Abstract
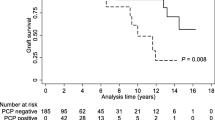
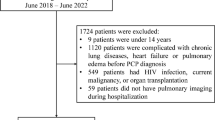
Pneumocystis jirovecii pneumonia (PCP) is a life-threatening opportunistic infection in idiopathic membranous nephropathy (IMN) patients, who are treated with immunosuppressive drugs. However, the risk factors of infection and their prognosis are rarely investigated. We aimed to characterize the clinical manifestations of PCP in patients with IMN, and to understand their risk factors, so that we can provide early warnings to patients with high risk and potential poor prognosis. We conducted a retrospective observational study of IMN patients in a referral center in China, from Jan 2012 to Dec 2018. Clinical and laboratory data were collected separately at the time of IMN and PCP diagnosis. Patients with PCP were matched to those without by gender and age at a ratio of 1:4. The risk factors and prognostic factors were determined by univariate and multivariate logistic regression analysis. A total of 879 patients with IMN were included, with a median follow-up of 267 (interquartile range (IQR) 64,842) days. In total, 26 (2.96%) of them were diagnosed with PCP. The infection rate increased to 3.87% among patients who received corticosteroids, and it further increased to 5.49% in those received over 0.5mg/kg prednisone. Univariate analysis indicated that initial usage of corticosteroids, use of cyclophosphamide, reduced estimated glomerular filtration rate (eGFR), and higher 24-h proteinuria were related to the PCP susceptibility. Multivariate analysis revealed that corticosteroid treatment and reduced eGFR increased the risk of the Pneumocystis jirovecii infection. The case fatality rate of the PCP patients was 23.08%, and increased to 75% among patients requiring invasive ventilation. Univariate analysis indicated that pulmonary insufficiency, invasive ventilation, decreased eGFR, and increased lactate dehydrogenase at presentation were linked to poor prognosis. PCP is not rare in patients with IMN, especially those on corticosteroids, and presented with decreased eGFR. Considering the high case fatality rate, further studies are in need for prevention and management of these patients.

Similar content being viewed by others
References
Yokoyama H, Taguchi T, Sugiyama H, Sato H (2012) Membranous nephropathy in Japan: analysis of the Japan Renal Biopsy Registry (J-RBR). Clin Exp Nephrol 16(4):557–563. https://doi.org/10.1007/s10157-012-0593-7
Zhu H et al (2018) The clinicopathological features of patients with membranous nephropathy. Int J Nephrol Renov Dis 11:33–40. https://doi.org/10.2147/IJNRD.S149029
Chen Y et al (2014) Immunosuppressive treatment for idiopathic membranous nephropathy in adults with nephrotic syndrome. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD004293.pub3
Tasaka S, Tokuda H (2012) Pneumocystis jirovecii pneumonia in non-HIV-infected patients in the era of novel immunosuppressive therapies. J Infect Chemother 18(6):793–806. https://doi.org/10.1007/s10156-012-0453-0
Roblot F et al (2002) Analysis of underlying diseases and prognosis factors associated with pneumocystis carinii pneumonia in immunocompromised HIV-negative patients. Eur J Clin Microbiol Infect Dis 21(7):523–531. https://doi.org/10.1007/s10096-002-0758-5
Mansharamani NG, Garland R, Delaney D, Koziel H (2000) Management and outcome patterns for adult Pneumocystis carinii pneumonia, 1985 to 1995. Chest 118(3):704–711. https://doi.org/10.1378/chest.118.3.704
Stern A, Green H, Paul M, Vidal L, Leibovici L (2014) Prophylaxis for Pneumocystis pneumonia (PCP) in non-HIV immunocompromised patients. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD005590.pub3
Eitner F et al (2011) Risk factors for Pneumocystis jiroveci pneumonia (PcP) in renal transplant recipients. Nephrol Dial Transplant 26(6):2013–2017. https://doi.org/10.1093/ndt/gfq689
Park JW, Curtis JR, Moon J, Song YW, Kim S, Lee EB (2018) Prophylactic effect of trimethoprim-sulfamethoxazole for pneumocystis pneumonia in patients with rheumatic diseases exposed to prolonged high-dose glucocorticoids. Ann Rheum Dis 77(5):644–649. https://doi.org/10.1136/annrheumdis-2017-211796
Mikaelsson L, Jacobsson G, Andersson R (2006) Pneumocystis pneumonia - a retrospective study 1991-2001 in Gothenburg, Sweden. J Inf Secur 53(4):260–265. https://doi.org/10.1016/j.jinf.2005.06.014
San-Andres F et al (2003) Incidence of acquired immunodeficiency syndrome–associated opportunistic diseases and the effect of treatment on a cohort of 1115 patients infected with human immunodeficiency virus, 1989–1997. Clin Infect Dis 36(9):1177–1185. https://doi.org/10.1086/374358
Pereira-Díaz E, Moreno-Verdejo F, de la Horra C, Guerrero JA, Calderón EJ, Medrano FJ (2019) Changing trends in the epidemiology and risk factors of Pneumocystis pneumonia in Spain. Front Public Health 7. https://doi.org/10.3389/fpubh.2019.00275
Gaborit BJ et al (2019) Outcome and prognostic factors of Pneumocystis jirovecii pneumonia in immunocompromised adults: a prospective observational study. Ann Intensive Care 9(1):1–10. https://doi.org/10.1186/s13613-019-0604-x
Sepkowitz KA (2002) Opportunistic infections in patients with and patients without acquired immunodeficiency syndrome. Clin Infect Dis 34(8):1098–1107. https://doi.org/10.1086/339548
Van Den Brand JAJG, Van Dijk PR, Hofstra JM, Wetzels JFM (2014) Long-term outcomes in idiopathic membranous nephropathy using a restrictive treatment strategy. J Am Soc Nephrol 25(1):150–158. https://doi.org/10.1681/ASN.2013020185
Chew L-C, Maceda-Galang LM, Tan YK, Chakraborty B, Thumboo J (2015) Pneumocystis jirovecii pneumonia in patients with autoimmune disease on high-dose glucocorticoid. JCR J Clin Rheumatol 21(2):72–75. https://doi.org/10.1097/RHU.0000000000000215
Ruggenenti P et al (2012) Rituximab in idiopathic membranous nephropathy. J Am Soc Nephrol 23(8):1416–1425. https://doi.org/10.1681/ASN.2012020181
van den Brand JAJG et al (2017) Safety of rituximab compared with steroids and cyclophosphamide for idiopathic membranous nephropathy. J Am Soc Nephrol 28(9):2729–2737. https://doi.org/10.1681/ASN.2016091022
Cattran DC, Pei Y, Greenwood CMT, Ponticelli C, Passerini P, Honkanen E (1997) Validation of a predictive model of idiopathic membranous nephropathy: its clinical and research implications. Kidney Int 51(3):901–907. https://doi.org/10.1038/ki.1997.127
Polanco N et al (2010) Spontaneous remission of nephrotic syndrome in idiopathic membranous nephropathy. J Am Soc Nephrol 21(4):697–704. https://doi.org/10.1681/ASN.2009080861
Mähr N et al (2005) Proteinuria and hemoglobin levels in patients with primary glomerular disease. Am J Kidney Dis 46(3):424–431. https://doi.org/10.1053/j.ajkd.2005.06.002
Vaziri ND (1993) Endocrinological consequences of the nephrotic syndrome. Am J Nephrol 13(5):360–364. https://doi.org/10.1159/000168650
Vaziri ND, Kaupke CJ, Barton CH, Gonzales E (1992) Plasma concentration and urinary excretion of erythropoietin in adult nephrotic syndrome. Am J Med 92(1):35–40. https://doi.org/10.1016/0002-9343(92)90012-Z
Liu Y, Zheng K, Liu Y, Zhu H (2020) Pneumocystis jirovecii pneumonia in patients with nephrotic syndrome: application of lymphocyte subset analysis in predicting clinical outcomes. Can J Infect Dis Med Microbiol 2020. https://doi.org/10.1155/2020/4631297
Ye W-L et al (2016) Underlying renal insufficiency: the pivotal risk factor for Pneumocystis jirovecii pneumonia in immunosuppressed patients with non-transplant glomerular disease. Int Urol Nephrol 48(11):1863–1871. https://doi.org/10.1007/s11255-016-1324-x
Fujikura Y, Manabe T, Kawana A, Kohno S (2017) Adjunctive corticosteroids for Pneumocystis jirovecii pneumonia in non-HIV-infected patients: a systematic review and meta-analysis of observational studies. Arch Bronconeumol (English Ed) 53(2):55–61. https://doi.org/10.1016/j.arbr.2016.08.002
Ding L, Huang H, Wang H, He H (2020) Adjunctive corticosteroids may be associated with better outcome for non-HIV Pneumocystis pneumonia with respiratory failure: a systemic review and meta-analysis of observational studies. Ann Intensive Care 10:1. https://doi.org/10.1186/s13613-020-00649-9
Vogel M et al (2011) Accuracy of serum LDH elevation for the diagnosis of Pneumocystis jiroveci pneumonia. Swiss Med Wkly. https://doi.org/10.4414/smw.2011.13184
Butt AA, Michaels S, Kissinger P (2002) The association of serum lactate dehydrogenase level with selected opportunistic infections and HIV progression. Int J Infect Dis 6(3):178–181. https://doi.org/10.1016/S1201-9712(02)90107-4
Salzer HJF et al (2018) Clinical, diagnostic, and treatment disparities between HIV-infected and non-HIV-infected immunocompromised patients with Pneumocystis jirovecii pneumonia. Respiration 96(1):52–65. https://doi.org/10.1159/000487713
Liu Y, Su L, Jiang S-J, Qu H (2017) Risk factors for mortality from pneumocystis carinii pneumonia (PCP) in non-HIV patients: a meta-analysis. Oncotarget 8(35):59729–59739. https://doi.org/10.18632/oncotarget.19927
Yale SH, Limper AH (1996) Pneumocystis carinii pneumonia in patients without acquired immunodeficiency syndrome: associated illnesses and prior corticosteroid therapy. Mayo Clin Proc 71(1):5–13. https://doi.org/10.4065/71.1.5
Fishman JA, Rubin RH (1998) Infection in organ-transplant recipients. N Engl J Med 338(24):1741–1751. https://doi.org/10.1056/NEJM199806113382407
Wang T et al (2019) Predicting risk of pulmonary infection in patients with primary membranous nephropathy on immunosuppressive therapy: The AIM-7C score. Nephrology 24(10):1009–1016. https://doi.org/10.1111/nep.13544
Green H, Paul M, Vidal L, Leibovici L (2007) Prophylaxis of Pneumocystis pneumonia in immunocompromised non-HIV-infected patients: systematic review and meta-analysis of randomized controlled trials. Mayo Clin Proc 82(9):1052–1059. https://doi.org/10.4065/82.9.1052
Blount RJ et al (2017) Effects of clinical and environmental factors on bronchoalveolar antibody responses to Pneumocystis jirovecii: a prospective cohort study of HIV+ patients. PLoS One 12(7):e0180212. https://doi.org/10.1371/journal.pone.0180212
Alvaro-Meca A, Palomares-Sancho I, Diaz A, Resino R, De Miguel AG, Resino S (2015) Pneumocystis pneumonia in HIV-positive patients in Spain: epidemiology and environmental risk factors. J Int AIDS Soc 18(1):19906. https://doi.org/10.7448/IAS.18.1.19906
Availability of data and material
All authors declare that all data and materials as well as software application or custom code support their published claims and comply with field standards.
Funding
This work was supported by the National Natural Sciences Foundation of China (grant no. 81801632 to Yz.Z.).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Lie Yang, Peng Xia, and Yangzhong Zhou. The first draft of the manuscript was written by Lie Yang and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
Consents were obtained from all authors before submission.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 191 kb)
Rights and permissions
About this article
Cite this article
Yang, L., Xia, P., Zhou, Y. et al. Characteristics and risk factors for Pneumocystis jirovecii pneumonia in patients with idiopathic membranous nephropathy. Eur J Clin Microbiol Infect Dis 40, 2305–2314 (2021). https://doi.org/10.1007/s10096-021-04227-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-021-04227-0