Abstract
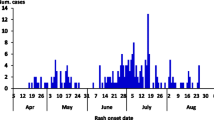
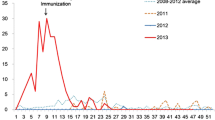
We describe a measles outbreak among previously vaccinated healthcare workers (HCWs) and inpatients and the control measures implemented at a tertiary care hospital in 2019. Case-patients were laboratory-confirmed measles with throat swabs tested by quantitative polymerase chain reactions (PCR), during April–May 2019. Medical histories and documented immunization records were obtained. We compared attack rates (ARs) among HCWs by occupational subgroup and age and examined the outbreak-associated costs. The index case was not ascertained. Among 26 measles case-patients (22 HCWs, four inpatients) aged 18–28 years, 25 had previously received measles–mumps–rubella (MMR) vaccine (12/26, 46% (two doses); 13/26, 50% (one dose)), and 16 (62%) had positive results of measles IgG prior to measles diagnosis. ARs were higher among HCWs aged < 30 years (1.88%), especially in the subgroup under 25 years of age (2.22%). Control measures included work restrictions for seronegative HCWs (218/2320, 9.4%) in immunity verification, administration of the MMR vaccine (207 HCWs) or intravenous immunoglobulin (2 HCWs and 11 inpatients), enhanced health surveillance of HCWs, and mandatory assessment of patients with measles-like symptoms at the infectious diseases screening units. The hospital spent 90,417,132 Korean won (US $79,733) in response to the outbreak. Measles outbreaks can occur in healthcare settings despite high population immunity, highlighting the importance of stronger vaccination policies, particularly among young HCWs. Moreover, an effective outbreak response comprising immunization activities and enhanced surveillance of HCWs and patients to rapidly detect measles-like symptoms at a prodromal phase is essential to control nosocomial measles outbreaks.




Similar content being viewed by others
Availability of data and material
The data are available upon reasonable request by contacting the corresponding author.
References
Guerra FM, Bolotin S, Lim G, Heffernan J, Deeks SL, Li Y, Crowcroft NS (2017) The basic reproduction number (R0) of measles: a systematic review. Lancet Infect Dis 17:e420–e428. https://doi.org/10.1016/S1473-3099(17)30307-9
Steingart KR, Thomas AR, Dykewicz CA, Redd SC (1999) Transmission of measles virus in healthcare settings during a communitywide outbreak. Infect Control Hosp Epidemiol 20:115–119. https://doi.org/10.1086/501595
Choi WS, Sniadack DH, Jee Y, Go UY, So JS, Cho H, Bae GR, Lee DH, Kim K, Yoon HS, Chung YS, Kang C, Park H, Park O, Lee JK (2011) Outbreak of measles in the Republic of Korea, 2007: importance of nosocomial transmission. J Infect Dis 204:S483–S490. https://doi.org/10.1093/infdis/jir087
Hagan JE, Takashima Y, Sarankhuu A, Dashpagma O, Jantsansengee B, Pastore R, Nyamaa G, Yadamsuren B, Mulders MN, Wannemuehler KA, Anderson R, Bankamp B, Rota P, Goodson JL (2017) Risk factors for measles virus infection among adults during a large outbreak in post elimination era in Mongolia, 2015. J Infect Dis 216:1187–1195. https://doi.org/10.1093/infdis/jix449
Botelho-Nevers E, Gautret P, Biellik R, Brouqui P (2012) Nosocomial transmission of measles: an updated review. Vaccine 30:3996–4001. https://doi.org/10.1016/j.vaccine.2012.04.023
Maltezou HC, Wicker S (2013) Measles in health care settings. Am J Infect Control 41:661–663. https://doi.org/10.1016/j.ajic.2012.09.017
Cherry JD, Zahn M (2018) Clinical characteristics of measles in previously vaccinated and unvaccinated patients in California. Clin Infect Dis 67:1315–1319. https://doi.org/10.1093/cid/ciy286
Rota JS, Hickman CJ, Sowers SB, Rota PA, Mercader S, Bellini WJ (2011) Two case studies of modified measles in vaccinated physicians exposed to primary measles cases: high risk of infection but low risk of transmission. J Infect Dis 204:S559–S563. https://doi.org/10.1093/infdis/jir098
Choe YJ, Park YJ, Kim JW, Eom HE, Park O, Oh MD, Lee JK (2017) An outbreak of measles in a university in Korea, 2014. J Korean Med Sci 32:1876–1878. https://doi.org/10.3346/jkms.2017.32.11.1876
Sá Machado R, Perez Duque M, Almeida S, Cruz I, Sottomayor A, Almeida I, Oliveira JR, Antunes D (2018) Measles outbreak in a tertiary level hospital, Porto, Portugal, 2018: challenges in the post-elimination era. Euro Surveill 23:18–00224. https://doi.org/10.2807/1560-7917.ES.2018.23.20.18-00224
Gohil SK, Okubo S, Klish S, Dickey L, Huang SS, Zahn M (2016) Healthcare workers and post-elimination era measles: lessons on acquisition and exposure prevention. Clin Infect Dis 62:155–172. https://doi.org/10.1093/cid/civ802
Hahné SJ, Nic Lochlainn LM, van Burgel ND, Kerkhof J, Sane J, Yap KB, van Binnendijk RS (2016) Measles outbreak among previously immunized healthcare workers, the Netherlands, 2014. J Infect Dis 214:1980–1986. https://doi.org/10.1093/infdis/jiw480
Hickman CJ, Hyde TB, Sowers SB, Mercader S, McGrew M, Williams NJ, Beeler JA, Audet S, Kiehl B, Nandy R, Tamin A, Bellini WJ (2011) Laboratory characterization of measles virus infection in previously vaccinated and unvaccinated individuals. J Infect Dis 204:S549–S558. https://doi.org/10.1093/infdis/jir106
Kontio M, Jokinen S, Paunio M, Peltola H, Davidkin I (2012) Waning antibody levels and avidity: implications for MMR vaccine-induced protection. J Infect Dis 206:1542–1548. https://doi.org/10.1093/infdis/jis568
Avramovich E, Indenbaum V, Haber M, Amitai Z, Tsifanski E, Farjun S, Sarig A, Bracha A, Castillo K, Markovich MP, Galor I (2018) Measles outbreak in highly vaccinated population – Israel, July-August 2017. MMWR Morb Mortal Wkly Rep 67:1186–1188. https://doi.org/10.15585/mmwr.mm6742a4
Mizumoto K, Kobayashi T, Chowell G (2018) Transmission potential of modified measles during an outbreak, Japan, March-May 2018. Euro Surveill 23:1800239. https://doi.org/10.2807/1560-7917.ES.2018.23.24.1800239
Gibney KB, Attwood LO, Nicholson S, Tran T, Druce J, Healy J, Strachan J, Franklin L, Hall R, Cross GB (2020) Emergence of attenuated measles illness among IgG-positive/IgM-negative measles cases: Victoria, Australia, 2008–2017. Clin Infect Dis 70:1060–1067. https://doi.org/10.1093/cid/ciz363
Rosen JB, Rota JS, Hickman CJ, Sowers SB, Mercader S, Rota PA, Bellini WJ, Huang AJ, Doll MK, Zucker JR, Zimmerman CM (2014) Outbreaks of measles among persons with prior evidence of immunity, New York City, 2011. Clin Infect Dis 58:1205–1210. https://doi.org/10.1093/cid/ciu105
Kang JH (2020) Review of measles in Korea: quarantine and elimination. Infect Chemother 52:113–122. https://doi.org/10.3947/ic.2020.52.1.113
Choe YJ, Jee Y, Oh MD, Lee JK (2015) Measles elimination activities in the Western Pacific Region: experience from the Republic of Korea. J Korean Med Sci 30:S115-121. https://doi.org/10.3346/jkms.2015.30.S2.S115
Yang TU, Kim JW, Eom HE, Oh HK, Kim ES, Kang HJ, Nam JG, Kim KS, Kim SS, Lee CK, Park YJ, Park O (2015) Resurgence of measles in a country of elimination: interim assessment and current control measures in the Republic of Korea in early 2014. Int J Infect Dis 33:12–14. https://doi.org/10.1016/j.ijid.2014.09.016
Helfand RF, Heath JL, Anderson LJ, Maes EF, Guris D, Bellini WJ (1997) Diagnosis of measles with and IgM capture EIA: the optimal timing of specimen collection after rash onset. J Infect Dis 175:195–199. https://doi.org/10.1093/infdis/175.1.195
Cho HJ, Kang HJ (2014) Genotype analysis of measles outbreaks in Korea 2013. Public Health Wkly Rep 7:470–475
McLean HQ, Fiebelkorn AP, Temte JL, Wallace GS, Centers for Disease Control and Prevention, (2013) Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: summary recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep 62:1–34
Venkat H, Briggs G, Brady S, Komatsu K, Hill C, Leung J, Patel M, Livar E, Su CP, Kassem A, Sowers SB, Mercader S, Rota PA, Elson D, Timme E, Robinson S, Fitzpatrick K, Franco J, Hickman C, Gastañaduy PA (2019) Measles outbreak at a privately operated detention facility: Arizona, 2016. Clin Infect Dis 68:2018–2025. https://doi.org/10.1093/cid/ciy819
Botelho-Nevers E, Cassir N, Minodier P, Laporte R, Gautret P, Badiaga S, Thiberville DJ, Ninove L, Charrel R, Brouqui P (2011) Measles among healthcare workers: a potential for nosocomial outbreaks. Euro Surveill 16:19764
Barrett P, Cotter S, Ryan F, Connell J, Cronin A, Ward M, Fitzgerald R, Lynch C, Margiotta T, on Behalf of the Outbreak Control Team (2018) A national measles outbreak in Ireland linked to a single imported case, April to September, 2016. Euro Surveill 23:1700655. https://doi.org/10.2807/1560-7917.ES.2018.23.31.1700655
Chen SY, Anderson S, Kutty PK, Lugo F, McDonald M, Rota PA, Ortega-Sanchez IR, Komatsu K, Armstrong GL, Sunenshine R, Seward JF (2011) Healthcare-associated measles outbreak in the United States after an importation: challenges and economic impact. J Infect Dis 203:1517–1525. https://doi.org/10.1093/infdis/jir115
Biribawa C, Atuhairwe JA, Bulage L, Okethwangu DO, Kwesiga B, Ario AR, Zhu BP (2020) Measles outbreak amplified in a pediatric ward: Lyantonde district, Uganda, August 2017. BMC Infect Dis 20:398. https://doi.org/10.1186/s12879-020-05120-5
Porretta A, Quattrone F, Aquino F, Pieve G, Bruni B, Gemignani G, Vatteroni ML, Pistello M, Privitera GP, Lopalco PL (2017) A nosocomial measles outbreak in Italy, February-April 2017. Euro Surveill 22:30597. https://doi.org/10.2807/1560-7917.ES.2017.22.33.30597
Jia H, Ma C, Lu M, Fu J, Rodewald LE, Su Q, Wang H, Hao L (2018) Transmission of measles among healthcare workers in hospital W, Xinjiang autonomous region, China, 2016. BMC Infect Dis 18:36. https://doi.org/10.1186/s12879-018-2950-y
Kang HJ, Han YW, Kim SJ, Kim YJ, Kim AR, Kim JA, Jung HD, Eom HE, Park O, Kim SS (2017) An increasing, potentially measles-susceptible population over time after vaccination in Korea. Vaccine 35:4126–4132. https://doi.org/10.1016/j.vaccine.2017.06.058
Chang HH, Kim SW, Kwon KT, Kim HI, Kim MJ, Ryu SY, Kim HA, Hur J, Kwon HH, Hong HL (2019) Preliminary report of seroprevalence of anti-measles immunoglobulin G among healthcare workers of 6 teaching hospitals of Daegu, Korea in 2019. Infect Chemother 51:54–57. https://doi.org/10.3947/ic.2019.51.1.54
Jung J, Kim SK, Kwak SH, Hong MJ, Kim SH (2019) Seroprevalence of measles in healthcare workers in South Korea. Infect Chemother 51:58–61. https://doi.org/10.3947/ic.2019.51.1.58
Maltezou HC, Wicker S, Borg M, Heininger U, Puro V, Theodoridou M, Poland GA (2011) Vaccination policies for health-care workers in acute health-care facilities in Europe. Vaccine 29:9557–9562
Maltezou HC, Botelho-Nevers E, Brantsæter AB et al (2019) Vaccination of healthcare personnel in Europe: update to current policies. Vaccine 37:7576–7584. https://doi.org/10.1016/j.vaccine.2011.09.076
Fiebelkorn AP, Seward JF, Orenstein WA (2014) A global perspective of vaccination of healthcare personnel against measles: systematic review. Vaccine 32:4823–4839. https://doi.org/10.1016/j.vaccine.2013.11.005
Six C, Blanes de Canecaude J, Duponchel J, Lafont E, Decoppet A, Travanut M, Pingeon J, Coulon L, Peloux-Petiot F, Grenier-Tisserant P, Delaroziere J, Charlet F, Malfait P (2010) Spotlight on measles 2010: measles outbreak in the Provence-Alpes-Cote d Azur region, France, January to November 2010 - substantial underreporting of cases. Euro Surveill 15:19754
Park SH, Lee MS, Kim SR, Kwak YG (2020) A national survey on the hospital vaccination policies in Korea. J Korean Med Sci 35:e76. https://doi.org/10.3346/jkms.2020.35.e76
Lindley M, Horlick G, Shefer A, Shaw F, Gorji M (2007) Assessing state immunization requirements for healthcare workers and patients. Am J Prev Med 32:459–465. https://doi.org/10.1016/j.amepre.2007.02.009
Sydnor E, Perl TM (2014) Healthcare providers as sources of vaccine-preventable diseases. Vaccine 32:4814–4822. https://doi.org/10.1016/j.vaccine.2014.03.097
Lefebvre F, Merle V, Savoye G, Lemée V, Chapuzet C, Marini H, Géhanno JF, Chefson-Girault C, Gueit I, Freymuth F, Lerebours E, Czernichow P (2011) Nosocomial transmission of measles: do we need extra precautions to avoid it? J Hosp Infect 79:185–187. https://doi.org/10.1016/j.jhin.2011.05.025
Fu J, Chu J, Wang J, Cai R, Cheng W, Shi L, Zhang F, Xu Z, Xing Y (2019) A hospital-associated measles outbreak in health workers in Beijing: implications for measles elimination in China, 2018. Int J Infect Dis 78:85–92. https://doi.org/10.1016/j.ijid.2018.10.023
Author information
Authors and Affiliations
Contributions
(1) Conception and design: SS and YKK; (2) acquisition of data and administrative support: SS and JML; (3) provision of study materials or patients: BRL, JYC, JY, SNL, and MYJ; (4) collection and assembly of data: HWK; (5) data analysis and interpretation: HSK, SMM, and YKK; (6) manuscript writing: all authors; (7) final approval of manuscript: all authors.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the hospital ethics committee.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interests
The authors declare that they have no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Song, K., Lee, J.M., Lee, E.J. et al. Control of a nosocomial measles outbreak among previously vaccinated adults in a population with high vaccine coverage: Korea, 2019. Eur J Clin Microbiol Infect Dis 41, 455–466 (2022). https://doi.org/10.1007/s10096-021-04390-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-021-04390-4