Abstract
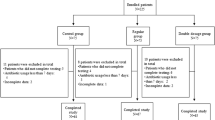
An unabsorbed dietary iron supplementation can modify the colonic microbiota equilibrium and favor the growth of pathogenic strains over barrier strains. Nevertheless, the impact of oral iron supplements (OIS) use on the clinical outcomes of patients with gram-negative bacteremia (GNB) has not been evaluated. To explore the impact of OIS on the outcomes of patients with GNB. A retrospective study conducted in a tertiary hospital including patients with GNB during 2011–2016. The entire cohort was divided into chronic OIS users (study group) and nonusers (control group). The two groups were compared for the study outcomes, septic shock at presentation, length of hospital stay (LOS), and short-term mortality. The study cohort included 232 patients; 44 patients in the study group and 188 in the control one. There was no any significant difference in demographic and comorbidities characteristics between the two groups. Escherichia coli comprised the majority of bacteria (69%), while the urinary tract was the main source of the bacteremia. OIS alone and after adjustment was significantly associated with septic shock at presentation (OR = 2, CI95% [1.03–5], p = 0.04 and OR = 5, CI95% [1.4–15], p = 0.01, respectively). By multivariate analysis, OIS was significantly associated with 30-day mortality (OR = 3, CI95% [1.05–7], p = 0.04), but had no impact on LOS (16 + 23 vs. 12 + 15, p = 0.9). There is a significant association between chronic OIS exposure and increased adverse outcomes in patients with GNB. These findings might have important clinical implications.
Similar content being viewed by others
References
Miller JL (2013) Iron deficiency anemia: a common and curable disease. Cold Spring Harb Perspect Med 3(7)
Cross JH (2015) Oral iron acutely elevates bacterial growth in human serum. Sci Rep 5:16670
Weinberg ED (2009) Iron availability and infection. Biochim Biophys Acta 1790(7):600–605
Andrews SC (2003) Bacterial iron homeostasis. FEMS Microbiol Rev 27(2–3):215–237
Bezkorovainy A, Kot E, Miller-Catchpole R, Halofis G, Furmanov S (1996) Iron metabolism in bifidobacteria. Int Dairy J 6:905–919
Naikare H, Palyada K (2006) Major role for FeoB in Campylobacter jejuni ferrous iron acquisition, gut colonization, and intracellular survival. Infect Immun 74(10):5433–5444
Zimmermann MB, Chassard C (2010) The effects of iron fortification on the gut microbiota in African children: a randomized controlled trial in Cote d'Ivoire. Am J Clin Nutr 92(6):1406–1415
Suárez CJ, Lolans K, Villegas MV, Quinn JP (2005) Mechanisms of resistance to beta-lactams in some common gram-negative bacteria causing nosocomial infections. Expert Rev Anti-Infect Ther 3(6):915–922
Sligl W, Taylor G, Brindley PG (2006) Five years of nosocomial gram-negative bacteremia in a general intensive care unit: epidemiology, antimicrobial susceptibility patterns, and outcomes. Int J Infect Dis 10(4):320–325
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS international Sepsis definitions conference. Crit Care Med 31(4):1250–1256
Meurman O, Koskensalo A, Rantakokko-Jalava K (2006) Evaluation of Vitek 2 for identification of yeasts in the clinical laboratory. Clin Microbiol Infect 12(6):591–593
Dhiman N, Hall L, Wohlfiel SL, Buckwalter SP, Wengenack NL (2011) Performance and cost analysis of matrix-assisted laser desorption ionization-time of flight mass spectrometry for routine identification of yeast. J Clin Microbiol 49(4):1614–1616
Neuberger A, Okebe J, Yahav D, Paul M (2016) Oral iron supplements for children in malaria-endemic areas. Cochrane Database Syst Rev 27(2):CD006589
Ishida JH, Johansen KL (2014) Iron and infection in hemodialysis patients. Semin Dial 27(1):26–36
Parkkinen J, von Bonsdorff L, Peltonen S, Gronhagen-Riska C, Rosenlof K (2000) Catalytically active iron and bacterial growth in serum ofhaemodialysis patients after i.v. iron-saccharate administration. Nephrol Dial Transplant 15(11):1827–1834
Deicher R, Ziai F, Cohen G, Mullner M, Horl WH (2003) High-dose parenteral iron sucrose depresses neutrophil intracellular killing capacity. Kidney Int 64(2):728–736
Sengoelge G, Kletzmayr J, Ferrara I, Perschl A, Horl WH, SunderPlassmann G (2003) Impairment of transendothelial leukocyte migration by iron complexes. J Am Soc Nephrol 14(10):2639–2644
Ichii H, Masuda Y, Hassanzadeh T, Saffarian M, Gollapudi S, Vaziri ND (2012) Iron sucrose impairs phagocytic function and promotes apoptosis in polymorphonuclear leukocytes. Am J Nephrol 36(1):50–57
Van Asbeck BS, Marx JJ, Struyvenberg A, van Kats JH, Verhoef J (1984) Effect of iron (III) in the presence of various ligands on the phagocytic and metabolic activity of human polymorphonuclear leukocytes. J Immunol 132(2):851–856
Mencacci A, Cenci E, Boelaert JR, Bucci P, Mosci P, Fe d’Ostiani C et al (1997) Iron overload alters innate and T helper cell responses to Candida albicans in mice. J Infect Dis 175(6):1467–1476
Author information
Authors and Affiliations
Contributions
Study concept and design: Elis A, Bishara J, and Atamna A contributed to study conception and design and analyzed the data
Acquisition, analysis, or interpretation of data: all authors
Drafting the manuscript: Atamna A and Hamud H draft the manuscript
Critical revision of the manuscript for important intellectual content: all authors
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the hospital’s Ethics Committee.
Informed consent
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was performed in partial fulfillment of the M.D. thesis requirement of the Sackler Faculty of Medicine, Tel Aviv University.
Rights and permissions
About this article
Cite this article
Atamna, A., Hamud, H., Daud, W. et al. Chronic use of oral iron supplements is associated with poor clinical outcomes in patients with gram-negative bacteremia. Eur J Clin Microbiol Infect Dis 38, 689–693 (2019). https://doi.org/10.1007/s10096-019-03481-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-019-03481-7