Abstract
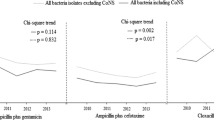
To conduct a survey of the local prevalent bacteria and antibiotic resistance in a referral tertiary neonatal intensive care unit (NICU), in order to assess the efficacy of local antibiotic policies. We reviewed all positive blood and cerebrospinal fluid cultures obtained between January 2007 and December 2017 in the NICU of Schneider Children’s Medical Center of Israel. Early and late-onset bacteremia were defined as episodes occurring within or after the first 3 calendar days of life respectively. Empiric treatment included ampicillin and gentamicin or piperacillin-tazobactam and amikacin for early or late-onset bacteremia respectively. The prevalence and antibiotic resistance of the bacteria were described and compared over time. Eight hundred and twenty nine of 15,947 (5.2%) newborns had at least one episode of bacteremia; 81 had multiple episodes. The most common bacteria were Escherichia coli (32.35%) and group B Streptococcus (19.11%) or coagulase negative Staphylococcus (CoNS) (60.5%) and Klebsiella sp. (12.4%) in early or late-onset bacteremia respectively. Overall, all Gram-positive bacteria were susceptible to vancomycin and most non-CoNS to ampicillin. Nosocomial vs. vertical bacteremia had increased resistance to ampicillin and cephalosporins. Resistance of nosocomial bacteria to piperacillin-tazobactam was 22.4%, to amikacin 3.3%, and to meropenem 1.8%. Changes over time: Gram-negative bacteria had a significant increase in resistance to cotrimoxazole and piperacillin. The resistance to gentamicin doubled. Our empiric antibiotic regimen covers the most frequent isolates. Amikacin may replace gentamicin for selected sick patients in early-onset bacteremia. Piperacillin-tazobactam should be combined with amikacin until susceptibility is available.

Similar content being viewed by others
References
Oza S, Lawn JE, Hogan DR, Mathers C, Cousens SN (2015) Neonatal cause-of-death estimates for the early and late neonatal periods for 194 countries: 2000-2013. Bull World Health Organ 93:19
Puopolo KM, Benitz WE, Zaoutis TE (2018) Committee on Fetus And Newborn, Committee on Infectious Diseases. Management of neonates born at ≥35 0/7 weeks’ gestation with suspected or proven early-onset bacterial sepsis. Pediatrics 142:e20182894
Hooven TA, Polin RA (2014) Healthcare-associated infections in the hospitalized neonate: a review. Early Hum Dev 90:S4–S6
Faour Kassem D, Shahar N, Ocampo S, Bader T, Zonis Z, Glikman D (2017) Bacteria without borders: a high carriage rate of antibiotic-resistant bacteria among Syrian children hospitalized in galilee medical center. Harefuah 156:298–301
Clinical and Laboratory Standards Institute (2015) Performance standards for antimicrobial susceptibility testing; approved standard—25th ed. CLSI document M100-S25. Clinical and Laboratory Standards Institute, Wayne
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332
Verani JR, McGee L, Schrag SJ (2010) Division of Bacterial Diseases, National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention (CDC). Prevention of perinatal group B streptococcal disease-revised guidelines from CDC, 2010. MMWR 19(59):1–36
Shane AL, Stoll BJ (2014) Neonatal sepsis: progress towards improved outcomes. J Infect 68:S24–S32
Brady MT, Polin RA (2013) Prevention and management of infants with suspected or proven neonatal sepsis. Pediatrics 132:166–168
Shane AL, Sánchez PJ, Stoll BJ (2017) Neonatal sepsis. Lancet 390:1770–1780
Flokas ME, Karanika S, Alevizakos M, Mylonakis E (2017) Prevalence of ESBL-producing Enterobacteriaceae in pediatric bloodstream infections: a systematic review and meta-analysis. PLoS One 12:e0171216
Piening BC, Geffers C, Gastmeier P, Schwab F (2017) Pathogen-specific mortality in very low birth weight infants with primary bloodstream infection. PLoS One 12:e0180134
Shane AL, Stoll BJ (2013) Recent developments and current issues in the epidemiology, diagnosis and management of bacterial and fungal neonatal sepsis. Am J Perinatol 30:131–141
Bromiker R, Arad I, Peleg O, Preminger A, Engelhard D (2001) Neonatal bacteremia: patterns of antibiotic resistance. Infect Control Hosp Epidemiol 22:767–770
May L, Klein EY, Rothman RE, Laxminarayan R (2014) Trends in antibiotic resistance in coagulase-negative staphylococci in the United States, 1999 to 2012. Antimicrob Agents Chemother 3:1404–1409
Goldstein BP (2014) Resistance to rifampicin: a review. J Antibiot 67:625–630
Sorlózano-Puerto A, Gómez-Luque JM, Luna-Del-Castillo JD, Navarro-Marí JM, Gutiérrez-Fernández J (2017) Etiological and resistance profile of bacteria involved in urinary tract infections in young children. Biomed Res Int 2017:4909452
Chazan B, Raz R, Teitler N, Nitzan O, Edelstein H, Colodner R (2009) Epidemiology and susceptibility to antimicrobials in community, hospital and long-term care facility bacteremia in northern Israel: a 6 year surveillance. Isr Med Assoc J 11:592–597
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the institutional review board (authorization number: RMC-0770-17).
Informed consent
No informed consent was required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mintz, A., Mor, M., Klinger, G. et al. Changing epidemiology and resistance patterns of pathogens causing neonatal bacteremia. Eur J Clin Microbiol Infect Dis 39, 1879–1884 (2020). https://doi.org/10.1007/s10096-020-03921-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-020-03921-9