Abstract
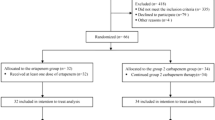
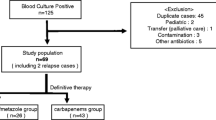
The efficacy of empirical non-carbapenem antibiotics for extended-spectrum beta-lactamase-producing Enterobacteriaceae bacteremia (ESBL-B) is still inconclusive. We conducted a multicenter retrospective cohort study to evaluate the efficacy of empirical non-carbapenem antibiotics for treating ESBL-B. Electronic medical records of individuals who were diagnosed with ESBL-B were reviewed between January 2010 and December 2014 at four university hospitals in Korea. Patients were classified into non-carbapenem and carbapenem groups according to the empirical antibiotic regimen. Patients treated with appropriate empirical antibiotics and who subsequently received carbapenems as definitive therapy were included in the analysis. The inverse probability of treatment weights, a statistical method that adjusts baseline statistics by giving weights based on propensity score, was used. During the study period, 232 adequately treated patients with ESBL-B were included in the analysis: 49 patients in the non-carbapenem group and 183 in the carbapenem group. The baseline characteristics and severity of infection were similar after propensity score weighting. The 30-day mortality rates for the two groups were not statistically significantly different (non-carbapenems 6.3% and carbapenems 11.4%; P = 0.42). In a multivariate analysis, empirical treatment with non-carbapenem antibiotics was not associated with 30-day all-cause mortality (HR 1.02, 95% CI 0.99–1.06, P = 0.14). In a subgroup analysis, empirical treatment with piperacillin-tazobactam was also not associated with 30-day all-cause mortality (HR 1.21, 95% CI 0.37–4.00, P = 0.75). Appropriate non-carbapenems were not inferior to carbapenems as initial empirical therapy for ESBL-B.

Similar content being viewed by others
References
Zhanel GG, Wiebe R, Dilay L, Thomson K, Rubinstein E, Hoban DJ, Noreddin AM, Karlowsky JA (2007) Comparative review of the carbapenems. Drugs 67:1027–1052
Rupp ME, Fey PD (2003) Extended spectrum beta-lactamase (ESBL)-producing Enterobacteriaceae: considerations for diagnosis, prevention and drug treatment. Drugs 63:353–365
Canton R, Novais A, Valverde A, Machado E, Peixe L, Baquero F, Coque TM (2008) Prevalence and spread of extended-spectrum beta-lactamase-producing Enterobacteriaceae in Europe. Clin Microbiol Infect 14(Suppl 1):144–153. https://doi.org/10.1111/j.1469-0691.2007.01850.x
Sheng WH, Badal RE, Hsueh PR (2013) Distribution of extended-spectrum beta-lactamases, AmpC beta-lactamases, and carbapenemases among Enterobacteriaceae isolates causing intra-abdominal infections in the Asia-Pacific region: results of the study for monitoring antimicrobial resistance trends (SMART). Antimicrob Agents Chemother 57:2981–2988. https://doi.org/10.1128/aac.00971-12
Pitout JD, Nordmann P, Laupland KB, Poirel L (2005) Emergence of Enterobacteriaceae producing extended-spectrum beta-lactamases (ESBLs) in the community. J Antimicrob Chemother 56:52–59. https://doi.org/10.1093/jac/dki166
Turner PJ (2005) Extended-spectrum beta-lactamases. Clin Infect Dis 41(Suppl 4):S273–S275. https://doi.org/10.1086/430789
Nordmann P, Naas T, Poirel L (2011) Global spread of carbapenemase-producing Enterobacteriaceae. Emerg Infect Dis 17:1791–1798. https://doi.org/10.3201/eid1710.110655
van Duin D, Kaye KS, Neuner EA, Bonomo RA (2013) Carbapenem-resistant Enterobacteriaceae: a review of treatment and outcomes. Diagn Microbiol Infect Dis 75:115–120. https://doi.org/10.1016/j.diagmicrobio.2012.11.009
Lee CS, Doi Y (2014) Therapy of infections due to carbapenem-resistant gram-negative pathogens. Infect Chemother 46:149–164. https://doi.org/10.3947/ic.2014.46.3.149
Falagas ME, Karageorgopoulos DE (2009) Extended-spectrum beta-lactamase-producing organisms. J Hosp Infect 73:345–354. https://doi.org/10.1016/j.jhin.2009.02.021
Gupta N, Limbago BM, Patel JB, Kallen AJ (2011) Carbapenem-resistant Enterobacteriaceae: epidemiology and prevention. Clin Infect Dis 53:60–67. https://doi.org/10.1093/cid/cir202
Peterson LR (2008) Antibiotic policy and prescribing strategies for therapy of extended-spectrum beta-lactamase-producing Enterobacteriaceae: the role of piperacillin-tazobactam. Clin Microbiol Infect 14(Suppl 1):181–184. https://doi.org/10.1111/j.1469-0691.2007.01864.x
Paterson DL, Ko WC, Von Gottberg A, Mohapatra S, Casellas JM, Goossens H, Mulazimoglu L, Trenholme G, Klugman KP, Bonomo RA, Rice LB, Wagener MM, McCormack JG, Yu VL (2004) Antibiotic therapy for Klebsiella Pneumoniae bacteremia: implications of production of extended-spectrum beta-lactamases. Clin Infect Dis 39:31–37. https://doi.org/10.1086/420816
Chaubey VP, Pitout JD, Dalton B, Ross T, Church DL, Gregson DB, Laupland KB (2010) Clinical outcome of empiric antimicrobial therapy of bacteremia due to extended-spectrum beta-lactamase producing Escherichia coli and Klebsiella pneumoniae. BMC Res Notes 3:116. https://doi.org/10.1186/1756-0500-3-116
Ofer-Friedman H, Shefler C, Sharma S, Tirosh A, Tal-Jasper R, Kandipalli D, Sharma S, Bathina P, Kaplansky T, Maskit M, Azouri T, Lazarovitch T, Zaidenstein R, Kaye KS, Marchaim D (2015) Carbapenems versus piperacillin-Tazobactam for bloodstream infections of nonurinary source caused by extended-spectrum Beta-lactamase-producing Enterobacteriaceae. Infect Control Hosp Epidemiol 36:981–985. https://doi.org/10.1017/ice.2015.101
Tsai HY, Chen YH, Tang HJ, Huang CC, Liao CH, Chu FY, Chuang YC, Sheng WH, Ko WC, Hsueh PR (2014) Carbapenems and piperacillin/tazobactam for the treatment of bacteremia caused by extended-spectrum beta-lactamase-producing Proteus mirabilis. Diagn Microbiol Infect Dis 80:222–226. https://doi.org/10.1016/j.diagmicrobio.2014.07.006
Ng TM, Khong WX, Harris PN, De PP, Chow A, Tambyah PA, Lye DC (2016) Empiric piperacillin-Tazobactam versus carbapenems in the treatment of Bacteraemia due to extended-spectrum beta-lactamase-producing Enterobacteriaceae. PLoS One 11:e0153696. https://doi.org/10.1371/journal.pone.0153696
Kang CI, Park SY, Chung DR, Peck KR, Song JH (2012) Piperacillin-tazobactam as an initial empirical therapy of bacteremia caused by extended-spectrum beta-lactamase-producing Escherichia Coli and Klebsiella Pneumoniae. J Inf Secur 64:533–534. https://doi.org/10.1016/j.jinf.2012.01.008
Rodriguez-Bano J, Navarro MD, Retamar P, Picon E, Pascual A (2012) Beta-lactam/beta-lactam inhibitor combinations for the treatment of bacteremia due to extended-spectrum beta-lactamase-producing Escherichia Coli: a post hoc analysis of prospective cohorts. Clin Infect Dis 54:167–174. https://doi.org/10.1093/cid/cir790
To KK, Lo WU, Chan JF, Tse H, Cheng VC, Ho PL (2013) Clinical outcome of extended-spectrum beta-lactamase-producing Escherichia coli bacteremia in an area with high endemicity. Int J Infect Dis 17:e120–e124. https://doi.org/10.1016/j.ijid.2012.09.008
Kang CI, Kim SH, Park WB, Lee KD, Kim HB, Kim EC, Oh MD, Choe KW (2004) Bloodstream infections due to extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae: risk factors for mortality and treatment outcome, with special emphasis on antimicrobial therapy. Antimicrob Agents Chemother 48:4574–4581. https://doi.org/10.1128/aac.48.12.4574-4581.2004
Vardakas KZ, Tansarli GS, Rafailidis PI, Falagas ME (2012) Carbapenems versus alternative antibiotics for the treatment of bacteraemia due to Enterobacteriaceae producing extended-spectrum beta-lactamases: a systematic review and meta-analysis. J Antimicrob Chemother 67:2793–2803. https://doi.org/10.1093/jac/dks301
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, Lamm W, Clark C, MacFarquhar J, Walton AL, Reller LB, Sexton DJ (2002) Health care-associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med 137:791–797
Mathers AJ, Peirano G, Pitout JD (2015) The role of epidemic resistance plasmids and international high-risk clones in the spread of multidrug-resistant Enterobacteriaceae. Clin Microbiol Rev 28:565–591. https://doi.org/10.1128/cmr.00116-14
Kwon JC, Kim SH, Choi JK, Cho SY, Park YJ, Park SH, Choi SM, Lee DG, Choi JH, Yoo JH (2013) Epidemiology and clinical features of bloodstream infections in hematology wards: one year experience at the catholic blood and marrow transplantation center. Infect Chemother 45:51–61. https://doi.org/10.3947/ic.2013.45.1.51
Reuland EA, Al Naiemi N, Kaiser AM, Heck M, Kluytmans JA, Savelkoul PH, Elders PJ, Vandenbroucke-Grauls CM (2016) Prevalence and risk factors for carriage of ESBL-producing Enterobacteriaceae in Amsterdam. J Antimicrob Chemother 71:1076–1082. https://doi.org/10.1093/jac/dkv441
Hawkey PM (2008) Prevalence and clonality of extended-spectrum beta-lactamases in Asia. Clin Microbiol Infect 14(Suppl 1):159–165. https://doi.org/10.1111/j.1469-0691.2007.01855.x
Kang CI, Wi YM, Ko KS, Chung DR, Peck KR, Lee NY, Song JH (2013) Outcomes and risk factors for mortality in community-onset bacteremia caused by extended-spectrum beta-lactamase-producing Escherichia Coli, with a special emphasis on antimicrobial therapy. Scand J Infect Dis 45:519–525. https://doi.org/10.3109/00365548.2013.775479
Rottier WC, Ammerlaan HS, Bonten MJ (2012) Effects of confounders and intermediates on the association of bacteraemia caused by extended-spectrum beta-lactamase-producing Enterobacteriaceae and patient outcome: a meta-analysis. J Antimicrob Chemother 67:1311–1320. https://doi.org/10.1093/jac/dks065
Qureshi ZA, Paterson DL, Peleg AY, Adams-Haduch JM, Shutt KA, Pakstis DL, Sordillo E, Polsky B, Sandkovsky G, Bhussar MK, Doi Y (2012) Clinical characteristics of bacteraemia caused by extended-spectrum beta-lactamase-producing Enterobacteriaceae in the era of CTX-M-type and KPC-type beta-lactamases. Clin Microbiol Infect 18:887–893. https://doi.org/10.1111/j.1469-0691.2011.03658.x
Tamma PD, Han JH, Rock C, Harris AD, Lautenbach E, Hsu AJ, Avdic E, Cosgrove SE (2015) Carbapenem therapy is associated with improved survival compared with piperacillin-tazobactam for patients with extended-spectrum beta-lactamase bacteremia. Clin Infect Dis 60:1319–1325. https://doi.org/10.1093/cid/civ003
Costa Ramos JM, Stein C, Pfeifer Y, Brandt C, Pletz MW, Makarewicz O (2015) Mutagenesis of the CTX-M-type ESBL-is MIC-guided treatment according to the new EUCAST recommendations a safe approach? J Antimicrob Chemother 70:2528–2535. https://doi.org/10.1093/jac/dkv153
Funding
This study was funded by the National Evidence-based Healthcare Collaborating Agency (NECA; project number NA2015–001).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
None of the authors have any conflicts of interest to report.
Ethical approval
This study was approved by the Institutional Review Board of the National Evidence-based Healthcare Collaborating Agency (NECA) and each hospital.
Informed consent
As a retrospective study, the Institutional Review Board waived informed consent in the present study.
Electronic supplementary material
ESM 1
(DOCX 52 kb)
Rights and permissions
About this article
Cite this article
Ko, JH., Lee, N.R., Joo, EJ. et al. Appropriate non-carbapenems are not inferior to carbapenems as initial empirical therapy for bacteremia caused by extended-spectrum beta-lactamase-producing Enterobacteriaceae: a propensity score weighted multicenter cohort study. Eur J Clin Microbiol Infect Dis 37, 305–311 (2018). https://doi.org/10.1007/s10096-017-3133-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-017-3133-2