Abstract
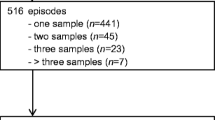
We conducted a retrospective study from 2005 to 2019 to describe the epidemiology and mortality of enterobacterial producing extended-spectrum β-lactamase (E-ESBL) infections in our university hospital over a 17-year period of time. Clinical and microbiological data were extracted from different software used for continuous surveillance. Stool samples from systematic screening for E-ESBL colonization were excluded from the study. The incidence rate of infected patient was calculated by E-ESBL species and by year. A comparison of mortality rate in patients with bloodstream infections versus other types of infections was conducted using a Kaplan–Meier method survival curves. A log rank test (with a risk of 5%) was carried out. A total of 3324 patients with E-ESBL infection were included with an increased incidence density per 1000 days of hospitalization from 0.03 in 2005 to 0.47 in 2019. Escherichia coli was the most frequently isolated pathogen (64%). Global mortality rate was significantly higher with E. coli than with Klebsiella spp. and Enterobacter spp. (p < 0.001). Mortality was higher in patients with E-ESBL bloodstream infection than in patients with other type of E-ESBL infection (p < 0.001). Our study showed a significant increase of the E-ESBL incidence density over a 17-year period survey with a higher mortality in patients with E-ESBL bacteremia. This highlights the need to continue efforts to control the spread of these multi-resistant bacteria in our institution.





Similar content being viewed by others
Data availability
The data analyzed were extracted from the laboratory database of our hospital and from the computerized patient records. The analysis was done in a transparent manner, and the database is available.
Code availability
Not applicable.
References
European Centre for Disease Prevention and Control. Antimicrobial resistance surveillance in Europe: annual report of the European Antimicrobial Resistance Surveillance Network (EARS Net) 2015. LU: Publications Office; 2017 Available at: https://data.europa.eu/doi/10.2900/6928 . Accessed March 8, 2022.
Zahar J-R, Bille E, Schnell D, Lanternier F, Mechai F, Masse V et al (2009) Extension of beta-lactamases producing bacteria is a worldwide concern. Med Sci (Paris) 25(11):939–944
Coque TM, Baquero F, Canton R (2008) Increasing prevalence of ESBL-producing Enterobacteriaceae in Europe. Euro Surveill 13(47).
Observatoire National de l’Epidémiologie de la Resistance Bactérienne aux Antibiotiques. Rapport d’activité annuel 2017. Available at: http://onerba-doc.onerba.org/Rapports/Rapport-ONERBA-2017/ONERBA_rapport_2017.pdf. Accessed March 8, 2022.
Arnaud I, Maugat S, Jarlier V, Astagneau P, National Early Warning, Investigation and Surveillance of Healthcare-Associated Infections Network (RAISIN)/multidrug resistance study group (2015) Ongoing increasing temporal and geographical trends of the incidence of extended-spectrum beta-lactamase-producing Enterobacteriaceae infections in France, 2009 to 2013. Euro Surveill 20(36).
Valverde A, Grill F, Coque TM, Pintado V, Baquero F, Cantón R et al (2008) High rate of intestinal colonization with extended-spectrum-β-lactamase-producing organisms in household contacts of infected community patients. J Clin Microbiol 46(8):2796–2799
Boyer-Mariotte S, Duboc P, Bonacorsi S, Lemeland J-F, Bingen E, Pinquier D (2008) CTX-M-15-producing Escherichia coli in fatal neonatal meningitis: failure of empirical chemotherapy. J Antimicrob Chemother 62(6):1472–1474
Rodríguez-Baño J, Navarro MD, Romero L, Martínez-Martínez L, Muniain MA, Perea EJ et al (2004) Epidemiology and clinical features of infections caused by extended-spectrum beta-lactamase-producing Escherichia coli in non hospitalized patients. J Clin Microbiol 42(3):1089–1094
Santé Publique France. Bactéries multirésistantes en établissements de santé en 2018 Mission nationale Spares, novembre 2019. Données 2018 du réseau BMR-Raisin. Availble at: /import/bacteries-multiresistantes-en-etablissements-de-sante-en-2018-mission-nationale-spares-novembre-2019.-donnees-2018-du-reseau-bmr-raisin. Accessed March 8, 2022.
Lambert M-L, Suetens C, Savey A, Palomar M, Hiesmayr M, Morales I et al (2011) Clinical outcomes of health-care-associated infections and antimicrobial resistance in patients admitted to European intensive-care units: a cohort study. Lancet Infect Dis 11(1):30–38
Barbier F, Lisboa T, Nseir S (2016) Understanding why resistant bacteria are associated with higher mortality in ICU patients. Intensive Care Med 42(12):2066–2069
McNamara JF, Righi E, Wright H, Hartel GF, Harris PNA, Paterson DL (2018) Long-term morbidity and mortality following bloodstream infection: a systematic literature review. J Infect 77(1):1–8
Bearman GML, Wenzel RP (2005) Bacteremias: a leading cause of death. Arch Med Res 36(6):646–659
Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB (2004) Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis 39(3):309–317
de Kraker MEA, Wolkewitz M, Davey PG, Koller W, Berger J, Nagler J et al (2011) Burden of antimicrobial resistance in European hospitals: excess mortality and length of hospital stay associated with bloodstream infections due to Escherichia coli resistant to third-generation cephalosporins. J Antimicrob Chemother 66(2):398–407
Drieux L, Brossier F, Duquesnoy O, Aubry A, Robert J, Sougakoff W et al (2009) Increase in hospital-acquired bloodstream infections caused by extended spectrum beta-lactamase-producing Escherichia coli in a large French teaching hospital. Eur J Clin Microbiol Infect Dis 28(5):491–498
Maslikowska JA, Walker SAN, Elligsen M, Mittmann N, Palmay L, Daneman N et al (2016) Impact of infection with extended-spectrum β-lactamase-producing Escherichia coli or Klebsiella species on outcome and hospitalization costs. J Hosp Infect 92(1):33–41
MacVane SH, Tuttle LO, Nicolau DP (2014) Impact of extended-spectrum β-lactamase-producing organisms on clinical and economic outcomes in patients with urinary tract infection. J Hosp Med 9(4):232–238
Noël A, Vastrade C, Dupont S, de Barsy M, Huang TD, Van Maerken T et al (2019) Nosocomial outbreak of extended-spectrum β-lactamase-producing Enterobacter cloacae among cardiothoracic surgical patients: causes and consequences. J Hosp Infect 102(1):54–60
Haut Conseil de la santé publique (HCSP). Prévenir l’émergence des entérobactéries BLSE et lutter contre leur dissémination [Internet]. Rapport de l’HCSP. Paris: Haut Conseil de la Santé Publique; 2010. Available at: https://www.hcsp.fr/explore.cgi/avisrapportsdomaine?clefr=162. Accessed March 8, 2022.
Société française d’hygiène hospitalière (2009) Recommandations nationales - Prévention de la transmission croisée : précautions complémentaires contact - Consensus formalisé d’experts - 2009;60.
Carbonne A, Arnaud I, Maugat S, Marty N, Dumartin C, Bertrand X et al (2013) National multidrug-resistant bacteria (MDRB) surveillance in France through the RAISIN network: a 9 year experience. J Antimicrob Chemother 68(4):954–959
Jarlier V, Trystram D, Brun-Buisson C, Fournier S, Carbonne A, Marty L et al (2010) Curbing methicillin-resistant Staphylococcus aureus in 38 French hospitals through a 15-year institutional control program. Arch Intern Med 170(6):552–559
Kassakian SZ, Mermel LA (2014) Changing epidemiology of infections due to extended spectrum beta-lactamase producing bacteria. Antimicrob Resist Infect Control 3:9
Marra AR, Edmond MB, Schweizer ML, Ryan GW, Diekema DJ (2018) Discontinuing contact precautions for multidrug-resistant organisms: a systematic literature review and meta-analysis. Am J Infect Control 46(3):333–340
Tacconelli E, Cataldo MA, Dancer SJ, De Angelis G, Falcone M, Frank U et al (2014) ESCMID guidelines for the management of the infection control measures to reduce transmission of multidrug-resistant Gram-negative bacteria in hospitalized patients. Clin Microbiol Infect 20(Suppl 1):1–55
Kirkland KB, Weinstein RA (2009) Taking off the gloves: toward a less dogmatic approach to the use of contact isolation. Clin Infect Dis 48(6):766–771
Kluytmans-van den Bergh MFQ, Bruijning-Verhagen PCJ, Vandenbroucke-Grauls CMJE, de Brauwer EIGB, Buiting AGM, Diederen BM et al (2019) Contact precautions in single-bed or multiple-bed rooms for patients with extended-spectrum β-lactamase-producing Enterobacteriaceae in Dutch hospitals: a cluster-randomised, crossover, non-inferiority study. Lancet Infect Dis 19(10):1069–79
Zahar J-R, Poirel L, Dupont C, Fortineau N, Nassif X, Nordmann P (2015) About the usefulness of contact precautions for carriers of extended-spectrum beta-lactamase-producing Escherichia coli. BMC Infect Dis 15(1):512
Scheuerman O, Schechner V, Carmeli Y, Gutiérrez-Gutiérrez B, Calbo E, Almirante B et al (2018) Comparison of predictors and mortality between bloodstream infections caused by ESBL-producing Escherichia coli and ESBL-producing Klebsiella pneumoniae. Infect Control Hosp Epidemiol 39(6):660–667
Leistner R, Gürntke S, Sakellariou C, Denkel LA, Bloch A, Gastmeier P et al (2014) Bloodstream infection due to extended-spectrum beta-lactamase (ESBL)-positive K. pneumoniae and E. coli: an analysis of the disease burden in a large cohort. Infection 42(6):991–7
Sakellariou C, Gürntke S, Steinmetz I, Kohler C, Pfeifer Y, Gastmeier P et al (2016) Sepsis caused by extended-spectrum beta-lactamase (ESBL)-positive K. pneumoniae and E. coli: comparison of severity of sepsis, delay of anti-infective therapy and ESBL genotype. PLoS One 11(7):e0158039
Leistner R, Bloch A, Gastmeier P, Schwab FE (2016) coli bacteremia in comparison to K. pneumoniae bacteremia: influence of pathogen species and ESBL production on 7-day mortality. Antimicrob Resist Infect Control 5:37
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Camille Bouchand and Didier Lepelletier. The first draft of the manuscript was written by Camille Bouchand and Didier Lepelletier, and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
We declared that compliance with ethical standard was followed during the study period.
Consent to participate
Not applicable.
Consent for publication
All the authors have declared their consent for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bouchand, C., Andréo, A., Le Gallou, F. et al. Retrospective analysis of a large single cohort of Enterobacteriaceae producing extended-spectrum B-lactamase (E-ESBL) patients: incidence, microbiology, and mortality. Eur J Clin Microbiol Infect Dis 41, 1237–1243 (2022). https://doi.org/10.1007/s10096-022-04489-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-022-04489-2