Abstract
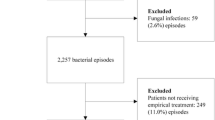
The objective of this study was to explore whether the percentage of inappropriate empirical antibiotic treatment in patients with bacteremia changed over time and to understand the factors that brought on the change. Three prospective cohorts of patients with bacteremia in three different periods (January 1st, 1988 to December 31st, 1989; May 1st, 2004 to November 30, 2004; May 1st, 2010 to April 30, 2011) were compared. Analysis was performed on a total of 811 patients. In 2010–2011, 55.9% (76/136) of patients with bacteremia received inappropriate empirical treatment, compared with 34.5% (170/493) and 33.5% (55/164) in the first and second periods, respectively, in a significant upward trend (p = 0.001). Resistance to antibiotics increased significantly during the study period. The following variables were included in the multivariate analysis assessing risk factors for inappropriate empirical treatment: study period (third period) [odds ratio, OR = 2.766 (95% confidence interval, CI, 1.655–4.625)], gender (male) [OR = 1.511 (1.014–2.253)], pathogen carrying extended-spectrum beta-lactamases [OR = 10.426 (4.688–23.187)], multidrug-resistant Acinetobacter baumannii [OR = 5.428 (2.181–13.513)], and skin/soft infections [OR = 3.23 (1.148–9.084)]. A model excluding microbiological data included: gender (male) [OR = 1.648 (1.216–2.234)], study period (third period) [OR = 2.446 (1.653–3.620)], hospital-acquired infection [OR = 1.551 (1.060–2.270)], previous use of antibiotics [OR = 1.815 (1.247–2.642)], bedridden patient [OR = 2.019 (1.114–3.658)], and diabetes mellitus [OR = 1.620 (1.154–2.274)]. We have observed a worrisome increase in the rate of inappropriate empirical treatment of bacteremia. We need tools that will allow us better prediction of the pathogen and its susceptibilities during the first hours of managing a patient suspected of a severe bacterial infection.
Similar content being viewed by others
References
Schwaber MJ, Navon-Venezia S, Kaye KS, Ben-Ami R, Schwartz D, Carmeli Y (2006) Clinical and economic impact of bacteremia with extended-spectrum-beta-lactamase-producing Enterobacteriaceae. Antimicrob Agents Chemother 50:1257–1262
Leibovici L, Shraga I, Andreassen S (1999) How do you choose antibiotic treatment? BMJ 318:1614–1618
Paul M, Shani V, Muchtar E, Kariv G, Robenshtok E, Leibovici L (2010) Systematic review and meta-analysis of the efficacy of appropriate empiric antibiotic therapy for sepsis. Antimicrob Agents Chemother 54:4851–4863
Leibovici L, Samra Z, Konisberger H, Kalter-Leibovici O, Pitlik SD, Drucker M (1991) Bacteremia in adult diabetic patients. Diabetes Care 14(2):89–94
Leibovici L, Konisberger H, Pitlik SD, Samra Z, Drucker M (1992) Bacteremia and fungemia of unknown origin in adults. Clin Infect Dis 14(2):436–443
Leibovici L, Konisberger H, Pitlik SD, Samra Z, Drucker M (1992) Patients at risk for inappropriate antibiotic treatment of bacteraemia. J Intern Med 231(4):371–374
Paul M, Gafter-Gvili A, Leibovici L, Bishara J, Levy I, Yaniv I, Shalit I, Samra Z, Pitlik S, Konigsberger H, Weinberger M (2007) The epidemiology of bacteremia with febrile neutropenia: experience from a single center, 1988–2004. Isr Med Assoc J 9(6):424–429
Fraser A, Paul M, Almanasreh N, Tacconelli E, Frank U, Cauda R, Borok S, Cohen M, Andreassen S, Nielsen AD, Leibovici L; TREAT Study Group (2006) Benefit of appropriate empirical antibiotic treatment: thirty-day mortality and duration of hospital stay. Am J Med 119(11):970–976
Endimiani A, Tamborini A, Luzzaro F, Lombardi G, Toniolo A (2003) A two-year analysis of risk factors and outcome in patients with bloodstream infection. Jpn J Infect Dis 56(1):1–7
Gasch O, Ayats J, Angeles Dominguez M, Tubau F, Liñares J, Peña C, Grau I, Pallarés R, Gudiol F, Ariza J, Pujol M (2011) Epidemiology of methicillin-resistant Staphylococcus aureus (MRSA) bloodstream infection: secular trends over 19 years at a university hospital. Medicine (Baltimore) 90(5):319–327
Kang CI, Kim SH, Park WB, Lee KD, Kim HB, Kim EC, Oh MD, Choe KW (2005) Bloodstream infections caused by antibiotic-resistant gram-negative bacilli: risk factors for mortality and impact of inappropriate initial antimicrobial therapy on outcome. Antimicrob Agents Chemother 49:760–766
Tumbarello M, Sanguinetti M, Montuori E, Trecarichi EM, Posteraro B, Fiori B, Citton R, D’Inzeo T, Fadda G, Cauda R, Spanu T (2007) Predictors of mortality in patients with bloodstream infections caused by extended-spectrum-beta-lactamase-producing Enterobacteriaceae: importance of inadequate initial antimicrobial treatment. Antimicrob Agents Chemother 51:1987–1994
Suppli M, Aabenhus R, Harboe ZB, Andersen LP, Tvede M, Jensen JU (2011) Mortality in enterococcal bloodstream infections increases with inappropriate antimicrobial therapy. Clin Microbiol Infect 17(7):1078–1083
Kahvecioglu D, Ramiah K, McMaughan D, Garfinkel S, McSorley VE, Nguyen QN, Yang M, Pugliese C, Mehr D, Phillips CD (2014) Multidrug-resistant organism infections in US nursing homes: a national study of prevalence, onset, and transmission across care settings, October 1, 2010–December 31, 2011. Infect Control Hosp Epidemiol 35:S48–S55
Sundvall PD, Stuart B, Davis M, Roderick P, Moore M (2015) Antibiotic use in the care home setting: a retrospective cohort study analysing routine data. BMC Geriatr 15:71
Van Aken S, Lund N, Ahl J, Odenholt I, Tham J (2014) Risk factors, outcome and impact of empirical antimicrobial treatment in extended-spectrum β-lactamase-producing Escherichia coli bacteraemia. Scand J Infect Dis 46(11):753–762
Denis B, Lafaurie M, Donay JL, Fontaine JP, Oksenhendler E, Raffoux E, Hennequin C, Allez M, Socie G, Maziers N, Porcher R, Molina JM (2015) Prevalence, risk factors, and impact on clinical outcome of extended-spectrum beta-lactamase-producing Escherichia coli bacteraemia: a five-year study. Int J Infect Dis 39:1–6
Nguyen ML, Toye B, Kanji S, Zvonar R (2014) Risk factors for and outcomes of bacteremia caused by extended-spectrum β-lactamase-producing Escherichia coli and Klebsiella species at a Canadian tertiary care hospital. Can J Hosp Pharm 68(2):136–143
Freeman JT, McBride SJ, Nisbet MS, Gamble GD, Williamson DA, Taylor SL, Holland DJ (2012) Bloodstream infection with extended-spectrum beta-lactamase-producing Enterobacteriaceae at a tertiary care hospital in New Zealand: risk factors and outcomes. Int J Infect Dis 16(5):e371–e374
Nasa P, Juneja D, Singh O, Dang R, Singh A (2012) An observational study on bloodstream extended-spectrum beta-lactamase infection in critical care unit: incidence, risk factors and its impact on outcome. Eur J Intern Med 23(2):192–195
Kariv G, Paul M, Shani V, Muchtar E, Leibovici L (2013) Benchmarking inappropriate empirical antibiotic treatment. Clin Microbiol Infect 19(7):629–633
Dyar OJ, Pagani L, Pulcini C (2015) Strategies and challenges of antimicrobial stewardship in long-term care facilities. Clin Microbiol Infect 21(1):10–19
Paul M, Nielsen AD, Goldberg E, Andreassen S, Tacconelli E, Almanasreh N, Frank U, Cauda R, Leibovici L; TREAT Study Group (2007) Prediction of specific pathogens in patients with sepsis: evaluation of TREAT, a computerized decision support system. J Antimicrob Chemother 59(6):1204–1207
Paul M, Andreassen S, Tacconelli E, Nielsen AD, Almanasreh N, Frank U, Cauda R, Leibovici L; TREAT Study Group (2006) Improving empirical antibiotic treatment using TREAT, a computerized decision support system: cluster randomized trial. J Antimicrob Chemother 58(6):1238–1245
Acknowledgements
LL and MP are active members of the European Society of Clinical Microbiology and Infectious Diseases—Study Group for Infections in the Elderly (ESGIE) and acknowledge the ESGIE’s contribution to the conception of this study.
Funding
This work was supported by ‘The Israel National Institute for Health Policy Research’.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Daitch, V., Akayzen, Y., Abu-Ghanem, Y. et al. Secular trends in the appropriateness of empirical antibiotic treatment in patients with bacteremia: a comparison between three prospective cohorts. Eur J Clin Microbiol Infect Dis 37, 455–462 (2018). https://doi.org/10.1007/s10096-018-3190-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3190-1