Abstract
Purpose
Clostridium difficile infection (CDI) is the most common cause of nosocomial diarrhea in adult patients and is associated with considerable morbidity and mortality. Apart from the standard treatment regimens, tigecycline has shown significant in vitro activity against C. difficile but data regarding its clinical impact remains controversial. The aim of this article is to update the evidence related to the clinical role of tigecycline against C. difficile.
Methods
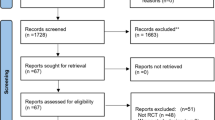
PubMed and Scopus databases were searched for relevant literature published from January 2015 to July 2018.
Results
Six retrospective cohort studies, 1 prospective study, 1 case series, and 2 case reports provided data regarding the effectiveness of tigecycline against C. difficile and were included in our evaluation. Also, we performed a meta-analysis based on 186 patients (from 4 studies) that showed clinical cure 79% (95% CI 73.0–84.5%).
Conclusion
Despite the heterogeneity of the included studies and the small number of patients, the available evidence suggests that tigecycline might be considered as a potential therapeutic option for patients with CDIs, especially in severe cases.


Similar content being viewed by others
Abbreviations
- CDI:
-
Clostridium difficile infection
- ESCMID:
-
European Society of Clinical Microbiology and Infectious Diseases
- IDSA:
-
Infectious Diseases Society of America
- NR:
-
Not reported
References
McDonald LC, Gerding DN, Johnson S, Bakken JS, Carroll KC, Coffin SE et al (2018) Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis 66:e1–e48
Barbut F, Jones G, Eckert C (2011) Epidemiology and control of Clostridium difficile infections in healthcare settings: an update. Curr Opin Infect Dis 24:370–376
Debast SB, Bauer MP, Kuijper EJ (2014) European Society of Clinical Microbiology and Infectious Diseases: update of the treatment guidance document for Clostridium difficile infection. Clin Microbiol Infect 20(Suppl 2):1–26
Surveillance for community-associated Clostridium difficile--Connecticut, 2006. MMWR Morb Mortal Wkly Rep. 2008;57:340-3.
Petrosillo N, Granata G, Cataldo MA. Novel antimicrobials for the treatment of Clostridium difficile infection. Front Med (Lausanne). 2018;5:96.
Rose WE, Rybak MJ (2006) Tigecycline: first of a new class of antimicrobial agents. Pharmacotherapy. 26:1099–1110
Di Bella S, Nisii C, Petrosillo N (2015) Is tigecycline a suitable option for Clostridium difficile infection? Evidence from the literature. Int J Antimicrob Agents 46:8–12
Navalkele BD, Lerner SA (2016) Intravenous tigecycline facilitates cure of severe Clostridium difficile Infection (CDI) after failure of standard therapy: a case report and literature review of tigecycline use in CDI. Open Forum Infect Dis 3:ofw094
Hecht DW, Galang MA, Sambol SP, Osmolski JR, Johnson S, Gerding DN (2007) In vitro activities of 15 antimicrobial agents against 110 toxigenic clostridium difficile clinical isolates collected from 1983 to 2004. Antimicrob Agents Chemother 51:2716–2719
Knafl D, Winhofer Y, Lotsch F, Weisshaar S, Steininger C, Burgmann H et al (2016) Tigecycline as last resort in severe refractory Clostridium difficile infection: a case report. J Hosp Infect 92:296–298
Dumitru IM, Dumitru E, Rugina S, Tuta LA (2017) Toxic megacolon - a three case presentation. J Crit Care Med (Targu Mures) 3:39–44
Gergely Szabo B, Kadar B, Szidonia Lenart K, Dezsenyi B, Kunovszki P, Fried K et al (2016) Use of intravenous tigecycline in patients with severe Clostridium difficile infection: a retrospective observational cohort study. Clin Microbiol Infect 22:990–995
Brinda BJ, Pasikhova Y, Quilitz RE, Thai CM, Greene JN (2017) Use of tigecycline for the management of Clostridium difficile colitis in oncology patients and case series of breakthrough infections. J Hosp Infect 95:426–432
LaSalvia MT, Branch-Elliman W, Snyder GM, Mahoney MV, Alonso CD, Gold HS et al (2017) Does Adjunctive Tigecycline Improve Outcomes in Severe-Complicated, Nonoperative Clostridium difficile Infection? Open Forum Infect Dis 4:ofw264
Manea E, Sojo-Dorado J, Jipa RE, Benea SN, Rodriguez-Bano J, Hristea A (2018) The role of tigecycline in the management of Clostridium difficile infection: a retrospective cohort study. Clin Microbiol Infect 24:180–184
Bishop EJ, Tiruvoipati R, Metcalfe J, Marshall C, Botha J, Kelley PG (2018) The outcome of patients with severe and severe-complicated Clostridium difficile infection treated with tigecycline combination therapy: a retrospective observational study. Intern Med J 48:651–660
Mirea L (2017) Efficacy of tigecycline treatment in severe and complicated Clostridium difficile infection. Pharmacia. 65
Kundrapu S, Hurless K, Sunkesula VC, Tomas M, Donskey CJ (2015) Tigecycline exhibits inhibitory activity against Clostridium difficile in the intestinal tract of hospitalised patients. Int J Antimicrob Agents 45:424–426
Ooijevaar RE, van Beurden YH, Terveer EM, Goorhuis A, Bauer MP, Keller JJ et al (2018) Update of treatment algorithms for Clostridium difficile infection. Clin Microbiol Infect 24:452–462
Preda CM, Meianu C, Sandra I, Becheanu G, Dumbrava M, Manuc M et al (2016) Fecal microbiota transplantation in recurrent NAP1/B1/027 Clostridium difficile infection (CDI) resistant to vancomycin and metronidazole in a patient with ulcerative colitis (UC): a case report. Rev Med Chir Soc Med Nat Iasi 120:563–567
Vindigni SM, Surawicz CM (2017) Fecal microbiota transplantation. Gastroenterol Clin N Am 46:171–185
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MEF participated in advisory boards of AstraZeneca, InfectoPharm, Tetraphase, Shionogi, and Xellia; received lecture honoraria from Cipla, Merck, and Pfizer; and received research support from Shionogi, Tetraphase, Helperby, and Xellia. The other authors have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kechagias, K.S., Chorepsima, S., Triarides, N.A. et al. Tigecycline for the treatment of patients with Clostridium difficile infection: an update of the clinical evidence. Eur J Clin Microbiol Infect Dis 39, 1053–1058 (2020). https://doi.org/10.1007/s10096-019-03756-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-019-03756-z