Abstract
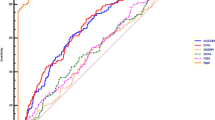
The prognostic impact of thrombocytopaenia in Staphylococcus aureus bacteraemia (SAB) has previously been determined at bacteraemia onset only and relevant pre-bacteraemic thrombocytopaenia predisposing parameters have not been accounted for. We evaluated the prognostic impact of low thrombocyte count in SAB excluding pre-bacteraemic factors potentially causing thrombocytopaenia. This was a multicentre retrospective analysis of methicillin-sensitive SAB (MS-SAB) patients. Thrombocyte count was determined at blood culture collection and at days 3 and 7. Thrombocytopaenia was defined as a thrombocyte count less than 150 ×109/L. Patients with chronic alcoholism, liver diseases and haematologic malignancies were excluded. Altogether, 495 patients were identified. Thrombocytopaenia at blood culture and at day 3 associated to endocarditis (p < 0.05 and p < 0.01) and defervescence (p < 0.001 and p < 0.01). Mortality at 90 days was higher for patients with thrombocytopaenia at blood culture collection (26 vs. 16%, p < 0.05), at day 3 (32 vs. 13%, p < 0.01) and at day 7 (50 vs. 14%, p < 0.001). In receiver operating characteristic analyses, thrombocytopaenia predicted a poor outcome at blood culture collection (p < 0.05), at day 3 (p < 0.001) and at day 7 (p < 0.001). When accounting for all prognostic parameters, thrombocytopaenia at day 3 [hazard ratio (HR), 1.83; p = 0.05] demonstrated a trend towards poor outcome, whereas thrombocytopaenia at day 7 (HR, 3.64; p < 0.001) associated to poor outcome. Thrombocytopaenia at blood culture collection was not a prognostic parameter when all prognostic factors were taken into account. However, thrombocytopaenia at day 3 indicated a poor outcome and thrombocytopaenia at day 7 was a significant independent negative prognostic marker that has not been previously reported in SAB.

Similar content being viewed by others
References
Rieg S, Peyerl-Hoffmann G, de With K et al (2009) Mortality of S. aureus bacteremia and infectious diseases specialist consultation—a study of 521 patients in Germany. J Infect 59:232–239
Forsblom E, Ruotsalainen E, Mölkänen T, Ollgren J, Lyytikäinen O, Järvinen A (2011) Predisposing factors, disease progression and outcome in 430 prospectively followed patients of healthcare- and community-associated Staphylococcus aureus bacteraemia. J Hosp Infect 78:102–107
Thwaites GE, Edgeworth JD, Gkrania-Klotsas E et al (2011) Clinical management of Staphylococcus aureus bacteraemia. Lancet Infect Dis 11:208–222
Fowler VG Jr, Olsen MK, Corey GR et al (2003) Clinical identifiers of complicated Staphylococcus aureus bacteremia. Arch Intern Med 163:2066–2072
Chang FY, Peacock JE Jr, Musher DM et al (2003) Staphylococcus aureus bacteremia: recurrence and the impact of antibiotic treatment in a prospective multicenter study. Medicine (Baltimore) 82:333–339
Lodise TP, McKinnon PS, Swiderski L, Rybak MJ (2003) Outcomes analysis of delayed antibiotic treatment for hospital-acquired Staphylococcus aureus bacteremia. Clin Infect Dis 36:1418–1423
Cosgrove SE, Sakoulas G, Perencevich EN, Schwaber MJ, Karchmer AW, Carmeli Y (2003) Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis 36:53–59
Pfaller MA, Jones RN, Doern GV, Sader HS, Kugler KC, Beach ML (1999) Survey of blood stream infections attributable to gram-positive cocci: frequency of occurrence and antimicrobial susceptibility of isolates collected in 1997 in the United States, Canada, and Latin America from the SENTRY Antimicrobial Surveillance Program. SENTRY Participants Group. Diagn Microbiol Infect Dis 33:283–297
Siegman-Igra Y, Reich P, Orni-Wasserlauf R, Schwartz D, Giladi M (2005) The role of vancomycin in the persistence or recurrence of Staphylococcus aureus bacteraemia. Scand J Infect Dis 37:572–578
Kim SH, Kim KH, Kim HB et al (2008) Outcome of vancomycin treatment in patients with methicillin-susceptible Staphylococcus aureus bacteremia. Antimicrob Agents Chemother 52:192–197
Forsblom E, Ruotsalainen E, Ollgren J, Järvinen A (2013) Telephone consultation cannot replace bedside infectious disease consultation in the management of Staphylococcus aureus bacteremia. Clin Infect Dis 56:527–535
Ringberg H, Thorén A, Lilja B (2000) Metastatic complications of Staphylococcus aureus septicemia. To seek is to find. Infection 28:132–136
Pragman AA, Kuskowski MA, Abraham JM, Filice GA (2012) Infectious disease consultation for Staphylococcus aureus bacteremia improves patient management and outcomes. Infect Dis Clin Pract (Baltim Md) 20:261–267
Annane D, Bellissant E, Cavaillon JM (2005) Septic shock. Lancet 365:63–78
Gafter-Gvili A, Mansur N, Bivas A et al (2011) Thrombocytopenia in Staphylococcus aureus bacteremia: risk factors and prognostic importance. Mayo Clin Proc 86:389–396
Spika JS, Peterson PK, Wilkinson BJ et al (1982) Role of peptidoglycan from Staphylococcus aureus in leukopenia, thrombocytopenia, and complement activation associated with bacteremia. J Infect Dis 146:227–234
Fitzgerald JR, Foster TJ, Cox D (2006) The interaction of bacterial pathogens with platelets. Nat Rev Microbiol 4:445–457
de Haas CJ, Weeterings C, Vughs MM, de Groot PG, Van Strijp JA, Lisman T (2009) Staphylococcal superantigen-like 5 activates platelets and supports platelet adhesion under flow conditions, which involves glycoprotein Ibalpha and alpha IIb beta 3. J Thromb Haemost 7:1867–1874
Kerrigan SW, Clarke N, Loughman A, Meade G, Foster TJ, Cox D (2008) Molecular basis for Staphylococcus aureus-mediated platelet aggregate formation under arterial shear in vitro. Arterioscler Thromb Vasc Biol 28:335–340
George NP, Konstantopoulos K, Ross JM (2007) Differential kinetics and molecular recognition mechanisms involved in early versus late growth phase Staphylococcus aureus cell binding to platelet layers under physiological shear conditions. J Infect Dis 196:639–646
Buyukasýk NS, Ileri M, Alper A et al (2004) Increased blood coagulation and platelet activation in patients with infective endocarditis and embolic events. Clin Cardiol 27:154–158
Hart RG, Foster JW, Luther MF, Kanter MC (1990) Stroke in infective endocarditis. Stroke 21:695–700
Wang JL, Chen SY, Wang JT et al (2008) Comparison of both clinical features and mortality risk associated with bacteremia due to community-acquired methicillin-resistant Staphylococcus aureus and methicillin-susceptible S. aureus. Clin Infect Dis 46:799–806
Wang JT, Wu HS, Weng CM, Hsu LY, Wang FD (2013) Prognosis of patients with methicillin-resistant Staphylococcus aureus bloodstream infection treated with teicoplanin: a retrospective cohort study investigating effect of teicoplanin minimum inhibitory concentrations. BMC Infect Dis 13:182
Wang JT, Hsu LY, Lauderdale TL, Fan WC, Wang FD (2015) Comparison of outcomes among adult patients with Nosocomial bacteremia caused by methicillin-susceptible and methicillin-resistant Staphylococcus aureus: a retrospective cohort study. PLoS One 10(12):e0144710
Paul M, Kariv G, Goldberg E et al (2010) Importance of appropriate empirical antibiotic therapy for methicillin-resistant Staphylococcus aureus bacteraemia. J Antimicrob Chemother 65:2658–2665
Paul M, Zemer-Wassercug N, Talker O et al (2011) Are all beta-lactams similarly effective in the treatment of methicillin-sensitive Staphylococcus aureus bacteraemia? Clin Microbiol Infect 17:1581–1586
Bishara J, Goldberg E, Leibovici L et al (2012) Healthcare-associated vs. hospital-acquired Staphylococcus aureus bacteremia. Int J Infect Dis 16:e457–e463
Ruotsalainen E, Järvinen A, Koivula I et al (2006) Levofloxacin does not decrease mortality in Staphylococcus aureus bacteraemia when added to the standard treatment: a prospective and randomized clinical trial of 381 patients. J Intern Med 259:179–190
Forsblom E, Ruotsalainen E, Järvinen A (2015) Improved outcome with early rifampicin combination treatment in methicillin-sensitive Staphylococcus aureus bacteraemia with a deep infection focus—a retrospective cohort study. PLoS One 10:e0122824
McCabe WR, Jackson GG (1962) Gram-negative bacteremia: I. Etiology and ecology. Arch Intern Med 110:847–855
Levy MM, Fink MP, Marshall JC et al (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 31:1250–1256
Li JS, Sexton DJ, Mick N et al (2000) Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 30:633–638
Levi M, Toh CH, Thachil J, Watson HG (2009) Guidelines for the diagnosis and management of disseminated intravascular coagulation. British Committee for Standards in Haematology. Br J Haematol 145:24–33
Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ (1995) Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med 23:1638–1652
Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL (2001) Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA 286:1754–1758
Peltz S (1991) Severe thrombocytopenia secondary to alcohol use. Postgrad Med 89:75–76
Akca S, Haji-Michael P, de Mendonça A, Suter P, Levi M, Vincent JL (2002) Time course of platelet counts in critically ill patients. Crit Care Med 30:753–756
Sy RW, Chawantanpipat C, Richmond DR, Kritharides L (2008) Thrombocytopenia and mortality in infective endocarditis. J Am Coll Cardiol 51:1824–1825
Nijsten MW, ten Duis HJ, Zijlstra JG et al (2000) Blunted rise in platelet count in critically ill patients is associated with worse outcome. Crit Care Med 28:3843–3846
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics statement
The trial was approved by the institutional review board of Helsinki University Central Hospital and the ethical committee of Helsinki University Central Hospital. A written informed consent was provided by each patient.
Funding
The study has been supported by grants from the Medical Society of Finland and the foundations Dorothea Olivia, Karl Walter och Jarl Walter Perkléns minne and Svenska Kulturfonden. The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
Additional information
E. Forsblom and I. Tielinen contributed equally to this work.
Rights and permissions
About this article
Cite this article
Forsblom, E., Tielinen, I., Ruotsalainen, E. et al. Thrombocytopaenia during methicillin-sensitive Staphylococcus aureus bacteraemia. Eur J Clin Microbiol Infect Dis 36, 887–896 (2017). https://doi.org/10.1007/s10096-016-2877-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-016-2877-4