Abstract
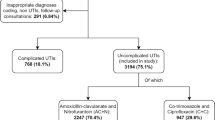
Targeted antibiotic prophylaxis (TAP) is required for patients with positive urine culture before urological surgery. Our aim was to determine the efficacy of TAP. This was a prospective single-center study performed in a urology department. All patients who underwent a programmed surgery were included. Urine culture was obtained before surgery requiring a prophylaxis: in the case of sterile urines, antibiotics were used in accordance with national recommendations; for positive urine culture, a TAP was used in accordance with susceptibility testing. The drugs were administered for 2 days before surgery until withdrawal of bladder catheter. The occurrence of healthcare-associated infections was registered until day 30 after surgery. Two hundred three patients were included for 8 non-consecutive weeks in 2020, among whom fifteen were lost of sight before day 30. Among the remaining 188 patients, most frequent surgeries were 75 prostatic diseases (40%), 50 endo-ureteral surgeries for JJ stent insertion (27%), and 23 bladder cancers (12%). One hundred forty-eight (79%) patients required a urine culture before procedure; 142/148 (96%) urine cultures were performed, leading to 74 TAP. The main isolated bacteria were 48 Enterobacteriaceae and 8 Enterococcus spp. TAP was cotrimoxazole (n = 30), aminoglycosides (n = 11), amoxicillin (n = 9), fluoroquinolones (n = 7), and others (n = 17). The rate of healthcare-associated infections was 14.8% (11/74), including six microbiologically documented antibiotic failures. The rate of healthcare-associated infection after urological surgery using TAP was high, implying to discuss the choice and the dosage of the antibiotic molecules.

Similar content being viewed by others
Data availability
The data used during the current study is available from the corresponding author on reasonable request.
References
Wolf JS, Bennett CJ, Dmochowski RR, Hollenbeck BK, Pearle MS, Schaeffer AJ (2008) Best practice policy statement on urologic surgery antimicrobial prophylaxis. J Urol 179:1379–1390
Khaw C, Oberle AD, Lund BC et al (2018) Assessment of guideline discordance with antimicrobial prophylaxis best practices for common urologic procedures. JAMA Netw Open 1(8):e186248. https://doi.org/10.1001/jamanetworkopen.2018.6248
Medina-Polo J, Sopeña-Sutil R, Benítez-Sala R et al (2017) Prospective study analyzing risk factors and characteristics of healthcare-associated infections in a urology ward. Investig Clin Urol 58:61–69
Enquête nationale de prévalence des infections nosocomiales et des traitements anti-infectieux en établissements de santé, mai-juin 2017. https://www.enquete-nationale-de-prevalence-des-infections-nosocomiales-et-des-traitements-anti-infectieux-en-etablissements-de-sante-mai-juin-2017
Souhail B, Charlot P, Déroudilhes G, Coblentz Y, Pierquet G, Gimel P et al (2020) Urinary tract infection and antibiotic use around ureteral stent insertion for urolithiasis. Eur J Clin Microbial Infect Dis 39:2077–2083
Köves B, Cai T, Veeratterapillay R, Pickard R, Seisen T, Lam TB et al. Benefits and harms of treatment of asymptomatic bacteriuria: a systematic review and meta-analysis by the European Association of Urology. Eur Ass Urol. https://doi.org/10.1016/j.eururo.2017.07.014
Sabé N, Oriol I, Melilli E, Manonelles A, Bestard O, Polo C et al (2019) Antibiotic treatment versus no treatment for asymptomatic bacteriuria in kidney transplant recipients: a multicenter randomized trial. Open Forum Infect Dis 6:ofz243. https://doi.org/10.1093/ofid/ofz243
Nicolle LE, Gupta K, Bradley SF, Colgan R, DeMuri GP, Drekonja D et al (2019) Clinical practice guideline for the management of asymptomatic bacteriuria: 2019 Update by the Infectious Diseases Society of America. Clin Infect Dis 68:1611–1615
Kandil H, Cramp E, Vaghela T (2016) Trends in antibiotic resistance in urologic practice. Eur Urol Focus. https://doi.org/10.1016/j.euf.2016.09.0068
Taylor AK, Zembower TR, Nadler RB et al (2012) Targeted antimicrobial prophylaxis using rectal swab cultures in men undergoing transrectal ultrasound guided prostate biopsy is associated with reduced incidence of postoperative infectious complications and cost of care. J Urol 187:1275–1279
Boeri L, Fontana M, Gallioli A, Zanetti SP, Catellani M, Longo F et al (2017) Rectal culture-guided targeted antimicrobial prophylaxis reduces the incidence of post-operative infectious complications in men at high risk for infections submitted to transrectal ultrasound prostate biopsy – results of a cross-sectional study. PLoS ONE 12:e0170319. https://doi.org/10.1371/journal.pone.0170319
Concepcion RS, Schaeffer EM, Shore ND, Kapoor DA, Scott JA, Kirsh GM (2019) The effect of local antibiogram–based augmented antibiotic prophylaxis on infection-related complications following prostate biopsy. Rev Urol 21:93–101
Peron EP, Hirsch AA, Jury LA, Jump RL, Donskey CJ (2013) Another setting for stewardship: high rate of unnecessary antimicrobial use in a Veterans Affairs long term care facility. J Am Geriat Soc 61:289–290
Hamasuna R, Betsunoh H, Sueyoshi T, Yakushiji K, Tsukino H, Nagano M et al (2004) Bacteria of preoperative urinary tract infections contaminate the surgical fields and develop surgical site infections in urological operations. Inter J Urol 11:941–947
Chen M, Buurma V, Shah M, Fahim G (2019) Evaluation of studies on extended versus standard infusion of beta-lactam antibiotics. Am J Health Syst Pharm 76:1383–1394. https://doi.org/10.1093/ajhp/zxz154
Lacy MK, Nicolau DP, Nightingale CH, Quintiliani R (1998) The pharmacodynamics of aminoglycosides. Clin Infect Dis 27:23–27
Author information
Authors and Affiliations
Contributions
All authors contributed significantly to the study, and all have read and consent to the article.
Corresponding author
Ethics declarations
Ethics approval
The antibiotic audit was sponsored by the French National Health Agency.
Consent to participate
The patients or their relatives provided written consent for computerization of their personal data for hospitalization purposes and clinical research. Patient privacy was protected as no personal data were extracted or copied from the computerized chart.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Curlier, E., Sadreux, Y., Markowicz, S. et al. Therapeutic failures of targeted antibiotic prophylaxis in urology. Eur J Clin Microbiol Infect Dis 41, 299–304 (2022). https://doi.org/10.1007/s10096-021-04329-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-021-04329-9