes in the consumption of antimicrobials and antimicrobial resistance rates after implementing piperacillin/tazobactam restriction. This study was conducted at Kandong Sacred Heart Hospital. We retrospectively collected and analysed data between October 2018 and May 2021 to evaluate antibiotic consumption and resistance patterns after restricting piperacillin/tazobactam. This study included two periods, a 16-month pre-restriction period and a 16-month post-restriction period. During the study period, there was a significant decrease in the consumption of piperacillin/tazobactam after implementing the restriction policy (127.82 ± 9.39 to 104.82 ± 15.66 defined daily doses/1000 patient days, p < 0.001). A significant decrease in the resistance rate of Acinetobacter spp. was observed for cefepime (p = 0.001), ceftazidime (p = 0.004), levofloxacin (p = 0.021), meropenem (p = 0.002) and piperacillin (p = 0.028). The introduction of piperacillin/tazobactam restriction reduced their use and positively impacted the resistance rates of Acinetobacter spp., carbapenem-resistant Pseudomonas spp. and carbapenem-resistant Enterobacteriaceae which are major threats to nosocomial infections.


Similar content being viewed by others
Data availability
The datasets generated and/or during analysed during the current study are available from the corresponding author on reasonable request.
References
Kaye KS, Pogue JM (2015) Infections caused by resistant gram-negative bacteria: epidemiology and management. Pharmacotherapy 35(10):949–962
Nathwani D, Raman G, Sulham K, Gavaghan M, Menon V (2014) Clinical and economic consequences of hospital-acquired resistant and multidrug-resistant Pseudomonas aeruginosa infections: a systematic review and meta-analysis. Antimicrob Resist Infect Control 3(1):32
Lemos EV, de la Hoz FP, Einarson TR, McGhan WF, Quevedo E, Castaneda C, Kawai K (2014) Carbapenem resistance and mortality in patients with Acinetobacter baumannii infection: systematic review and meta-analysis. Clin Microbiol Infect 20(5):416–423
Peleg AY, Hooper DC (2010) Hospital-acquired infections due to gram-negative bacteria. N Engl J Med 362(19):1804–1813
Rodriguez-Rojas A, Rodriguez-Beltran J, Couce A, Blazquez J (2013) Antibiotics and antibiotic resistance: a bitter fight against evolution. Int J Med Microbiol 303(6–7):293–297
Fishman N (2006) Antimicrobial stewardship. Am J Infect Control 34 (5 Suppl 1):S55–63; discussion S64–73
Dyar OJ, Huttner B, Schouten J, Pulcini C, Esgap, (2017) What is antimicrobial stewardship? Clin Microbiol Infect 23(11):793–798
Barlam TF, Cosgrove SE, Abbo LM, MacDougall C, Schuetz AN, Septimus EJ, Srinivasan A, Dellit TH, Falck-Ytter YT, Fishman NO, Hamilton CW, Jenkins TC, Lipsett PA, Malani PN, May LS, Moran GJ, Neuhauser MM, Newland JG, Ohl CA, Samore MH, Seo SK, Trivedi KK (2016) Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis 62(10):e51-77
Saez-Llorens X, Castrejon de Wong MM, Castano E, De Suman O, De Moros D, De Atencio I (2000) Impact of an antibiotic restriction policy on hospital expenditures and bacterial susceptibilities: a lesson from a pediatric institution in a developing country. Pediatr Infect Dis J 19(3):200–206
Brahmi N, Blel Y, Kouraichi N, Lahdhiri S, Thabet H, Hedhili A, Amamou M (2006) Impact of ceftazidime restriction on gram-negative bacterial resistance in an intensive care unit. J Infect Chemother 12(4):190–194
Abdallah M, Badawi M, Amirah MF, Rasheed A, Mady AF, Alodat M, Alharthy A (2017) Impact of carbapenem restriction on the antimicrobial susceptibility pattern of Pseudomonas aeruginosa isolates in the ICU. J Antimicrob Chemother 72(11):3187–3190
Yusef D, Hayajneh WA, Bani Issa A, Haddad R, Al-Azzam S, Lattyak EA, Lattyak WJ, Gould I, Conway BR, Bond S, Conlon-Bingham G, Aldeyab MA (2021) Impact of an antimicrobial stewardship programme on reducing broad-spectrum antibiotic use and its effect on carbapenem-resistant Acinetobacter baumannii (CRAb) in hospitals in Jordan. J Antimicrob Chemother 76(2):516–523
Regal RE, DePestel DD, VandenBussche HL (2003) The effect of an antimicrobial restriction program on Pseudomonas aeruginosa resistance to beta-lactams in a large teaching hospital. Pharmacotherapy 23(5):618–624
Murki S, Jonnala S, Mohammed F, Reddy A (2010) Restriction of cephalosporins and control of extended spectrum beta-lactamase producing gram negative bacteria in a neonatal intensive care unit. Indian Pediatr 47(9):785–788
Agodi A, Auxilia F, Barchitta M, Brusaferro S, D’Errico MM, Montagna MT, Pasquarella C, Tardivo S, Mura I, Spin-Uti network of the Gisioworking Group of the Italian Society of Hygiene, PM Public H (2015) Antibiotic consumption and resistance: results of the SPIN-UTI project of the GISIO-SItI. Epidemiol Prev 39(4 Suppl 1):94–98
White AC Jr, Atmar RL, Wilson J, Cate TR, Stager CE, Greenberg SB (1997) Effects of requiring prior authorization for selected antimicrobials: expenditures, susceptibilities, and clinical outcomes. Clin Infect Dis 25(2):230–239
Amaha ND, Weldemariam DG, Berhe YH (2020) Antibiotic consumption study in two hospitals in Asmara from 2014 to 2018 using WHO’s defined daily dose (DDD) methodology. PLoS ONE 15(7):e0233275
Razazi K, Derde LPG, Verachten M, Legrand P, Lesprit P, Brun-Buisson C (2012) Clinical impact and risk factors for colonization with extended-spectrum β-lactamase-producing bacteria in the intensive care unit. Intensive Care Med 38:1769–1778
Le Terrier C, Vinetti M, Bonjean P et al (2021) Impact of a restrictive antibiotic policy on the acquisition of extended-spectrum beta-lactamase-producing Enterobacteriaceae in an endemic region: a before-and-after, propensity-matched cohort study in a Caribbean intensive care unit. Crit Care. 25(1):261. Published 2021 Jul 26. https://doi.org/10.1186/s13054-021-03660-z
Vardakas KZ, Tansarli GS, Bliziotis IA, Falagas ME (2013) β-Lactam plus aminoglycoside or fluoroquinolone combination versus β-lactam monotherapy for Pseudomonas aeruginosa infections: a meta-analysis. Int J Antimicrob Agents 41(4):301–310
Yoon YK, Kim J, Moon C, Lee MS, Hur J, Lee H, Kim SW (2019) Antimicrobial susceptibility of microorganisms isolated from patients with intraabdominal infection in Korea: a multicenter study. J Korean Med Sci 34(47):e309
Choe YJ, Shin JY (2019) Trends in the use of antibiotics among Korean children. Korean J Pediatr 62(4):113–118
Kim B, Lee MJ, Moon SM, Park SY, Song KH, Lee H, Park JS, Lee MS, Choi SM, Yeom JS, Kim JY, Kim CJ, Chang HH, Kim ES, Kim TH, Kim HB (2020) Current status of antimicrobial stewardship programmes in Korean hospitals: results of a 2018 nationwide survey. J Hosp Infect 104(2):172–180
Burke JP (1998) Antibiotic resistance–squeezing the balloon? JAMA 280(14):1270–1271
Jean SS, Harnod D, Hsueh PR (2022) Global threat of carbapenem-resistant gram-negative bacteria. Front Cell Infect Microbiol 12:823684
Gales AC, Seifert H, Gur D, Castanheira M, Jones RN, Sader HS (2019) Antimicrobial susceptibility of Acinetobacter calcoaceticus-Acinetobacter baumannii complex and Stenotrophomonas maltophilia clinical isolates: results from the SENTRY Antimicrobial Surveillance Program (1997–2016). Open Forum Infect Dis 6(Suppl 1):S34–S46
Kritsotakis EI, Tsioutis C, Roumbelaki M, Christidou A, Gikas A (2011) Antibiotic use and the risk of carbapenem-resistant extended-spectrum-{beta}-lactamase-producing Klebsiella pneumoniae infection in hospitalized patients: results of a double case-control study. J Antimicrob Chemother 66(6):1383–1391
Kim YA, Lee SJ, Park YS, Lee YJ, Yeon JH, Seo YH, Lee K (2020) Risk factors for carbapenemase- producing Enterobacterales infection or colonization in a Korean intensive care unit: a case-control study. Antibiotics (Basel) 9(10):680
Gasink LB, Edelstein PH, Lautenbach E, Synnestvedt M, Fishman NO (2009) Risk factors and clinical impact of Klebsiella pneumoniae carbapenemase-producing K pneumoniae. Infect Control Hosp Epidemiol 30(12):1180–5
Ahn JY, Song JE, Kim MH, Choi H, Kim JK, Ann HW, Kim JH, Jeon Y, Jeong SJ, Kim SB, Ku NS, Han SH, Song YG, Yong D, Lee K, Kim JM, Choi JY (2014) Risk factors for the acquisition of carbapenem-resistant Escherichia coli at a tertiary care center in South Korea: a matched case-control study. Am J Infect Control 42(6):621–625
Papadimitriou-Olivgeris M, Marangos M, Fligou F, Christofidou M, Bartzavali C, Anastassiou ED, Filos KS (2012) Risk factors for KPC-producing Klebsiella pneumoniae enteric colonization upon ICU admission. J Antimicrob Chemother 67(12):2976–2981
Kang JS, Yi J, Ko MK, Lee SO, Lee JE, Kim KH (2019) Prevalence and risk factors of carbapenem-resistant Enterobacteriaceae acquisition in an emergency intensive care unit in a tertiary hospital in Korea: a Case-Control Study. J Korean Med Sci 34(18):e140
Lee HJ, Choi JK, Cho SY, Kim SH, Park SH, Choi SM, Lee DG, Choi JH, Yoo JH (2016) Carbapenem-resistant Enterobacteriaceae: prevalence and risk factors in a single community-based hospital in Korea. Infect Chemother 48(3):166–173
Korea Disease Control and Prevention Agency (2020) Infectious disease surveillance yearbook. https://www.kdca.go.kr/npt
Centers for Disease Control and Prevention (2013) Antibiotic resistance threats in the United States. https://www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdf
Centers for Disease Control and Prevention (2019) Antibiotic resistnace threats in the United States. https://www.cdc.gov/DrugResistance/Biggest-Threats.html
Kim D, Yoon EJ, Hong JS, Choi MH, Kim HS, Kim YR, Kim YA, Uh Y, Shin KS, Shin JH, Park JS, Park KU, Won EJ, Kim SH, Shin JH, Kim JW, Lee S, Jeong SH (2021) Major bloodstream infection-causing bacterial pathogens and their antimicrobial resistance in South Korea, 2017–2019: Phase I Report From Kor-GLASS. Front Microbiol 12:799084
Liu C, Yoon EJ, Kim D, Shin JH, Shin JH, Shin KS, Kim YA, Uh Y, Kim HS, Kim YR, Jeong SH (2019) Antimicrobial resistance in South Korea: a report from the Korean global antimicrobial resistance surveillance system (Kor-GLASS) for 2017. J Infect Chemother 25(11):845–859
Enne VI, Livermore DM, Stephens P, Hall LM (2001) Persistence of sulphonamide resistance in Escherichia coli in the UK despite national prescribing restriction. Lancet 357(9265):1325–1328
Funding
This work was supported by the Kangdong Sacred Heart Hospital Fund [grant number 2021–03].
Author information
Authors and Affiliations
Contributions
Jihyu Oh: methodology, investigation, and writing. So Yeon Park: supervision, conceptualization, and statistical analysis. Jin Seo Lee: conceptualization and supervision. Seo Hu Lee: investigation.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Institutional Review Board of Kandong Sacred Heart Hospital (study number 2021–03-009).
Consent to participate
Not applicable.
Consent to publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Oh, J., Park, S.Y., Lee, J.S. et al. Effect of restricting piperacillin/tazobactam prescription on rates of antimicrobial resistance in gram-negative bacteria and antibiotic consumption. Eur J Clin Microbiol Infect Dis 42, 53–60 (2023). https://doi.org/10.1007/s10096-022-04525-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-022-04525-1