Abstract
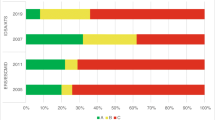
Invasive aspergillosis (IA) is a severe life-threatening infection with challenges in therapy. The aim was to evaluate the level of evidence (LOE) supporting recommendations in clinical practice guidelines (CPGs) of IA and changes over time. Search on CPG on IA released between 2000 and 2019 was done. Last versions were evaluated and compared with previous versions. Recommendations were classified by LOE as A (multiple randomized controlled trial (RCT) or meta-analysis), B (data from a single RCT or observational studies), or C (observational studies with limitations, case series, or expert opinion). Diagnosis recommendations were excluded. Five CPG from three groups of scientific societies were identified: the 2016 Infectious Diseases Society of America/American Thoracic Society (IDSA/ATS), 2017 European Society of Clinical Microbiology Infectious Diseases/European Confederation of Medical Mycology/European Respiratory Society (ESCMID/ECMM/ERS), 2018 Spanish Society of Infectious Diseases and Clinical Microbiology (SEIMC) CPGs, and their previous versions (2008 IDSA/ATS and 2011 GEMICOMED/SEIMC). ECMID/ECMM/ERS have not published any previous version. From 511 recommendations analyzed, 80 were classified as LOE A (15.7%), 223 LOE B (43.6%), and 208 LOE C (40.7%). Among 238 strong recommendations, only 57 (24.0%) were supported by LOE A. When comparing recent CPGs with previous versions, the proportion of recommendations supported by LOE A did not significantly increase over time (IDSA/ATS: 13.3% [2016] vs. 14.8% [2008], p = 0.798; and SEIMC: 22.6% [2018] vs. 19% [2011], p = 0.568). In conclusion, IA is a condition with an urgent unmet clinical need for more high-quality randomized trials.





Similar content being viewed by others
Abbreviations
- ACC:
-
American College of Cardiology
- AHA:
-
American Heart Association
- ATS:
-
American Thoracic Society
- CPG:
-
Clinical Practice Guidelines
- ECIL:
-
European Conference on Infections and Leukemia
- ECMM:
-
European Confederation of Medical Mycology
- ERS:
-
European Respiratory Society
- ESCMID:
-
European Society of Clinical Microbiology and Infectious Diseases
- GEMICOMED:
-
Grupo de Estudio de Micología Médica
- IA:
-
Invasive Aspergillosis
- IDSA:
-
Infectious Diseases Society of America
- IPA:
-
Invasive Pulmonary Aspergillosis
- LOE:
-
Level of Evidence
- MA:
-
Meta-analysis
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-analyses
- RCT:
-
Randomized Controlled Trial
- SEIMC:
-
Spanish Society of Infectious Diseases and Clinical Microbiology
- SR:
-
Systematic Review
References
Bitar D, Lortholary O, Le Strat Y, Nicolau J, Coignard B, Tattevin P, Che D, Dromer F (2014) Population-based analysis of invasive fungal infections, France, 2001-2010. Emerg Infect Dis 20:1149–1155
Cadena J, Thompson GR, Patterson TF (2016) Invasive aspergillosis: current strategies for diagnosis and management. Infect Dis Clin N Am 30:125–142
Schmiedel Y, Zimmerli S (2016) Common invasive fungal diseases: an overview of invasive candidiasis, aspergillosis, cryptococcosis, and Pneumocystis pneumonia. Swiss Med Wkly. https://doi.org/10.4414/smw.2016.14281
Sanguinetti M, Posteraro B, Beigelman-Aubry C, Lamoth F, Dunet V, Slavin M, Richardson MD (2019) Diagnosis and treatment of invasive fungal infections: looking ahead. J Antimicrob Chemother 74:ii27–ii37
Meyer C, Bowers A, Wayant C, Checketts J, Scott J, Musuvathy S, Vassar M (2018) Scientific evidence underlying the American College of Gastroenterology’s clinical practice guidelines. PLoS One 13:e0204720
Tricoci P, Allen JM, Kramer JM, Califf RM, Smith SC (2009) Scientific evidence underlying the ACC/AHA clinical practice guidelines. JAMA 301:831–841
Khan AR, Khan S, Zimmerman V, Baddour LM, Tleyjeh IM (2010) Quality and strength of evidence of the Infectious Diseases Society of America clinical practice guidelines. Clin Infect Dis 51:1147–1156
Brozek JL, Akl EA, Alonso-Coello P et al (2009) Grading quality of evidence and strength of recommendations in clinical practice guidelines. Part 1 of 3. An overview of the GRADE approach and grading quality of evidence about interventions. Allergy 64:669–677
Guyatt GH, Cook DJ, Jaeschke R, Pauker SG, Schünemann HJ (2008) Grades of recommendation for antithrombotic agents: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest 133:123S–131S
Canadian Task Force on the Periodic Health Examination (1979) The Canadian guide to clinical preventive health care. Can Med Assoc J 121:1193–1254
Lee DH, Vielemeyer O (2011) Analysis of overall level of evidence behind Infectious Diseases Society of America practice guidelines. Arch Intern Med 171:18–22
Jacobs AK, Kushner FG, Ettinger SM et al (2013) ACCF/AHA clinical practice guideline methodology summit report: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Am Coll Cardiol 61:213–265
Wan K, Liang H, Yan G, Zou B, Huang C, Jiang M (2019) A quality assessment of evidence-based guidelines for the prevention and management of ventilator-associated pneumonia: a systematic review. J Thorac Dis 11:2795–2807
Campogiani L, Tejada S, Ferreira-Coimbra J, Restrepo MI, Rello J (2019) Evidence supporting recommendations from international guidelines on treatment, diagnosis, and prevention of HAP and VAP in adults. Eur J Clin Microbiol Infect Dis
Patterson TF, Thompson GR, Denning DW et al (2016) Executive summary: practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis 63:433–442
Walsh TJ, Anaissie EJ, Denning DW et al (2008) Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis 46:327–360
Ullmann AJ, Aguado JM, Arikan-Akdagli S et al (2018) Diagnosis and management of Aspergillus diseases: executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin Microbiol Infect 24(Suppl 1):e1–e38
Garcia-Vidal C, Alastruey-Izquierdo A, Aguilar-Guisado M et al (2018) Executive summary of clinical practice guideline for the management of invasive diseases caused by Aspergillus: 2018 update by the GEMICOMED-SEIMC/REIPI. Enferm Infecc Microbiol Clin. https://doi.org/10.1016/j.eimc.2018.03.018
Fortún J, Carratalá J, Gavaldá J et al (2011) Guidelines for the treatment of invasive fungal disease by Aspergillus spp. and other fungi issued by the Spanish Society of Infectious Diseases and Clinical Microbiology (SEIMC). 2011 update. Enferm Infecc Microbiol Clin 29:435–454
Fanaroff AC, Califf RM, Windecker S, Smith SC, Lopes RD (2019) Levels of Evidence Supporting American College of Cardiology/American Heart Association and European Society of Cardiology Guidelines, 2008-2018. JAMA 321:1069–1080
Tissot F, Agrawal S, Pagano L, Petrikkos G, Groll AH, Skiada A, Lass-Flörl C, Calandra T, Viscoli C, Herbrecht R (2017) ECIL-6 guidelines for the treatment of invasive candidiasis, aspergillosis and mucormycosis in leukemia and hematopoietic stem cell transplant patients. Haematologica 102:433–444
De Pauw B, Walsh TJ, Donnelly JP, et al (2008) Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis 46:1813–1821
Acknowledgments
Authors appreciate comments from Maria Teresa Martin, Microbiology Department, Vall d’Hebron University Hospital who helped to improve the final manuscript.
Funding
This work was funded in part by CIBERES, Instituto Salud Carlos III, Madrid, Spain (Fondos FEDER) (CB06–06-036). Dr. Blot holds a research mandate of the Special Research Fund at Ghent University.
Author information
Authors and Affiliations
Contributions
JR and ST designed the study. The recommendations were abstracted by a single reviewer (ST) and validated by two other reviewers (LC and JFC). ST analyzed data and writes the first manuscript draft. SJB provided statistical analyses and write methods. All authors approved the final version of the manuscript. ST takes full responsibility for the integrity of reported data.
Corresponding author
Ethics declarations
Competing interests
Dr. Rello has served as consultant and in the speakers’ bureau for Pfizer and Astellas. Dr. Blot received research grants from Pfizer. The remaining authors have no conflicts of interest to declare.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tejada, S., Campogiani, L., Ferreira-Coimbra, J. et al. Levels of evidence supporting clinical practice guidelines on invasive aspergillosis. Eur J Clin Microbiol Infect Dis 39, 903–913 (2020). https://doi.org/10.1007/s10096-019-03794-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-019-03794-7