Abstract
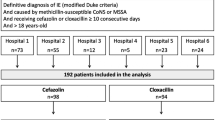
Whether cefazolin is as effective and safer than antistaphylococcal penicillins (ASPs) for the treatment of methicillin-susceptible Staphylococcus aureus (MSSA) infective endocarditis (IE) is still debated in the absence of a randomized controlled trial. In this quasi-experimental study, we aimed to assess the effectiveness and safety of these two treatments in MSSA-IE, using the ASPs nationwide shortage in April 2016 as a unique opportunity to overcome the indication bias associated with observational studies. In this single-centre study, we compared patients with Duke-Li definite MSSA-IE treated with ASPs from January 2015 to March 2016 versus those treated with cefazolin from April 2016 to December 2018, when ASPs were not available. Effectiveness outcome was 90-day all-cause mortality. Safety outcomes included significant decrease in GFR and significant increase in serum liver enzymes. Logrank test was used to compare survival rates. Of 73 patients with MSSA-IE, 35 and 38 were treated with ASPs and cefazolin, respectively. Baseline patients’ characteristics (demography, native or prosthetic valve IE, clinical characteristics, cardiac and septic complications) were similar between groups. Ninety-day all-cause mortality was 28.6% and 21.1%, in patients treated with ASPs and cefazolin, respectively (logrank p = 0.5727). There was no difference between groups for incident renal or liver toxicity events: acute kidney injury 45.7% vs. 44.7% (p = 0.933), increased ALT 5.7% vs. 13.2% (p = 0.432), bilirubin increase 5.7% vs. 10.5% (p = 0.676), in ASPs vs. cefazolin groups, respectively. In this quasi-experimental, effectiveness and safety did not statistically differ between ASPs and cefazolin for MSSA-IE treatment.


Similar content being viewed by others
Data and materials availability
The datasets generated during and/or analysed during the current study are not publicly available due to restrictions by the French law, but are available from the last author on reasonable request at the following email address: n.agrinier@chru-nancy.fr.
Code availability
Not applicable.
References
Habib G, Erba PA, Iung B, Donal E, Cosyns B, Laroche C et al (2019) Clinical presentation, aetiology and outcome of infective endocarditis. Results of the ESC-EORP EURO-ENDO (European infective endocarditis) registry: a prospective cohort study. Eur Heart J 40:3222–3232. https://doi.org/10.1093/eurheartj/ehz620
Selton-Suty C, Célard M, Le Moing V, Doco-Lecompte T, Chirouze C, Iung B et al (2012) Preeminence of Staphylococcus aureus in infective endocarditis: a 1-year population-based survey. Clin Infect Dis 1(54):1230–1239. https://doi.org/10.1093/cid/cis199
Olmos C, Vilacosta I, Fernández-Pérez C, Bernal JL, Ferrera C, García-Arribas D et al (2017) The evolving nature of infective endocarditis in Spain. J Am Coll Cardiol 70:2795–2804. https://doi.org/10.1016/j.jacc.2017.10.005
Cahill TJ, Prendergast BD (2016) Infective endocarditis. Lancet 387:882–893. https://doi.org/10.1016/S0140-6736(15)00067-7
Chu VH, Cabell CH, Benjamin DK, Kuniholm EF, Fowler VG, Engemann J et al (2004) Early predictors of in-hospital death in infective endocarditis. Circulation 13(109):1745–1749. https://doi.org/10.1161/01.CIR.0000124719.61827.7F
Hill EE, Herijgers P, Claus P, Vanderschueren S, Peetermans WE, Herregods M-C (2008) Clinical and echocardiographic risk factors for embolism and mortality in infective endocarditis. Eur J Clin Microbiol Infect Dis 27:1159–1164. https://doi.org/10.1007/s10096-008-0572-9
Asgeirsson H, Thalme A, Weiland O (2018) Staphylococcus aureus bacteraemia and endocarditis – epidemiology and outcome: a review. Infect Dis 4(50):175–192. https://doi.org/10.1080/23744235.2017.1392039
Le Moing V, Alla F, Doco-Lecompte T, Delahaye F, Piroth L, Chirouze C et al (2015) Staphylococcus aureus bloodstream infection and endocarditis - a prospective cohort study. PLoS ONE 28(10):e0127385. https://doi.org/10.1371/journal.pone.0127385
Hoen B, Duval X (2013) Infective endocarditis. N Engl J Med 11(368):1425–1433. https://doi.org/10.1056/NEJMcp1206782
Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta J-P, Del Zotti F et al (2015) 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC) Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J 21(36):3075–3128. https://doi.org/10.1093/eurheartj/ehv319
Baddour LM, Wilson WR, Bayer AS, Fowler VG, Tleyjeh IM, Rybak MJ et al (2015) Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: A Scientific Statement for Healthcare Professionals From the American Heart Association. Circulation 13(132):1435–1486. https://doi.org/10.1161/CIR.0000000000000296
SPILF & GPIP (2016) Propositions d’alternatives à l’oxacilline ou la cloxacilline par voie IV chez l’adulte et l’enfant en contexte de rupture de stock [Internet]. 22. https://ansm.sante.fr/var/ansm_site/storage/original/application/5974b225f773ec8cdcae133f286012bc.pdf. Accessed April 2020
Quintiliani R (1978) Drugs five years later: cefazolin. Ann Intern Med 1(89):650. https://doi.org/10.7326/0003-4819-89-5-650
Madhavan T, Quinn EL, Freimer E, Fisher EJ, Cox F, Burch K et al (1973) Clinical studies of cefazolin and comparison with other cephalosporins. Antimicrob Agents Chemother 1(4):525–531. https://doi.org/10.1128/AAC.4.5.525
Nannini EC, Singh KV, Arias CA, Murray BE (2013) In Vivo effects of cefazolin, daptomycin, and nafcillin in experimental endocarditis with a methicillin-susceptible Staphylococcus aureus strain showing an inoculum effect against cefazolin. Antimicrob Agents Chemother 57:4276–4281. https://doi.org/10.1128/AAC.00856-13
Sande MA, Johnson ML (1975) Antimicrobial therapy of experimental endocarditis caused by Staphylococcus aureus. J Infect Dis 1(131):367–375. https://doi.org/10.1093/infdis/131.4.367
Fernandez-Guerrero ML, de Gorgolas M (2005) Cefazolin therapy for Staphylococcus aureus bacteremia. Clin Infect Dis 1(41):127–127. https://doi.org/10.1086/430833
Quinn EL, Pohlod D, Madhavan T, Burch K, Fisher E, Cox F (1973) Clinical experiences with cefazolin and other cephalosporins in bacterial endocarditis. J Infect Dis 1(128):S386–S391. https://doi.org/10.1093/infdis/128.Supplement_2.S386
Goldman PL, Petersdorf RG (1980) Importance of -lactamase inactivation in treatment of experimental endocarditis caused by Staphylococcus aureus. J Infect Dis 1(141):331–337. https://doi.org/10.1093/infdis/141.3.331
Nannini EC, Stryjewski ME, Singh KV, Bourgogne A, Rude TH, Corey GR et al (2009) Inoculum effect with cefazolin among clinical isolates of methicillin-susceptible Staphylococcus aureus: frequency and possible cause of cefazolin treatment failure. Antimicrob Agents Chemother 1(53):3437–3441. https://doi.org/10.1128/AAC.00317-09
Steckelberg JM, Rouse MS, Tallan BM, Osmon DR, Henry NK, Wilson WR (1993) Relative efficacies of broad-spectrum cephalosporins for treatment of methicillin-susceptible Staphylococcus aureus experimental infective endocarditis. Antimicrob Agents Chemother 1(37):554–558. https://doi.org/10.1128/AAC.37.3.554
Carrizosa J, Santoro J, Kaye D (1978) Treatment of experimental Staphylococcus aureus endocarditis: comparison of cephalothin, cefazolin, and methicillin. Antimicrob Agents Chemother 1(13):74–77. https://doi.org/10.1128/AAC.13.1.74
Bryant RE, Alford RH (1977) Unsuccessful treatment of staphylococcal endocarditis with cefazolin. JAMA 7(237):569–570
Bai AD, Showler A, Burry L, Steinberg M, Ricciuto DR, Fernandes T et al (2015) Comparative effectiveness of cefazolin versus cloxacillin as definitive antibiotic therapy for MSSA bacteraemia: results from a large multicentre cohort study. J Antimicrob Chemother 70:1539–1546. https://doi.org/10.1093/jac/dku560
Lee S, Choe PG, Song K-H, Park S-W, Kim HB, Kim NJ et al (2011) Is cefazolin inferior to nafcillin for treatment of methicillin-susceptible Staphylococcus aureus bacteremia? Antimicrob Agents Chemother 55:5122–5126. https://doi.org/10.1128/AAC.00485-11
Li J, Echevarria KL, Traugott KA (2017) β-Lactam Therapy for methicillin-susceptible Staphylococcus aureus bacteremia: a comparative review of cefazolin versus antistaphylococcal penicillins. Pharmacother J Hum Pharmacol Drug Ther 37:346–360. https://doi.org/10.1002/phar.1892
Loubet P, Burdet C, Vindrios W, Grall N, Wolff M, Yazdanpanah Y et al (2018) Cefazolin versus anti-staphylococcal penicillins for treatment of methicillin-susceptible Staphylococcus aureus bacteraemia: a narrative review. Clin Microbiol Infect 24:125–132. https://doi.org/10.1016/j.cmi.2017.07.003
Paul M, Zemer-Wassercug N, Talker O, Lishtzinsky Y, Lev B, Samra Z et al (2011) Are all beta-lactams similarly effective in the treatment of methicillin-sensitive Staphylococcus aureus bacteraemia? Clin Microbiol Infect 17:1581–1586. https://doi.org/10.1111/j.1469-0691.2010.03425.x
Rao SN, Rhodes NJ, Lee BJ, Scheetz MH, Hanson AP, Segreti J et al (2015) Treatment outcomes with cefazolin versus oxacillin for deep-seated methicillin-susceptible Staphylococcus aureus bloodstream infections. Antimicrob Agents Chemother 59:5232–5238. https://doi.org/10.1128/AAC.04677-14
Monogue ML, Ortwine JK, Wei W, Eljaaly K, Bhavan KP (2018) Nafcillin versus cefazolin for the treatment of methicillin-susceptible Staphylococcus aureus bacteremia. J Infect Public Health 11:727–731. https://doi.org/10.1016/j.jiph.2018.02.004
Lecomte R, Bourreau A, Deschanvres C, Issa N, Le Turnier P, Gaborit B, et al (2020) Comparative outcomes of cefazolin versus anti-staphylococcal penicillins in methicillin-susceptible Staphylococcus aureus infective endocarditis: a post-hoc analysis of a prospective multicentre French cohort study. Clin Microbiol Infect S1198743X20305644. https://doi.org/10.1016/j.cmi.2020.08.044
U.S. National Institutes of Health (NIH) Department of Health And Human Services (2017) Common Terminology Criteria for Adverse Events (CTCAE) Version 5.0 [Internet]. 27 [cited 2021 24]. https://ctep.cancer.gov/protocoldevelopment/electronic_applications/ctc.htm#ctc_50. Accessed April 2020
KDIGO AKI Work Group (2012) KDIGO clinical practice guidelines for acute kidney injury. Kidney Int Suppl 2:2. https://doi.org/10.1038/kisup.2012.2
Weis S, Kesselmeier M, Davis JS, Morris AM, Lee S, Scherag A et al (2019) Cefazolin versus anti-staphylococcal penicillins for the treatment of patients with Staphylococcus aureus bacteraemia. Clin Microbiol Infect 25:818–827. https://doi.org/10.1016/j.cmi.2019.03.010
Bidell MR, Patel N, O’Donnell JN (2018) Optimal treatment of MSSA bacteraemias: a meta-analysis of cefazolin versus antistaphylococcal penicillins. J Antimicrob Chemother 1(73):2643–2651. https://doi.org/10.1093/jac/dky259
Rindone JP, Mellen CK (2018) Meta-analysis of trials comparing cefazolin to antistaphylococcal penicillins in the treatment of methicillin-sensitive Staphylococcus aureus bacteraemia: meta-analysis: cefazolin vs. antistaphylococcal penicillin. Br J Clin Pharmacol 84:1258–1266. https://doi.org/10.1111/bcp.13554
Shi C, Xiao Y, Zhang Q, Li Q, Wang F, Wu J, et al (2018) Efficacy and safety of cefazolin versus antistaphylococcal penicillins for the treatment of methicillin-susceptible Staphylococcus aureus bacteremia: a systematic review and meta-analysis. BMC Infect Dis [Internet] [cited 2019 15] 18. https://doi.org/10.1186/s12879-018-3418-9
Lee S, Song K-H, Jung S-I, Park WB, Lee SH, Kim Y-S et al (2018) Comparative outcomes of cefazolin versus nafcillin for methicillin-susceptible Staphylococcus aureus bacteraemia: a prospective multicentre cohort study in Korea. Clin Microbiol Infect 24:152–158. https://doi.org/10.1016/j.cmi.2017.07.001
McDanel JS, Roghmann M-C, Perencevich EN, Ohl ME, Goto M, Livorsi DJ et al (2017) Comparative effectiveness of cefazolin versus nafcillin or oxacillin for treatment of methicillin-susceptible Staphylococcus aureus infections complicated by bacteremia: a nationwide cohort study. Clin Infect Dis 1(65):100–106. https://doi.org/10.1093/cid/cix287
Twilla JD, Algrim A, Adams EH, Samarin M, Cummings C, Finch CK (2020) Comparison of nafcillin and cefazolin for the treatment of methicillin-susceptible Staphylococcus aureus bacteremia. Am J Med Sci 360:35–41. https://doi.org/10.1016/j.amjms.2020.04.006
Pollett S, Baxi SM, Rutherford GW, Doernberg SB, Bacchetti P, Chambers HF (2016) Cefazolin versus nafcillin for methicillin-sensitive Staphylococcus aureus bloodstream infection in a California Tertiary Medical Center. Antimicrob Agents Chemother 60:4684–4689. https://doi.org/10.1128/AAC.00243-16
Davis J, Turnidge J, Tong S (2018) A large retrospective cohort study of cefazolin compared with flucloxacillin for methicillin-susceptible Staphylococcus aureus bacteraemia. Int J Antimicrob Agents 52:297–300. https://doi.org/10.1016/j.ijantimicag.2018.02.013
Renaud CJ, Lin X, Subramanian S, Fisher DA (2011) High-dose cefazolin on consecutive hemodialysis in anuric patients with Staphylococcal bacteremia: High-dose cefazolin on consecutive HD in anuric patients. Hemodial Int 15:63–68. https://doi.org/10.1111/j.1542-4758.2010.00507.x
Li J, Echevarria KL, Hughes DW, Cadena JA, Bowling JE, Lewis JS (2014) Comparison of cefazolin versus oxacillin for treatment of complicated bacteremia caused by methicillin-susceptible Staphylococcus aureus. Antimicrob Agents Chemother 58:5117–5124. https://doi.org/10.1128/AAC.02800-14
Youngster I, Shenoy ES, Hooper DC, Nelson SB (2014) Comparative evaluation of the tolerability of cefazolin and nafcillin for treatment of methicillin-susceptible Staphylococcus aureus infections in the outpatient setting. Clin Infect Dis 1(59):369–375. https://doi.org/10.1093/cid/ciu301
Burrelli CC, Broadbent EK, Margulis A, Snyder GM, Gold HS, McCoy C et al (2018) Does the beta-lactam matter? Nafcillin versus cefazolin for methicillin-susceptible Staphylococcus aureus bloodstream infections. Chemotherapy 63:345–351. https://doi.org/10.1159/000499033
Flynt LK, Kenney RM, Zervos MJ, Davis SL (2017) The safety and economic impact of cefazolin versus nafcillin for the treatment of methicillin-susceptible Staphylococcus aureus bloodstream infections. Infect Dis Ther 6:225–231. https://doi.org/10.1007/s40121-017-0148-z
Miller MA, Fish DN, Barber GR, Barron MA, Goolsby TA, Moine P et al (2020) A comparison of safety and outcomes with cefazolin versus nafcillin for methicillin-susceptible Staphylococcus aureus bloodstream infections. J Microbiol Immunol Infect 53:321–327. https://doi.org/10.1016/j.jmii.2018.07.006
Chan L, Chan-Tompkins NH, Como J, Guarascio AJ (2020) Retrospective analysis of adverse drug events between nafcillin versus cefazolin for treatment of methicillin-susceptible Staphylococcus aureus infections. Ann Pharmacother 54:662–668. https://doi.org/10.1177/1060028019897267
Acknowledgements
We would like to acknowledge the entire ObservatoireEI team.
Author information
Authors and Affiliations
Consortia
Contributions
Personal contribution for the conception and design of the study (BL, BH, FG, NAg), acquisition of data (BL, BH, FG, NA, CA, EJ, SH, LF, CSS), analysis and interpretation of data (BL, BH, WNS, NAg), drafting the article or revising it critically for important intellectual content (BL, BH, WNS, NAg) and final approval of the version to be submitted (BL, BH, FG, NA, WNS, NA, CA, EJ, SH, LF, CSS, NAg).
Corresponding author
Ethics declarations
Ethics approval
This study complies with the principles outlined in the Declaration of Helsinki. ObservatoireEI (NCT03272724) was authorized by the Commission Nationale de l’Informatique et des Libertés (CNIL).
Consent to participate
Patients were informed of the study and individual consent was waived, in accordance with French legal standards.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lefèvre, B., Hoen, B., Goehringer, F. et al. Antistaphylococcal penicillins vs. cefazolin in the treatment of methicillin-susceptible Staphylococcus aureus infective endocarditis: a quasi-experimental monocentre study. Eur J Clin Microbiol Infect Dis 40, 2605–2616 (2021). https://doi.org/10.1007/s10096-021-04313-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-021-04313-3