Abstract
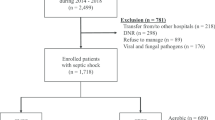
Culture results of patients with septic shock affect their management strategies, including antibiotic administration. This study aimed to compare clinical characteristics and outcomes of patients with culture-negative septic shock (CNSS) and culture-positive septic shock (CPSS) in the emergency department. We also assessed the differences in duration and de-escalation timing of antibiotic administration between the two groups. This single-center, retrospective, case–control study included adult patients diagnosed with septic shock in the emergency department between January 1, 2019 and March 31, 2020. They were divided into the CNSS and CPSS groups based on their culture results. The baseline characteristics, infection sites, culture types, and clinical outcomes were recorded and compared. Patients with CPSS (63.7%, 311/488) and CNSS (36.3%, 177/488) were identified. The CPSS and CNSS groups had comparable clinical outcomes, including mechanical ventilation (29.6% vs. 32.8%, p = 0.46), renal replacement therapy (19.3% vs. 23.2%, p = 0.31), 30-day mortality (35.7% vs. 36.7%, p = 0.82), and in-hospital mortality (39.5% vs. 41.8%, p = 0.63). The CNSS group had a significantly shorter duration (13 [8 − 19] vs. 16 [10 − 23], days, p = 0.04) and earlier de-escalation timing (5 [2 − 9] vs. 9 [7 − 12], day, p = 0.02) of antibiotic administration than the CPSS group. Patients with CNSS and CPSS had similar clinical characteristics and proportion of adverse outcomes. Physicians can evaluate the feasibility of early de-escalation or discontinuation of antibiotic administration in patients with CNSS showing clinical improvement.


Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the present study are available from the corresponding author upon reasonable request.
Abbreviations
- CNSS:
-
Culture-negative septic shock
- CPSS:
-
Culture-positive septic shock
- ED:
-
Emergency department
- MAP:
-
Mean arterial pressure
- qSOFA:
-
Quick sequential organ failure assessment
- SIRS:
-
Systemic inflammatory response syndrome
- SOFA:
-
Sequential organ failure assessment
- ICU:
-
Intensive care unit
- CRP:
-
C-reactive protein
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- INR:
-
International normalized ratio
References
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche J-D, Coopersmith CM (2016) The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315(8):801–810
Mayr FB, Yende S, Angus DC (2014) Epidemiol Severe Sepsis Virulence 5(1):4–11
Vincent J-L, Jones G, David S, Olariu E, Cadwell KK (2019) Frequency and mortality of septic shock in Europe and North America: a systematic review and meta-analysis. Crit Care 23(1):1–11
Kim J-s, Kim Y-J, Kim WY (2021) Characteristics and clinical outcomes of culture-negative and culture-positive septic shock: a single-center retrospective cohort study. Crit Care 25(1):1–9
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, Machado FR, Mcintyre L, Ostermann M, Prescott HC (2021) Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med 47(11):1181–1247
Li Y, Guo J, Yang H, Li H, Shen Y, Zhang D (2021) Comparison of culture-negative and culture-positive sepsis or septic shock: a systematic review and meta-analysis. Crit Care 25(1):1–9
Gupta S, Sakhuja A, Kumar G, McGrath E, Nanchal RS, Kashani KB (2016) Culture-negative severe sepsis: nationwide trends and outcomes. Chest 150(6):1251–1259
Kethireddy S, Bilgili B, Sees A, Kirchner HL, Ofoma UR, Light RB, Mirzanejad Y, Maki D, Kumar A, Layon AJ (2018) Culture-negative septic shock compared with culture-positive septic shock: a retrospective cohort study. Crit Care Med 46(4):506–512
Sigakis MJ, Jewell E, Maile MD, Cinti SK, Bateman BT, Engoren M (2019) Culture negative and culture positive sepsis: a comparison of characteristics and outcomes. Anesth Analg 129(5):1300
Paquette K, Sweet D, Stenstrom R, Stabler SN, Lawandi A, Akhter M, Davidson AC, Gavric M, Jinah R, Saeed Z (2021) Neither blood culture positivity nor time to positivity is associated with mortality among patients presenting with severe manifestations of sepsis: the FABLED cohort study. Open Forum Infect Dis 8(7):ofab321
Gray A, Ward K, Lees F, Dewar C, Dickie S, McGuffie C (2013) The epidemiology of adults with severe sepsis and septic shock in Scottish emergency departments. Emerg Med J 30(5):397–401
Yu C-W, Chang S-S, Lai C-C, Wu J-Y, Yen DW, M-tG L, Yeh C-C, Chung J-Y, Lin Y-J, Lee C-C (2019) Epidemiology of emergency department sepsis: a national cohort study between 2001 and 2012. Shock 51(5):619–624
Armstrong-Briley D, Hozhabri NS, Armstrong K, Puthottile J, Benavides R, Beal S (2015) Comparison of length of stay and outcomes of patients with positive versus negative blood culture results. Proc (Bayl Univ Med Cent) 28(1):10–13
Klompas M, Calandra T, Singer M (2018) Antibiotics for sepsis—finding the equilibrium. JAMA 320(14):1433–1434
Thorndike J, Kollef MH (2020) Culture-negative sepsis. Curr Opin Criti Care 26(5):473–477
Opota O, Croxatto A, Prod’hom G, Greub G (2015) Blood culture-based diagnosis of bacteraemia: state of the art. Clin Microbiol Infect 21(4):313–322
Tabah A, Bassetti M, Kollef MH, Zahar J-R, Paiva J-A, Timsit J-F, Roberts JA, Schouten J, Giamarellou H, Rello J (2020) Antimicrobial de-escalation in critically ill patients: a position statement from a task force of the European Society of Intensive Care Medicine (ESICM) and European Society of Clinical Microbiology and Infectious Diseases (ESCMID) Critically Ill Patients Study Group (ESGCIP). Intensive Care Med 46(2):245–265
Garnacho-Montero J, Escoresca-Ortega A, Fernández-Delgado E (2015) Antibiotic de-escalation in the ICU: how is it best done? Curr Opin Infect Dis 28(2):193–198
Kaukonen K-M, Bailey M, Pilcher D, Cooper DJ, Bellomo R (2015) Systemic inflammatory response syndrome criteria in defining severe sepsis. N Engl J Med 372(17):1629–1638
Ferreira FL, Bota DP, Bross A, Mélot C, Vincent J-L (2001) Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA 286(14):1754–1758
Allison MG, Heil EL, Hayes BD (2017) Appropriate antibiotic therapy. Emerg Med Clin North Am 35(1):25–42
Scheer C, Fuchs C, Gründling M, Vollmer M, Bast J, Bohnert J, Zimmermann K, Hahnenkamp K, Rehberg S, Kuhn S-O (2019) Impact of antibiotic administration on blood culture positivity at the beginning of sepsis: a prospective clinical cohort study. Clin Microbiol Infect 25(3):326–331
Lin G-L, McGinley JP, Drysdale SB, Pollard AJ (2018) Epidemiology and immune pathogenesis of viral sepsis. Front Immunol 9:2147
Phua J, Ngerng WJ, See KC, Tay CK, Kiong T, Lim HF, Chew MY, Yip HS, Tan A, Khalizah HJ (2013) Characteristics and outcomes of culture-negative versus culture-positive severe sepsis. Crit Care 17(5):1–12
Scott MC (2017) Defining and diagnosing sepsis. Emerg Med Clin North Am 35(1):1–9
Ferrer R, Martin-Loeches I, Phillips G, Osborn TM, Townsend S, Dellinger RP, Artigas A, Schorr C, Levy MM (2014) Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: results from a guideline-based performance improvement program. Crit Care Med 42(8):1749–1755
Alam N, Oskam E, Stassen PM, van Exter P, van de Ven PM, Haak HR, Holleman F, van Zanten A, van Leeuwen-Nguyen H, Bon V (2018) Prehospital antibiotics in the ambulance for sepsis: a multicentre, open label, randomised trial. Lancet Respir Med 6(1):40–50
Mignot-Evers L, Raaijmakers V, Buunk G, Brouns S, Romano L, van Herpt T, Gharbharan A, Dieleman J, Haak H (2021) Comparison of SIRS criteria and qSOFA score for identifying culture-positive sepsis in the emergency department: a prospective cross-sectional multicentre study. BMJ Open 11(6):e041024
Chiu I-M, Huang Y-H, Su C-M, Kung C-T, Li C-J, Chen C-H, Tang K-S, Kuo K-C (2020) C-Reactive protein concentration can help to identify bacteremia in children visiting the emergency department: a single medical center experience. Pediatr Emerg Care 36(6):291–295
Wu Q, Yang H, Kang Y (2018) Comparison of diagnostic accuracy among procalcitonin, C-reactive protein, and interleukin 6 for blood culture positivity in general ICU patients. Crit Care 22(1):1–2
Author information
Authors and Affiliations
Contributions
Choon-Bing Chua and Yin-Chou Hsu designed the study. Chi-Chieh Hung, Yong-Ye Yang, and Tsung-Han Wang extracted the data and performed statistical analysis. Tsung-Han Wang and Yin-Chou Hsu prepared figures. Choon-Bing Chua, Chi-Chieh Hung, and Yong-Ye Yang prepared tables. Choon-Bing Chua, Chi-Chieh Hung, and Yin-Chou Hsu drafted the manuscript. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This observational study and process of anonymized data acquisition was approved by the Institutional Review Board of E-Da hospital (EMRP-109–044).
Consent to participate
The requirement for informed consent was waived owing to the retrospective observational nature of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chua, CB., Hung, CC., Yang, YY. et al. Comparison between culture-positive and culture-negative septic shock in patients in the emergency department. Eur J Clin Microbiol Infect Dis 41, 1285–1293 (2022). https://doi.org/10.1007/s10096-022-04496-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-022-04496-3