Abstract
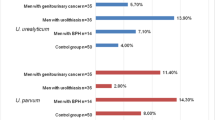
The aim of this study was to determine the occurrence of urogenital mycoplasmas in urogenital tract of women with systemic lupus erythematosus (SLE). The study group included 36 women diagnosed with SLE and 100 healthy controls. Mycoplasmas were detected with microculture and PCR in 13/36 (36.1%) women with SLE and in 25/100 (25%) controls. In both groups, U. parvum occurred significantly more frequently. M. genitalium was detected in 3/36 (8.3%) SLE patients and in 3/100 (3%) controls. FVU as a material decreased the number of positive results from 33.3% to 30.6% compared with swabs.
Although the incidence of mycoplasmas in urogenital tract of women with SLE and controls did not differ statistically, it is important to consider them as a potential etiology of urogenital infection when clinical symptoms are present, but etiology is unknown or uncertain.
Similar content being viewed by others
References
Rúa-Figueroa Í, López-Longo J, Galindo-Izquierdo M et al (2017) Incidence, associated factors and clinical impact of severe infections in a large, multicentric cohort of patients with systemic lupus erythematosus. Semin Arthritis Rheum 47:38–45. https://doi.org/10.1016/j.semarthrit.2017.01.010
Cervera R, Khamashta MA, Font J et al; European Working Party on Systemic Lupus Erythematosus (2003) Morbidity and mortality in systemic lupus erythematosus during a 10-year period: a comparison of early and late manifestations in a cohort of 1,000 patients. Medicine (Baltimore) 82: 299-308 https://doi.org/10.1097/01.md.0000091181.93122.55
Leli C, Mencacci A, Latino MA, Clerici P (2018) Prevalence of cervical colonization by Ureaplasma parvum, Ureaplasma urealyticum, Mycoplasma hominis and Mycoplasma genitalium in childbearing age women by a commercially available multiplex real-time PCR: an Italian observational multicentre study. J Microbiol Immunol Infect 51:220–225. https://doi.org/10.1016/j.jmii.2017.05.004
Del Prete R, Ronga L, Lestingi M et al (2017) Simultaneous detection and identification of STI pathogens by multiplex real-time PCR in genital tract specimens in a selected area of Apulia, a region of Southern Italy. Infection 45:469–477. https://doi.org/10.1007/s15010-017-1002-7
Taylor-Robinson D (2017) Mollicutes in vaginal microbiology: Mycoplasma hominis Ureaplasma urealyticum, Ureaplasma parvum and Mycoplasma genitalium. Res Microbiol 168:875–881. https://doi.org/10.1016/j.resmic.2017.02.009
Workowski KA, Bolan GA, Centers for Disease Control and Prevention (2015) Sexually transmitted diseases treatment guidelines. MMWR Recomm Rep 64:1–137
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725. https://doi.org/10.1002/art.1780400928
Kong F, Ma Z, James G et al (2000) Species identification and subtyping of Ureaplasma parvum and Ureaplasma urealyticum using PCR-based assays. J Clin Microbiol 38:1175–1179
Jensen JS, Uldum SA, Søndergård-Andersen J, Vuust J, Lind K (1991) Polymerase chain reaction for detection of Mycoplasma genitalium in clinical samples. J Clin Microbiol 29:46–50
Jensen JS, Borre MB, Dohn B (2003) Detection of Mycoplasma genitalium by PCR amplification of the 16S rRNA gene. J Clin Microbiol 41:261–266. https://doi.org/10.1128/jcm.41.1.261-266.2003
Nugent RP, Krohn MA, Hillier SL (1991) Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol 29:297–301
Schwartz DJ, Elward A, Storch GA et al (2019) Ureaplasma urealyticum pyelonephritis presenting with progressive dysuria, renal failure, and neurologic symptoms in an immunocompromised patient. Transpl Infect Dis 21:e13032. https://doi.org/10.1111/tid.13032
Unemo M, Salado-Rasmussen K, Hansen M et al (2018) Clinical and analytical evaluation of the new Aptima Mycoplasma genitalium assay, with data on M. genitalium prevalence and antimicrobial resistance in M. genitalium in Denmark, Norway and Sweden in 2016. Clin Microbiol Infect 24:533–539. https://doi.org/10.1016/j.cmi.2017.09.006
Wroblewski JK, Manhart LE, Dickey KA et al (2006) Comparison of transcription-mediated amplification and PCR assay results for various genital specimen types for detection of Mycoplasma genitalium. J Clin Microbiol 44:3306–3312. https://doi.org/10.1128/JCM.00553-06
Ekiel AM, Pietrzak B, Kamiński P et al (2009) Prevalence of urogenital mycoplasmas and ureaplasmas in women after kidney transplantation. Transplantation 87:848–851. https://doi.org/10.1097/TP.0b013e318199d19a
Marovt M, Keše D, Kotar T et al (2015) Ureaplasma parvum and Ureaplasma urealyticum detected with the same frequency among women with and without symptoms of urogenital tract infection. Eur J Clin Microbiol Infect Dis 34:1237–4125. https://doi.org/10.1007/s10096-015-2351-8
Méndez-Martínez S, García-Carrasco M, Cedillo-Ramírez ML et al (2017) Genital Mycoplasma infection among Mexican women with systemic lupus erythematosus. Int J Gynaecol Obstet 138:17–22. https://doi.org/10.1002/ijgo.12154
Geissdörfer W, Sandner G, John S et al (2008) Ureaplasma urealyticum meningitis in an adult patient. J Clin Microbiol 46:1141–1143. https://doi.org/10.1128/JCM.01628-07
Eilers E, Moter A, Bollmann R et al (2007) Intrarenal abscesses due to Ureaplasma urealyticum in a transplanted kidney. J Clin Microbiol 45:1066–1068. https://doi.org/10.1128/JCM.01897-06
Yager JE, Ford ES, Boas ZP et al (2010) Ureaplasma urealyticum continuous ambulatory peritoneal dialysis-associated peritonitis diagnosed by 16S rRNA gene PCR. J Clin Microbiol 48:4310–4314. https://doi.org/10.1128/JCM.01045-10
Gassiep I, Gore L, Dale JL et al (2017) Ureaplasma urealyticum necrotizing soft tissue infection. J Infect Chemother 23:830–832. https://doi.org/10.1016/j.jiac.2017.07.007
Rohner P, Schnyder I, Ninet B et al (2004) Severe Mycoplasma hominis infections in two renal transplant patients. Eur J Clin Microbiol Infect Dis 23:203–204. https://doi.org/10.1007/s10096-003-1097-x
van der Bijl AE, Kamper AM, de Fijter JW et al (2000) Mycoplasma hominis peritonitis after renal transplantation. Nephron 86:541–542. https://doi.org/10.1159/000045862
Pastural M, Audard V, Bralet MP et al (2002) Mycoplasma hominis infection in renal transplantation. Nephrol Dial Transplant 17:495–496. https://doi.org/10.1093/ndt/17.3.495
Okumura Y, Kajihara T, Koba Y et al (2018) Multiple intraabdominal abscesses caused by Mycoplasma hominis infection following simultaneous pancreas-kidney transplantation. Ann Lab Med 38: 381-383 https://doi.org/10.3343/alm.2018.38.4.381.
Funding
This study was supported by the grant from the Medical University of Silesia (KNW-1-061/K/8/O).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were approved by the local Bioethical Committee (KNW/0022/KB1/88/09) and in accordance with the 1964 Helsinki Declaration and its later amendments. All study subjects agreed to participate in the study and signed an informed consent form.
Statement of informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alicja, E., Małgorzata, R., Małgorzata, A. et al. Prevalence of urogenital mycoplasmas in women with systemic lupus erythematosus (SLE): preliminary study. Eur J Clin Microbiol Infect Dis 39, 717–721 (2020). https://doi.org/10.1007/s10096-019-03783-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-019-03783-w