Abstract
Prosthetic joint infection (PJI) is a feared and challenging to diagnose complication after arthroplasty, with Staphylococcus epidermidis as the major pathogen. One important criteria to define PJI is the detection of phenotypically indistinguishable microorganisms with identical antibiotic susceptibility pattern in at least two different samples. However, owing to phenotypical variation within genetic clones and clonal variation within a phenotype, the criteria may be ambiguous. We investigated the extent of diversity among coagulase-negative staphylococci (CoNS) in PJI and characterised S. epidermidis isolates from PJI samples, specifically multiple S. epidermidis isolates identified in individual PJI patients. We performed a retrospective cohort study on 62 consecutive patients with PJI caused by CoNS from two hospitals in Northern Sweden. In 16/62 (26%) PJIs, multiple S. epidermidis isolates were available for whole-genome analyses. Hospital-adapted multidrug-resistant genetic clones of S. epidermidis were identified in samples from 40/62 (65%) of the patients using a combination of pulsed-field gel electrophoresis and multilocus sequence typing. Whole-genome sequencing showed the presence of multiple sequence types (STs) in 7/16 (44%) PJIs where multiple S. epidermidis isolates were available. Within-patient phenotypical variation in the antibiotic susceptibility and/or whole-genome antibiotic resistance gene content was frequent (11/16, 69%) among isolates with the same ST. The results highlight the ambiguity of S. epidermidis phenotypic characterisation as a diagnostic method in PJI and call for larger systematic studies for determining the frequency of CoNS diversity in PJIs, the implications of such diversity for microbiological diagnostics, and the therapeutic outcomes in patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prosthetic joint replacement is one of the most important medical innovations of the twentieth century, and it has significantly improved the quality of life for millions of individuals worldwide by providing pain relief and restoring joint function, mobility, and independence [1, 2]. However, prosthetic joint infection (PJI) following joint replacement is a devastating complication associated with high medical costs and increased in-hospital mortality [3]. Both PJI diagnosis and treatment are challenging [4]. Previous studies have shown that Staphylococcus aureus and coagulase-negative staphylococci (CoNS), and in particular Staphylococcus epidermidis, are the pathogenic agents in most PJIs [5].
Currently, the international clinical guidelines for defining PJI diagnosis require two positive periprosthetic cultures with phenotypically ‘identical’ or ‘indistinguishable’ organisms, with the phenotype determined using common laboratory tests for genus and species identification and antibiograms [6,7,8]. Since phenotypic morphological variations [9], including the presence of small colony variants and different antibiograms, have been reported in monoclonal CoNS infections [10,11,12], the term ‘phenotypically identical organisms’ is ambiguous. Furthermore, the assessment of CoNS in clinical cultures is demanding as CoNS are a ubiquitous part of the human skin microbiota and often for S. epidermidis display high sub-species heterogeneity [13, 14], which makes distinction between contamination and true infection challenging. Here, we investigated the extent of diversity among CoNS in PJI and characterised in detail the S. epidermidis in these infections which revealed substantial within-patient diversity further highlighting the complexity and ambiguity in the current phenotypical assessment as the diagnostic criteria.
Methods
Study population
The patients in the study population were recruited from two hospitals in Northern Sweden: Umeå University Hospital and Östersund County Hospital. All patients were identified using the laboratory information systems and based on the presence of CoNS in more than two periprosthetic tissue biopsies retrieved during revision surgery in patients with clinically suspected PJI between December 2008 and June 2011. Diagnosis was based on the PJI diagnostic criteria of the Infectious Disease Society of America (IDSA, www.idsociety.org), ‘identical microorganisms isolated from two or more cultures’ [7], and classified according to the time point of occurrence after implantation: acute, within 1–3 months; delayed, 3 months to 1 year; late, after more than 1 year [6]. The medical records of the patients were reviewed for additional data on concomitant diseases, previous hospitalisation during the preceding year, intraoperative clinical findings by the surgeon, surgical treatment of PJI, and outcome at 2-year follow-up.
Bacterial isolates
CoNS cultured from more than two perioperative tissue specimens (obtained during revision surgery of patients with clinically suspected PJI) were evaluated. Based on differences in colony morphology (i.e., size, consistency, luster, and colour), one to two isolates resembling CoNS were collected from each tissue culture for further investigation. The bacterial isolates were stored at − 70 °C in preservation media (Trypticase Soy Broth, BD Diagnostic Systems, Sparks, MD, USA) until further examination. In total, 131 CoNS isolates collected from 62 patients with PJIs were included for antimicrobial susceptibility testing and pulsed-field gel electrophoresis (PFGE). Only one isolate was available for PFGE and MLST in 40/62 (65%) patients with PJIs. Multiple CoNS isolates were available from 22 PJIs; 18 caused by S. epidermidis, two Staphylococcus capitis, one Staphylococcus caprae, and one Staphylococcus hominis. We were not able to recultivate multiple isolates of S. epidermidis for WGS in two PJIs. Hence, multiple S. epidermidis (n = 69) isolates collected from 16 patients were available for whole-genome sequencing (WGS) (Supplementary Figs. S1 and S2).
Identification
Species-level identification was performed using matrix-assisted laser resorption/ionisation time-of-flight mass spectrometry (MALDI-TOF MS) with a Microflex LT (Bruker Daltonik GmbH, Bremen, Germany) and MALDI Biotyper software v3.1 DB7311 (Bruker Daltonik), according to the manufacturer’s instructions. A score > 2.0 was required for species identification [15].
Antimicrobial susceptibility testing
Antimicrobial susceptibility was tested using disc diffusion according to the recommendations of the European Committee on Antimicrobial Susceptibility Testing (EUCAST, http://www.eucast.org) with the following eight antimicrobials: cefoxitin, clindamycin, erythromycin, fusidic acid, gentamicin, norfloxacin, rifampicin, and trimethoprim/sulfamethoxazole. The clinical breakpoints were the same as those specified in the EUCAST recommendation (v10.0). Vancomycin heteroresistance was not tested. Multidrug resistance (MDR) was defined as resistance towards antimicrobials from more than three classes.
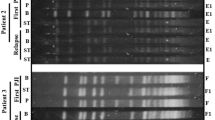
PFGE and multilocus sequence typing (MLST)
PFGE and MLST were performed as previously described [16]. In short, DNA was prepared from 3 mL S. epidermidis overnight cultures in Todd Hewitt broth (Difco Laboratories). The DNA was digested using SmaI (Thermo Fisher Scientific, Waltham, MA, USA), and the DNA fragments were separated by PFGE in a GenePath apparatus (Bio-Rad Laboratories) using Program 14, for 19.7 h according to the manufacturer’s instructions (Bio-Rad). Gels were stained in 1 mg/L ethidium bromide, destained, and photographed under UV illumination. Genetic similarity between isolates was calculated using GelCompar II 4.0 (Applied Maths) using the Dice coefficient, and the unweighted pair group method with arithmetic mean (UPGMA) with 1.3% tolerance and 0.8% optimization settings. S. aureus NCTC 8325 was included as a reference in every sixth to seventh lane to allow normalisation of the electrophoretic pattern. Band sizes below 36 kb were not analysed. PFGE types were visually identified according to established criteria; isolates with more than three-band variation in the PFGE pattern were defined as genetically unrelated. This corresponded to a similarity coefficient of 90% using the cluster analysis.
PFGE was performed using all isolates (n = 131). All unique S. epidermidis PFGE types that included at least three isolates were further analysed using MLST (n = 102) according to Thomas et al. [17]. The 7 housekeeping genes were amplified by PCR, and both strands of all amplicons were sequenced with an Applied Biosystems 3730xl DNA Analyser by using BigDye Terminator v3.1 cycle sequencing kit. Sequence types (STs) were assigned using the S. epidermidis MLST database (https://pubmlst.org/sepidermidis/).
Genome sequencing and analyses
WGS was performed on the 69 S. epidermidis isolates collected from 16 patients with PJI using Illumina MiSeq and the 300-cycle MiSeq Reagent Kit v3 to generate paired-end 150-bp reads according to the manufacturer’s instructions. DNA purification was performed using the Qiagen Blood and Tissue kit. The sequencing data were subjected to quality control using bifrost (https://github.com/ssi-dk/bifrost) to ensure adequate sequencing quality of all isolates and assembled using SPAdes v3.9.0 [18]. After the duplicated regions in the reference were eliminated using NUCmer, the raw reads were aligned against the S. epidermidis ATCC 12,228 reference chromosome (GenBank accession ID CP0222479) for detecting single nucleotide polymorphisms (SNPs) using NASP v1.0.0 [19]. NASP was also used to detect intraspecies contamination. All positions with < tenfold coverage or cases where the variant was present in < 90% of the base calls were excluded using GATK [20]. The SNPs identified in the core genome were used to infer phylogenetic relationships using PhyML v3 [21] with Smart Model Selection [22]. The resistance mechanisms were determined as previously described [23].
Statistics
Statistical analyses were performed using the SPSS v24 (SPSS Inc., Chicago, IL, USA) software package. Fisher’s exact test was used to test association in all two-way tables. A value with p < 0.05 was considered significant.
Research ethics
The study was approved by the Research Ethics Committee (No 2012–477-31 M) of the Faculty of Medicine, Umeå University, Sweden. All study participants provided written informed consent prior to study participation.
Results
Clinical characteristics
The clinical characteristics of 62 consecutive patients (34 men and 28 women; median age 68.6 years) requiring revision or resection arthroplasties for CoNS-related PJIs are presented in Table 1.
Microbiological findings and genetic analyses
In total, 131 CoNS isolates as determined using MALDI-TOF MS were available from 62 patients with PJI, with S. epidermidis (n = 107; 85%), Staphylococcus capitis (n = 11; 8%), and Staphylococcus hominis (n = 8; 4%) as the most frequent species (Table 2, Supplementary Fig. S1). PFGE analysis of all 131 isolates and subsequent MLST on selected S. epidermidis PFGE types revealed two major clusters corresponding to ST215 and ST2 (Supplementary Fig. S2). In addition, two single locus variants (SLVs) of ST215 (ST434) and ST2 (ST188) were identified, and the major clusters, including the SLVs, were denoted as the ST215 and ST2 lineages, respectively (Fig. 1). Among S. epidermidis isolates, the antimicrobial resistance rates were as follows: cefoxitin (80%), gentamicin (90%), norfloxacin (79%), trimethoprim-sulfamethoxazole (75%), clindamycin (63%), fusidic acid (42%), and rifampicin 33% (Supplementary Table S2). No resistance to linezolid was detected. Significant differences in antimicrobial susceptibility were identified when the two major genetic clusters were compared. All 32 isolates of the ST215 lineage exhibited fusidic acid resistance compared to 21% in the ST2 lineage (p < 0.0001). In contrast, rifampicin resistance was significantly more common among isolates in the ST2 lineage (27/47, 57%) than in the ST215 lineage (5/32, 16%) (p = 0.0002).
Midpoint-rooted maximum-likelihood phylogeny of 69 Staphylococcus epidermidis prosthetic joint infection isolates from 16 patients. Information on sequence type, genes associated with antimicrobial resistance is presented along with the patient number. The scale bar indicates the substitutions per site. The black blocks indicate the presence of genes mediating antibiotic resistance or previously associated with virulence
Phenotypic diversity of CoNS in PJI
The majority (43/62; 69%) of the PJIs were monomicrobial, with S. epidermidis detected in most PJIs (n = 33), followed by S. capitis (n = 5) and S. hominis (n = 2) (Table 2, Supplementary Table S3). S. epidermidis was also detected in all 19 polymicrobial PJIs, most frequently in combination with Enterococcus faecalis (n = 7), Escherichia coli (n = 3), or S. hominis (n = 2), and with similar frequencies in hip and knee revision arthroplasties with 11/37 (30%) and 6/20 (33%), respectively.
The presence of a sinus tract with communication to the joint in PJI was reported in only 2/19 (11%) polymicrobial S. epidermidis PJIs.
Whole-genome analyses of S. epidermidis in PJIs
In 16 of the 62 cases of PJI, 9 of which were monomicrobial infections, multiple S. epidermidis isolates (n = 69) from different samples collected from the same patient were available for WGS (Supplementary Figs. S1 and S3, Table 3). Between two to nine isolates were available per patient, and genomic analysis of these isolates helped identify three major lineages: ST59/ST965 in two PJIs, ST215 in five PJIs, and ST2 in nine PJIs (Fig. 1). Nine of the sixteen (56%) patients were infected by bacteria from a single S. epidermidis lineage, whereas seven (44%) patients were infected by bacteria from two to five different S. epidermidis lineages (Fig. 2). Based on a 73% (1.83 Mb) core genome conservation across all the sequenced S. epidermidis PJI isolates, we found that the within-patient genetic diversity among isolates from individual STs ranged from 10 to 107 SNPs, whereas among isolates from PJIs caused by bacteria from multiple STs, 100 to 39,618 SNPs were detected (Fig. 3, Supplementary Table S1).
Resistance determinants in S. epidermidis lineages
The presence of phenotypic antimicrobial resistance and antimicrobial resistance genes identified using WGS was highly concordant (Supplementary Table S4). Our analyses showed that some antibiotic resistance genes were also associated with the STs (Fig. 1, Supplementary Table S1): fusB acid and tet(K), conferring resistance to fusidic acid and tetracycline respectively, were detected only in ST215/ST434, ST188, and ST59. Likewise, mutations in gyr(A), conferring resistance to fluoroquinolones, were detected in isolates belonging to ST2, ST22, and ST215, whereas rpoB mutations conferring rifampicin resistance were identified in both ST2 lineages and in ST434 isolates, but not in any of the ST215 isolates (Fig. 1, Table S1).
Within-patient variations in phenotypic and genotypic resistance
When we compared multiple S. epidermidis isolates collected from each patient with PJI, variations in antibiograms were identified in 13 of the 16 (81%) cases (Table 4). Differences in susceptibility to one to five antimicrobials were observed (Fig. 1, Table 3), with colony polymorphism among isolates observed in samples collected from all patients (data not shown). The variation in detected antibiotic resistance genes was also apparent when multiple isolates of the same ST collected from one patient were compared (Fig. 1, Supplementary Table S1); in patient 1, six out of seven ST215 isolates varied in genetic content with respect to mecA, tet(K), ermC, and mutations in folA.
Discussion
Here, we investigated the diversity among CoNS in PJI and characterised in detail the S. epidermidis isolates from these infections. We found considerable within-patient diversity in S. epidermidis isolates, with variations in phenotypic and genotypic resistance observed in the majority (13/16; 81%) of cases, and also between isolates with the same ST. Additionally, while we considered the inherent difficulty of ruling out the possibility that a single S. epidermidis isolate represents contamination, S. epidermidis isolates belonging to different STs were detected in several PJIs (7/16; 44%). These findings further add to the complexity in assessing whether S. epidermidis identified in multiple cultures in potential PJI cases represent phenotypically identical organisms in two positive periprosthetic cultures. Hence, with the present guidelines, there is a risk that PJI pathogens are incorrectly dismissed as contaminants, which hinders the appropriate microbial diagnosis and treatment.
To date, limited data has been published on the within-patient genetic diversity of CoNS isolates in PJI. Here, we showed that while only a single ST was detected in the majority (9/16, 56%) of the PJIs, polyclonality was detected in 44% (7/16) of all PJIs with between two to five different STs. Importantly, when at least three S. epidermidis isolates from different tissue samples were characterised in each PJI, the extent of the identified within-patient diversity among S. epidermidis isolates increased. Within-patient variation in antibiograms was observed comparing S. epidermidis isolates in almost all patients (10/11, 91%) and different STs were identified in 5/11 (45%). Obviously, among PJIs in which only two S. epidermidis isolates were available for characterisation, polyclonal infection was detected less frequently (2/5 patients; Table 3). These results are consistent with those of a recent German study in which paired isolates from 55 cases of orthopaedic device-related infection were analysed, and 6/55 (11%) cases assessed as polyclonal [24]. Therefore, increasing the number of S. epidermidis isolates for characterisation, and preferably obtaining isolates from different tissue specimens, is important for determining isolate diversity and reduces the risk of incorrect dismissal of isolates as contaminants, and improves the basis for decisions on antibiotic therapy and accurate identification of a relapse or reinfection.
In agreement with previous data, isolates from HA-MDRSE lineages were the cause of most S. epidermidis PJIs over a period of more than 2 years in the two hospitals in Northern Sweden [23, 25]. The low pairwise diversity in the ST215 lineage observed in two PJI cases for which isolates were collected more than 1 year apart in the same hospital (2 SNPs), indicates that the ST215 lineage is persistent in the hospital setting in Sweden. In contrast, limited hospital-adapted transmission of genetic lineages has been reported in S. aureus PJIs [26]. The findings of this study are in alignment with a previously described scenario of the global dissemination of multidrug-resistant lineages of S. epidermidis [27, 28]. The likelihood of hospital-adapted transmission was further corroborated by a recent large study on S. epidermidis PJI in Sweden [23]. The adaptation of ST2 and ST215 lineages to the hospital environment includes common genomic traits (IS256) and high prevalence of antimicrobial resistance genes even though some lineage-dependent differences are evident, i.e., the ST215 lineage lacks the intercellular adhesion gene A (icaA) gene [23, 27]. The primary source of HA-MDRSE lineages and the routes of transmission are uncertain. Recent data suggest that current perioperative PJI prevention regimens select MDRSE either from the patient’s normal flora or by facilitating acquisition from the hospital environment [23].
Polymicrobial infections, including those caused by S. epidermidis, were common among the PJIs investigated in this study, and consistent with previous data, Enterococcus faecalis was the most frequent companion microbe [29]. In most cases, both S. epidermidis and E. faecalis were detected in most tissue specimens from each patient, which reduced the chances of contamination; however, the possibility cannot be completely excluded.
The results presented here have practical and clinical implications. The within-patient diversity of S. epidermidis infections suggests that the clinical microbiology assessment of a PJI requires re-evaluation [30]. We believe characterising more than two isolates phenotypically and genotypically will improve assessment regardless of whether the PJI microbiological diagnostic criteria are met. In-depth analysis of more than two isolates will also provide additional information for selecting the appropriate targeted antibiotic therapy and help distinguish between a relapse and reinfection. The present clinical microbiology method for genetic heterogeneity assessment is laborious and expensive; however, advances reported in recent studies may change that in the near future. For example, new culture-independent methods that can be applied in clinical laboratories can facilitate the rapid assessment of clonality and population structure of S. epidermidis communities in PJI [31]. Another suitable approach is the culturing of several specimens followed by sequencing of multiple microbial isolates during routine PJI microbial diagnostics. Given the high cost of PJI treatment, it is practical to implement routine PJI diagnostics using small-scale rapid sequencing technologies with a turn-around time, including bioinformatics, of 1–2 days [32].
There were a few limitations to this study. First, the study had a retrospective cohort design. However, this may not affect the investigation of S. epidermidis populations causing PJIs, as it was shown that the S. epidermidis population structure in central Sweden has remained fairly stable over the last 10 years [23]. Second, the collection of more isolates per patient would strengthen our findings. Multiple S. epidermidis isolates for WGS analysis could only be collected from a few patients with PJI. That said, the microbiological findings of heterogeneity indicate that the present-day criteria for PJI diagnosis is sub-optimal. Third, and most importantly, some of the isolates detected and characterised were potential contaminants and were not truly invasive; however, all consecutive patients with PJI who met the IDSA criteria were included. Further, we used fresh sets of skin incision and subcutaneous incision instruments and a new set of sterile instruments for each tissue specimen to reduce the risk of contamination.
In conclusion, the within-patient genetic diversity in S. epidermidis isolates was substantial, with variation in both antibiotic susceptibility and antibiotic resistance genes. The findings highlight the complexity and ambiguity in the phenotypical assessment of CoNS isolates from periprosthetic tissue cultures as diagnostic criteria for PJI. Larger systematic studies are needed to determine the implications of these findings for microbiological diagnosis and the clinical significance of these results for therapeutic outcomes.
Data availability
The whole-genome sequence data generated in this study have been submitted to the European Nucleotide Archive under BioProject ID PRJEB44086.
Change history
28 February 2022
The original version of this paper was updated to add the missing compact agreement Open Access funding note.
References
Learmonth ID, Young C, Rorabeck C (2007) The operation of the century: total hip replacement. Lancet 370(9597):1508–1519. https://doi.org/10.1016/S0140-6736(07)60457-7
Zinkernagel AS, Speck RF, Ruef C, Zingg W, Berger-Bachi B, Springer B (2005) Rapidly destructive Staphylococcus epidermidis endocarditis. Infection 33(3):148–150. https://doi.org/10.1007/s15010-005-4111-7
Shahi A, Tan TL, Chen AF, Maltenfort MG, Parvizi J (2017) In-hospital mortality in patients with periprosthetic joint infection. J Arthroplast 32(3):948-952 e941. https://doi.org/10.1016/j.arth.2016.09.027
Del Pozo JL, Patel R (2009) Clinical practice. Infection associated with prosthetic joints. N Engl J Med 361(8):787–794. https://doi.org/10.1056/NEJMcp0905029
Tande AJ, Patel R (2014) Prosthetic joint infection. Clin Microbiol Rev 27(2):302–345. https://doi.org/10.1128/CMR.00111-13
Osmon DR, Berbari EF, Berendt AR, Lew D, Zimmerli W, Steckelberg JM, Rao N, Hanssen A, Wilson WR, Infectious Diseases Society of America (2013) Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis 56(1):e1–e25. https://doi.org/10.1093/cid/cis803
Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, Garvin KL, Mont MA, Wongworawat MD, Zalavras CG (2011) New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res 469(11):2992–2994. https://doi.org/10.1007/s11999-011-2102-9
Amanatullah D, Dennis D, Oltra EG, Marcelino Gomes LS, Goodman SB, Hamlin B, Hansen E, Hashemi-Nejad A, Holst DC, Komnos G, Koutalos A, Malizos K, Martinez Pastor JC, McPherson E, Meermans G, Mooney JA, Mortazavi J, Parsa A, Pecora JR, Pereira GA, Martos MS, Shohat N, Shope AJ, Zullo SS (2019) Hip and knee section, diagnosis, definitions: Proceedings of International Consensus on Orthopedic Infections. J Arthroplast 34 (2S):S329-S337. https://doi.org/10.1016/j.arth.2018.09.044
Harris LG, Murray S, Pascoe B, Bray J, Meric G, Magerios L, Wilkinson TS, Jeeves R, Rohde H, Schwarz S, de Lencastre H, Miragaia M, Rolo J, Bowden R, Jolley KA, Maiden MC, Mack D, Sheppard SK (2016) Biofilm morphotypes and population structure among Staphylococcus epidermidis from commensal and clinical samples. PLoS ONE 11(3):e0151240. https://doi.org/10.1371/journal.pone.0151240
Bogut A, Niedzwiadek J, Koziol-Montewka M, Strzelec-Nowak D, Blacha J, Mazurkiewicz T, Marczynski W, Plewik D (2014) Characterization of Staphylococcus epidermidis and Staphyloccocus warneri small-colony variants associated with prosthetic-joint infections. J Med Microbiol 63(Pt 2):176–185. https://doi.org/10.1099/jmm.0.066068-0
Maduka-Ezeh AN, Greenwood-Quaintance KE, Karau MJ, Berbari EF, Osmon DR, Hanssen AD, Steckelberg JM, Patel R (2012) Antimicrobial susceptibility and biofilm formation of Staphylococcus epidermidis small colony variants associated with prosthetic joint infection. Diagn Microbiol Infect Dis 74(3):224–229. https://doi.org/10.1016/j.diagmicrobio.2012.06.029
Tevell S, Baig S, Nilsdotter-Augustinsson A, Stegger M, Soderquist B (2019) Same organism, different phenotype—are phenotypic criteria adequate in coagulase-negative staphylococcal orthopaedic implant-associated infections? J Bone Jt Infect 4(1):16–19. https://doi.org/10.7150/jbji.30256
Oh J, Byrd AL, Deming C, Conlan S, Program NCS, Kong HH, Segre JA (2014) Biogeography and individuality shape function in the human skin metagenome. Nature 514(7520):59–64. https://doi.org/10.1038/nature13786
Hu L, Umeda A, Amako K (1995) Typing of Staphylococcus epidermidis colonizing in human nares by pulsed-field gel electrophoresis. Microbiol Immunol 39(5):315–319. https://doi.org/10.1111/j.1348-0421.1995.tb02207.x
Harris LG, El-Bouri K, Johnston S, Rees E, Frommelt L, Siemssen N, Christner M, Davies AP, Rohde H, Mack D (2010) Rapid identification of staphylococci from prosthetic joint infections using MALDI-TOF mass-spectrometry. Int J Artif Organs 33(9):568–574. https://doi.org/10.1177/039139881003300902
Widerstrom M, Monsen T, Karlsson C, Edebro H, Johansson A, Wistrom J (2009) Clonality among multidrug-resistant hospital-associated Staphylococcus epidermidis in northern Europe. Scand J Infect Dis 41(9):642–649. https://doi.org/10.1080/00365540903146987
Thomas JC, Vargas MR, Miragaia M, Peacock SJ, Archer GL, Enright MC (2007) Improved multilocus sequence typing scheme for Staphylococcus epidermidis. J Clin Microbiol 45(2):616–619
Bankevich A, Nurk S, Antipov D, Gurevich AA, Dvorkin M, Kulikov AS, Lesin VM, Nikolenko SI, Pham S, Prjibelski AD, Pyshkin AV, Sirotkin AV, Vyahhi N, Tesler G, Alekseyev MA, Pevzner PA (2012) SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J Comput Biol 19(5):455–477. https://doi.org/10.1089/cmb.2012.0021
Sahl JW, Lemmer D, Travis J, Schupp JM, Gillece JD, Aziz M, Driebe EM, Drees KP, Hicks ND, Williamson CHD, Hepp CM, Smith DE, Roe C, Engelthaler DM, Wagner DM, Keim P (2016) NASP: an accurate, rapid method for the identification of SNPs in WGS datasets that supports flexible input and output formats. Microb Genom 2(8):e000074. https://doi.org/10.1099/mgen.0.000074
McKenna A, Hanna M, Banks E, Sivachenko A, Cibulskis K, Kernytsky A, Garimella K, Altshuler D, Gabriel S, Daly M, DePristo MA (2010) The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res 20(9):1297–1303. https://doi.org/10.1101/gr.107524.110
Guindon S, Dufayard JF, Lefort V, Anisimova M, Hordijk W, Gascuel O (2010) New algorithms and methods to estimate maximum-likelihood phylogenies: assessing the performance of PhyML 3.0. Syst Biol 59(3):307–321. https://doi.org/10.1093/sysbio/syq010
Lefort V, Longueville JE, Gascuel O (2017) SMS: smart model selection in PhyML. Mol Biol Evol 34(9):2422–2424. https://doi.org/10.1093/molbev/msx149
Mansson E, Bech Johannesen T, Nilsdotter-Augustinsson A, Soderquist B, Stegger M (2021) Comparative genomics of Staphylococcus epidermidis from prosthetic-joint infections and nares highlights genetic traits associated with antimicrobial resistance, not virulence. Microb Genom. https://doi.org/10.1099/mgen.0.000504
Harris LG, Bodger O, Post V, Mack D, Morgenstern M, Rohde H, Moriarty TF, Wilkinson TS (2020) Temporal changes in patient-matched Staphylococcus epidermidis isolates from infections: towards defining a ‘true’ persistent infection. Microorganisms 8(10):1508. https://doi.org/10.3390/microorganisms8101508
Widerstrom M, McCullough CA, Coombs GW, Monsen T, Christiansen KJ (2012) A multidrug-resistant Staphylococcus epidermidis clone (ST2) is an ongoing cause of hospital-acquired infection in a Western Australian hospital. J Clin Microbiol 50(6):2147–2151. https://doi.org/10.1128/JCM.06456-11
Wildeman P, Tevell S, Eriksson C, Lagos AC, Soderquist B, Stenmark B (2020) Genomic characterization and outcome of prosthetic joint infections caused by Staphylococcus aureus. Sci Rep 10(1):5938. https://doi.org/10.1038/s41598-020-62751-z
Lee JYH, Monk IR, Goncalves da Silva A, Seemann T, Chua KYL, Kearns A, Hill R, Woodford N, Bartels MD, Strommenger B, Laurent F, Dodemont M, Deplano A, Patel R, Larsen AR, Korman TM, Stinear TP, Howden BP (2018) Global spread of three multidrug-resistant lineages of Staphylococcus epidermidis. Nat Microbiol 3(10):1175–1185. https://doi.org/10.1038/s41564-018-0230-7
Meric G, Mageiros L, Pensar J, Laabei M, Yahara K, Pascoe B, Kittiwan N, Tadee P, Post V, Lamble S, Bowden R, Bray JE, Morgenstern M, Jolley KA, Maiden MCJ, Feil EJ, Didelot X, Miragaia M, de Lencastre H, Moriarty TF, Rohde H, Massey R, Mack D, Corander J, Sheppard SK (2018) Disease-associated genotypes of the commensal skin bacterium Staphylococcus epidermidis. Nat Commun 9(1):5034. https://doi.org/10.1038/s41467-018-07368-7
Flurin L, Greenwood-Quaintance KE, Patel R (2019) Microbiology of polymicrobial prosthetic joint infection. Diagn Microbiol Infect Dis 94(3):255–259. https://doi.org/10.1016/j.diagmicrobio.2019.01.006
Proctor RA (2000) Editorial response: coagulase-negative staphylococcal infections: A diagnostic and therapeutic challenge. Clin Infect Dis 31(1):31–33. https://doi.org/10.1086/313894
Rendboe AK, Johannesen TB, Ingham AC, Mansson E, Iversen S, Baig S, Edslev S, Jensen JS, Soderquist B, Andersen PS, Stegger M (2020) The Epidome—a species-specific approach to assess the population structure and heterogeneity of Staphylococcus epidermidis colonization and infection. BMC Microbiol 20(1):362. https://doi.org/10.1186/s12866-020-02041-w
Taxt AM, Avershina E, Frye SA, Naseer U, Ahmad R (2020) Rapid identification of pathogens, antibiotic resistance genes and plasmids in blood cultures by nanopore sequencing. Sci Rep 10(1):7622. https://doi.org/10.1038/s41598-020-64616-x
Acknowledgements
Preliminary data from this study was presented at ISSSI 2014.
Funding
Open access funding provided by Umea University. The project was supported by the following: the Swedish Society of Medicine SLS-24993, SLS-413681; the Research and Development Unit, Jämtland County Council, Sweden; and through a regional agreement between Umeå University and Region Västerbotten. The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Author information
Authors and Affiliations
Contributions
TM, MW, AJ, ARL, and MS conceive and designed the study, analysed and interpreted data, and drafted the manuscript. HE and BKG carried out the phenotypic and genotypic analyses. LW and MW collected the clinical data. All authors read, revised, and approved the manuscript before submission.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Research Ethics Committee (No 2012–477-31 M) of the Faculty of Medicine, Umeå University, Sweden.
Consent to participate
Oral and written informed consent was obtained from the participants.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Widerström, M., Stegger, M., Johansson, A. et al. Heterogeneity of Staphylococcus epidermidis in prosthetic joint infections: time to reevaluate microbiological criteria?. Eur J Clin Microbiol Infect Dis 41, 87–97 (2022). https://doi.org/10.1007/s10096-021-04352-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-021-04352-w