Abstract
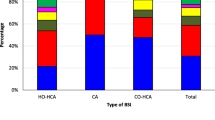
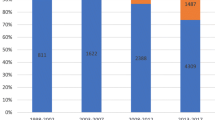
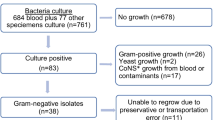
We aimed to identify the carbapenem-resistant Gram-negative bacteria (GNB) causing catheter-related bloodstream infections (CRBSI) in intensive care units (ICU) in a tertiary care Egyptian hospital, to study their resistance mechanisms by phenotypic and genetic tests, and to use ERIC-PCR for assessing their relatedness. The study was conducted over 2 years in three ICUs in a tertiary care hospital in Egypt during 2015–2016. We identified 194 bloodstream infections (BSIs); 130 (67.01%) were caused by GNB, of which 57 were isolated from CRBSI patients (73.84%). Identification of isolates was performed using conventional methods and MALDI-TOF MS. Antimicrobial susceptibility testing (AST) was done by disc diffusion following CLSI guidelines. Phenotypic detection of carbapenemases enzymes activity was by modified Hodge test and the Carba-NP method. Isolates were investigated for the most common carbapenemases encoding genes blaKPC, blaNDM, and blaOXA-48 using multiplex PCR. Molecular typing of carbapenem-resistant isolates was done by ERIC-PCR followed by sequencing of common resistance genes. The overall rate of CRBSI in our study was 3.6 per 1000 central venous catheter (CVC) days. Among 57 Gram-negative CRBSI isolates, Klebsiella pneumoniae (K. pneumoniae) was the most frequently isolated (27/57; 47.4%), of which more than 70% were resistant to Meropenem. Phenotypic tests for carbapenemases showed that 37.9% of isolates were positive by modified Hodge test and 63.8% by Carba-NP detection. Multiplex PCR assay detected the blaNDM in 28.6% of the isolates and blaKPC in 26.8%, blaNDM and blaKPC were detected together in the same isolate in 5.6%, while blaOXA-48-like were not detected. ERIC-PCR detected limited genetic relatedness between K. pneumoniae isolates. Elevated resistance rates were observed to all antibiotics including carbapenems among K. pneumoniae isolates causing CRBSI. ERIC-PCR showed that the resistant isolates were mainly polyclonal. Our results call for reinforcement of antimicrobial stewardship and measures to prevent CRBSI.

Similar content being viewed by others
References
Vincent JL, Rello J, Marshall J et al (2009) International study of the prevalence and outcomes of infection in intensive care units. JAMA 302(21):2323–2329
Russotto V, Cortegiani A, Graziano G, Saporito L, Raineri SM, Mammina C, Giarratano A (2015) Bloodstream infections in intensive care unit patients: distribution and antibiotic resistance of bacteria. Infect Drug Resist 8:287–296
Paterson DL (2006) Resistance in gram-negative bacteria: Enterobacteriaceae. Am J Infect Control 34:S20–S28 S64 –S73
Ammerlaan H, Harbarth S, Buiting A et al (2013) Secular trends in nosocomial bloodstream infections: antibiotic-resistant bacteria increase the total burden of infection. Clinical Infect Dis 56(6):798–805
Qureshi ZA, Paterson DL, Potoski BA, Kilayko MC, Sandovsky G, Sordillo E et al (2012) Treatment outcome 478 of bacteremia due to KPC-producing Klebsiella pneumoniae: superiority of 479 combination antimicrobial regimens. AntimicrobAgents Chemother 56:2108–2480 2113
Livermore DM, Woodford N (2006) The beta-lactamase threat in Enterobacteriaceae, Pseudomonas and Acinetobacter. Trends Microbiol 14:413–420
Montero JG, Lerma FÁ, Galleymore PR et al (2015) Combatting resistance in intensive care: the multimodal approach of the Spanish ICU “Zero Resistance” program. Crit Care 19:114. https://doi.org/10.1186/s13054-015-0800-5
Talaat M, El-Shokry M, El-Kholy J, Ismail G, Kotb S, Hafez S, Attia E, Lessa FC (2016) National surveillance of health care–associated infections in Egypt: developing a sustainable program in a resource-limited country. Am J Infect Control 44(11):1296–1301. https://doi.org/10.1016/j.ajic.2016.04.212
Centres for Disease Control and Prevention/ National Healthcare Safety Network. Surveillance definition of healthcare-associated infection and criteria for specific types of infections in the acute care setting. Available from: http://www.cdc.gov/nhsn/PDFs/pscManual/17pscNosInfDef_current.pdf. Accessed 28 Sept 2016
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332
Noyal MJC, Menezes GA, Sujatha BN, Harish S, Parija SC (2009) Simple screening tests for detection of carbapenemases in clinical isolates of non-fermentative Gram-negative bacteria. Indian J Med Res 129:707–712
Nordmann P, Poirel L, Dortet L (2012) Rapid detection of carbapenemase producing Enterobacteriaceae. Emerg Infect Dis:1503–1507
Poirel L, Walsh TR, Cuvillier TR, Nordmann P (2011) Multiplex PCR for detection of acquired carbapenemase genes. Infect Dis 119–123
El Kholy A, Baseem H, Hall GS, Procop GW, Longworth DL (2003) Antimicrobial resistance in Cairo, Egypt 1999–2000: a survey of five hospitals. JAC 51:625–630
Ribeiro PC, Monteiro AS, Marques SG, Monteiro SG, Monteiro-Neto V, Coqueiro MM, Marques AC (2016) Phenotypic and molecular detection of the blaKPC gene in clinical isolates from inpatients at hospitals in São Luis, MA, Brazil. BMC Infect Dis 16:737
Rosenthal VD, Al-Abdely HM, El-Kholy AA et al (2016) International Nosocomial Infection Control Consortium report, data: summary of 50 countries for 2010–2015,. Device-associated module. Am J Infect Control 44(12):1495–1504
Talaat M, Saied T, Kandeel A, El-Ata GA, El-Kholy A et al (2014) A point prevalence survey of antibiotic use in 18 hospitals in Egypt. Antibiotics 3:450–460
Satlin MJ, Jenkins SJ, And Walsh TJ (2014) The global challenge of carbapenem-resistant enterobacteriaceae in transplant recipients and patients with hematologic malignancies. Clin Infect Dis 58(9):1274–1283
Sievert DM, Ricks P, Edwards JR, Schneider A, Patel J, Srinivasan A et al (2013) Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the national healthcare safety network at the centers for disease control and prevention, 2009-2010. Infect Control Hosp Epidemiol 34:1–14
Khan MA (2012) Bacterial spectrum and susceptibility patterns of pathogens in ICU and IMCU of a secondary care hospital in Kingdom of Saudi Arabia. Int J Path 10:64–70
Rubio FG, Oliveira VD, Rangel RM, Nogueira MC, Almeida MT (2013) Trends in bacterial resistance in a tertiary university hospital over one decade. Braz J Infect Dis 17:480–482
Shibl A, Al-Agamy A, Memish Z, Senok A, Abdul Khader S, Assiri A et al (2013) The emergence of OXA-48- and NDM-1-positive Klebsiella pneumoniae in Riyadh, Saudi Arabia. Int J Infect Dis 17(12):1130–1133
Amer WH, Khalil HS, Abd EL Wahab MAA (2016) Risk factors, phenotypic and genotypic characterization of carbapenem resistant Enterobacteriaceae in Tanta University Hospitals, Egypt. Int J Infect Control v12:i2
Mohamed ER, Aly SA, Halby HM, Ahmed SH, Zakaria AM, El-Asheer OM (2017) Epidemiological typing of multidrug-resistant Klebsiella pneumoniae, which causes paediatric ventilator-associated pneumoniae in Egypt. J Med Microbiol 66(5):628–634
Gozalan A, Coskun-Ari FF, Ozdem B, Unaldi O, Celikbilek N, Kirca F, Aydogan S, Muderris T, Guven T, Acikgoz ZC, Durmaz R (2015) Molecular characterization of vancomycin-resistant Enterococcus faecium strains isolated from carriage and clinical samples in a tertiary hospital, Turkey. J Med Microbiol 64(7):759–766
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abdulall, A.K., Tawfick, M.M., El Manakhly, A.R. et al. Carbapenem-resistant Gram-negative bacteria associated with catheter-related bloodstream infections in three intensive care units in Egypt. Eur J Clin Microbiol Infect Dis 37, 1647–1652 (2018). https://doi.org/10.1007/s10096-018-3294-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3294-7