Abstract
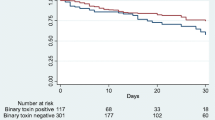
Binary toxin-producing Clostridium difficile strains such as ribotypes 027 and 078 have been associated with increased Clostridium difficile infection (CDI) severity. Our objective was to investigate the association between presence of the binary toxin gene and CDI severity and recurrence. We performed a laboratory-based retrospective study including patients between January 2013 and March 2015 whose fecal samples were analyzed by polymerase chain reaction (PCR) for the presence of the genes for toxin B and binary toxin and a deletion in the tcdC gene, specific for ribotype 027. Clinical and epidemiological characteristics were compared between 33 binary toxin-positive CDI patients and 33 binary toxin-negative CDI patients. Subsequently, the characteristics of 66 CDI patients were compared to those of 66 diarrhea patients who were carriers of non-toxigenic C. difficile strains. Fifty-nine of 1034 (5.7 %) fecal samples analyzed by PCR were binary toxin-positive, belonging to 33 different patients. No samples were positive for ribotype 027. Binary toxin-positive CDI patients did not differ from binary toxin-negative CDI patients in terms of disease recurrence, morbidity, or mortality, except for a higher peripheral leukocytosis in the binary toxin-positive group (16.30 × 109/L vs. 11.65 × 109/L; p = 0.02). The second part of our study showed that CDI patients had more severe disease, but not a higher 30-day mortality rate than diarrhea patients with a non-toxicogenic C. difficile strain. In our setting with a low prevalence of ribotype 027, the presence of the binary toxin gene is not associated with poor outcome.
Similar content being viewed by others
References
Bartlett JG (2006) Narrative review: the new epidemic of Clostridium difficile-associated enteric disease. Ann Intern Med 145:758–764
Bartlett JG, Moon N, Chang TW et al (1978) Role of Clostridium difficile in antibiotic-associated pseudomembranous colitis. Gastroenterology 75:778–782
Thomas C, Stevenson M, Riley TV (2003) Antibiotics and hospital-acquired Clostridium difficile-associated diarrhoea: a systematic review. J Antimicrob Chemother 51:1339–1350
Loo VG, Bourgault AM, Poirier L et al (2011) Host and pathogen factors for Clostridium difficile infection and colonization. N Engl J Med 365:1693–1703
Healthcare Commission (2006) Investigation into outbreaks of Clostridium difficile at Stoke Mandeville Hospital, Buckinghamshire Hospitals NHS Trust. Healthcare Commission, London. Available online at: http://www.buckshealthcare.nhs.uk/Downloads/healthcarecommision/HCC-Investigation-into-the-Outbreak-of-Clostridium-Difficile.pdf. Accessed 03 Feb 2015
Kuijper EJ, Barbut F, Brazier JS et al (2008) Update of Clostridium difficile infection due to PCR ribotype 027 in Europe, 2008. Euro Surveill 13. pii: 18942
Neely F, Catry B, Lambert M-L (2014) Epidemiology of Clostridium difficile infection in Belgium: report 2014. Wetenschappelijk Instituut Volksgezondheid (WIV), Brussels. Available online at: http://www.nsih.be/download/CDIF/CDIF-AR-2014-EN.pdf. Accessed 03 Feb 2015
Hensgens MP, Goorhuis A, Notermans DW et al (2009) Decrease of hypervirulent Clostridium difficile PCR ribotype 027 in the Netherlands. Euro Surveill 14. pii: 19402
van Dorp SM, Harmanus C, Sanders IM et al (2014) Eighth Annual Report of the National Reference Laboratory for Clostridium difficile and results of the sentinel surveillance: May 2013–May 2014. Center for Infectious Diseases Control (CIb), Bilthoven. Available online at: http://www.rivm.nl/Documenten_en_publicaties/Algemeen_Actueel/Uitgaven/Infectieziekten/CDiffNL/Eighth_Annual_Report_of_the_National_Reference_Laboratory_for_Clostridium_difficile_and_results_of_the_sentinel_surveillance. Accessed 09 May 2015
Cloud J, Noddin L, Pressman A et al (2009) Clostridium difficile strain NAP-1 is not associated with severe disease in a nonepidemic setting. Clin Gastroenterol Hepatol 7:868–873.e2
Walk ST, Micic D, Jain R et al (2012) Clostridium difficile ribotype does not predict severe infection. Clin Infect Dis 55:1661–1668
Carter GP, Rood JI, Lyras D (2012) The role of toxin A and toxin B in the virulence of Clostridium difficile. Trends Microbiol 20:21–29
Murray R, Boyd D, Levett PN et al (2009) Truncation in the tcdC region of the Clostridium difficile PathLoc of clinical isolates does not predict increased biological activity of Toxin B or Toxin A. BMC Infect Dis 9:103
Cartman ST, Kelly ML, Heeg D et al (2012) Precise manipulation of the Clostridium difficile chromosome reveals a lack of association between the tcdC genotype and toxin production. Appl Environ Microbiol 78:4683–4690
Verdoorn BP, Orenstein R, Rosenblatt JE (2010) High prevalence of tcdC deletion-carrying Clostridium difficile and lack of association with disease severity. Diagn Microbiol Infect Dis 66:24–28
Gerding DN, Johnson S, Rupnik M et al (2014) Clostridium difficile binary toxin CDT: mechanism, epidemiology, and potential clinical importance. Gut Microbes 5:15–27
Stewart DB, Berg A, Hegarty J (2013) Predicting recurrence of C. difficile colitis using bacterial virulence factors: binary toxin is the key. J Gastrointest Surg 17:118–124
Bacci S, Mølbak K, Kjeldsen MK et al (2011) Binary toxin and death after Clostridium difficile infection. Emerg Infect Dis 17:976–982
Goldenberg SD, French GL (2011) Lack of association of tcdC type and binary toxin status with disease severity and outcome in toxigenic Clostridium difficile. J Infect 62:355–362
Barbut F, Rupnik M (2012) Editorial commentary: 027, 078, and others: going beyond the numbers (and away from the hypervirulence). Clin Infect Dis 55:1669–1672
Reigadas E, Alcalá L, Marín M et al (2016) Role of binary toxin in the outcome of Clostridium difficile infection in a non-027 ribotype setting. Epidemiol Infect 144:268–273
Peach SL, Borriello SP, Gaya H et al (1986) Asymptomatic carriage of Clostridium difficile in patients with cystic fibrosis. J Clin Pathol 39:1013–1018
Welkon CJ, Long SS, Thompson CM Jr et al (1985) Clostridium difficile in patients with cystic fibrosis. Am J Dis Child 139:805–808
Yahav J, Samra Z, Blau H et al (2006) Helicobacter pylori and Clostridium difficile in cystic fibrosis patients. Dig Dis Sci 51:2274–2279
Bauer MP, Farid A, Bakker M et al (2014) Patients with cystic fibrosis have a high carriage rate of non-toxigenic Clostridium difficile. Clin Microbiol Infect 20:O446–O449
Shetty N, Wren MW, Coen PG (2011) The role of glutamate dehydrogenase for the detection of Clostridium difficile in faecal samples: a meta-analysis. J Hosp Infect 77:1–6
Alasmari F, Seiler SM, Hink T et al (2014) Prevalence and risk factors for asymptomatic Clostridium difficile carriage. Clin Infect Dis 59:216–222
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval for this study was obtained by the Ethics Committee of UH Leuven.
Informed consent
For this type of observational and retrospective study, informed consent is not required.
Rights and permissions
About this article
Cite this article
Pilate, T., Verhaegen, J., Van Ranst, M. et al. Binary toxin and its clinical importance in Clostridium difficile infection, Belgium. Eur J Clin Microbiol Infect Dis 35, 1741–1747 (2016). https://doi.org/10.1007/s10096-016-2719-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-016-2719-4