Abstract
Procalcitonin (PCT)-guided antibiotic stewardship is a successful strategy to decrease antibiotic use. We assessed if clinical judgement affected compliance with a PCT-algorithm for antibiotic prescribing in a multicenter surveillance of patients with lower respiratory tract infections (LRTI).
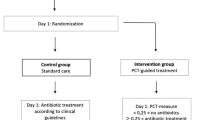
Initiation and duration of antibiotic therapy, adherence to a PCT algorithm and outcome were monitored in consecutive adults with LRTI who were enrolled in a prospective observational quality control. We correlated initial clinical judgment of the treating physician with algorithm compliance and assessed the influence of PCT on the final decision to initiate antibiotic therapy.
PCT levels correlated with physicians’ estimates of the likelihood of bacterial infection (p for trend <0.02). PCT influenced the post-test probability of antibiotic initiation with a greater effect in patients with non-pneumonia LRTI (e.g., for bronchitis: −23 % if PCT ≤ 0.25 μg/L and +31 % if PCT > 0.25 μg/L), in European centers (e.g., in France −22 % if PCT ≤ 0.25 μg/L and +13 % if PCT > 0.25 μg/L) and in centers, which had previous experience with the PCT-algorithm (−16 % if PCT ≤ 0.25 μg/L and +19 % if PCT > 0.25 μg/L). Algorithm non-compliance, i.e. antibiotic prescribing despite low PCT-levels, was independently predicted by the likelihood of a bacterial infection as judged by the treating physician. Compliance was significantly associated with identification of a bacterial etiology (p = 0.01).
Compliance with PCT-guided antibiotic stewardship was affected by geographically and culturally-influenced subjective clinical judgment. Initiation of antibiotic therapy was altered by PCT levels. Differential compliance with antibiotic stewardship efforts contributes to geographical differences in antibiotic prescribing habits and potentially influences antibiotic resistance rates.




Similar content being viewed by others
References
Grill MF, Maganti RK (2011) Neurotoxic effects associated with antibiotic use: management considerations. BJCP 72(3):381–93
Stewardson AJ, Huttner B, Harbarth S (2011) At least it won’t hurt: the personal risks of antibiotic exposure. Curr Opin Pharmacol 11(5):446–52
Stevens V, Dumyati G, Fine LS, Fisher SG, van Wijngaarden E (2011) Cumulative antibiotic exposures over time and the risk of Clostridium difficile infection. CID 53(1):42–8
Harbarth S, Emonet S (2006) Navigating the World Wide Web in search of resources on antimicrobial resistance. CID 43(1):72–8
Van de Sande-Bruinsma N, Grundmann H, Verloo D, Tiemersma E, Monen J, Goossens H et al (2008) Antimicrobial drug use and resistance in Europe. EID 14(11):1722–30
Albrich WC, Monnet DL, Harbarth S (2004) Antibiotic selection pressure and resistance in Streptococcus pneumoniae and Streptococcus pyogenes. EID 10(3):514–517
Dagan R, Barkai G, Givon-Lavi N, Sharf AZ, Vardy D, Cohen T et al (2008) Seasonality of antibiotic-resistant streptococcus pneumoniae that causes acute otitis media: a clue for an antibiotic-restriction policy? JID 197(8):1094–1102
Nasrin D, Collignon PJ, Roberts L, Wilson EJ, Pilotto LS, Douglas RM (2002) Effect of beta lactam antibiotic use in children on pneumococcal resistance to penicillin: prospective cohort study. BMJ 324(7328):28–30
Carmeli Y, Troillet N, Karchmer AW, Samore MH (1999) Health and economic outcomes of antibiotic resistance in Pseudomonas aeruginosa. Arch Int Med 159(10):1127–1132
Cosgrove SE, Carmeli Y (2003) The impact of antimicrobial resistance on health and economic outcomes. CID 36(11):1433–1437
Cosgrove SE (2006) The relationship between antimicrobial resistance and patient outcomes: mortality, length of hospital stay, and health care costs. CID 42(Suppl 2):S82–89
Spellberg B (2011) The antibiotic crisis: can we reverse 65 years of failed stewardship? Arch Int Med 171(12):1080–1081
Cars O, Molstad S, Melander A (2001) Variation in antibiotic use in the European Union. Lancet 357(9271):1851–1853
Harbarth S, Albrich W, Goldmann DA, Huebner J (2001) Control of multiply resistant cocci: do international comparisons help? Lancet Infect Dis 1(4):251–261
Finch RG, Metlay JP, Davey PG, Baker LJ, International Forum on Antibiotic Resistance (2002) Educational interventions to improve antibiotic use in the community: report from the International Forum on Antibiotic Resistance (IFAR) colloquium, 2002. Lancet Infect Dis 4(1):44–53
Hulscher ME, Grol RP, van der Meer JW (2010) Antibiotic prescribing in hospitals: a social and behavioural scientific approach. Lancet Infect Dis 10(3):167–175
Harbarth S, Albrich W, Brun-Buisson C (2002) Outpatient antibiotic use and prevalence of antibiotic-resistant pneumococci in France and Germany: a sociocultural perspective. EID 8(12):1460–1467
Filippini M, Masiero G, Moschetti K (2006) Socioeconomic determinants of regional differences in outpatient antibiotic consumption: evidence from Switzerland. Healthpol 78(1):77–92
Christ-Crain M, Jaccard-Stolz D, Bingisser R, Gencay MM, Huber PR, Tamm M et al (2004) Effect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster-randomised, single-blinded intervention trial. Lancet 363(9409)
Christ-Crain M, Stolz D, Bingisser R, Muller C, Miedinger D, Huber PR et al (2006) Procalcitonin guidance of antibiotic therapy in community-acquired pneumonia: a randomized trial. AJRCCM 174(1):84–93
Schuetz P, Christ-Crain M, Thomann R, Falconnier C, Wolbers M, Widmer I et al (2009) Effect of procalcitonin-based guidelines vs standard guidelines on antibiotic use in lower respiratory tract infections: the ProHOSP randomized controlled trial. JAMA 302(10):1059–1066
Bouadma L, Luyt CE, Tubach F, Cracco C, Alvarez A, Schwebel C et al (2010) Use of procalcitonin to reduce patients’ exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised controlled trial. Lancet 375(9713):463–474
Schuetz P, Batschwaroff M, Dusemund F, Albrich W, Burgi U, Maurer M et al (2010) Effectiveness of a procalcitonin algorithm to guide antibiotic therapy in respiratory tract infections outside of study conditions: a post-study survey. EJCMID 29(3):269–277
Schuetz P, Albrich W, Christ-Crain M, Chastre J, Mueller B (2010) Procalcitonin for guidance of antibiotic therapy. Expert Rev Anti Infect Ther 8(5):575–587
Albrich WC, Dusemund F, Bucher B, Meyer S, Thomann R, Kuehn F, Bassetti S, Sprenger M, Bachli E, Sigrist T, Schwietert M, Amin D, Hausfater P, Carre E, Gaillat J, Schuetz P, Regez K, Bossart R, Schild U, Mueller B (2012) Effectiveness and safety of procalcitonin-guided antibiotic therapy in lower respiratory tract infections in “real life” - an international, multicenter poststudy survey (ProREAL). Arch Int Med 172(9):715–722
Schuetz P, Christ-Crain M, Wolbers M, Schild U, Thomann R, Falconnier C et al (2007) Procalcitonin guided antibiotic therapy and hospitalization in patients with lower respiratory tract infections: a prospective, multicenter, randomized controlled trial. BMC Health Serv Res 7:102
Fischer JE, Harbarth S, Agthe AG, Benn A, Ringer SA, Goldmann DA et al (2004) Quantifying uncertainty: physicians’ estimates of infection in critically ill neonates and children. CID 38(10):1383–1390
Bartlett JG (2011) Diagnostic tests for agents of community-acquired pneumonia. CID 52(S4):296–304
Schwartz A (2011) Medical decision making and medical education: challenges and opportunities. Perspect Biol Med 54(1):68–74
Gonzales R, Sande MA (2000) Uncomplicated acute bronchitis. Ann Int Med 133(12):981–991
Gonzales R, Steiner JF, Sande MA (1997) Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA 278(11):901–904
Wenzel RP, Fowler AA (2006) Clinical practice. Acute bronchitis. N Engl J Med 355(20):2125–2130
Sabuncu E, David J, Bernede-Bauduin C, Pepin S, Leroy M, Boelle PY et al (2009) Significant reduction of antibiotic use in the community after a nationwide campaign in France, 2002–2007. PLoS Medicine 6(6):e1000084
Huttner B, Goossens H, Verheij T et al (2010) Characteristics and outcomes of public campaigns aimed at improving the use of antibiotics in outpatients in high-income countries. The Lancet ID 10(1):17–31
Aujesky D, McCausland JB, Whittle J, Obrosky DS, Yealy DM, Fine MJ (2009) Reasons why emergency department providers do not rely on the pneumonia severity index to determine the initial site of treatment for patients with pneumonia. CID 49(10):e100–108
Grol R, Grimshaw J (1999) Evidence-based implementation of evidence-based medicine. Joint Comm J Qual Im 25(10):503–513
Hannes K, Leys M, Vermeire E, Aertgeerts B, Buntinx F, Depoorter AM (2005) Implementing evidence-based medicine in general practice: a focus group based study. BMC Fam Pract 6:37
Kitto S, Petrovic A, Gruen RL, Smith JA (2011) Evidence-based medicine training and implementation in surgery: the role of surgical cultures. JECP 17(4):819
Haspel RL (2010) Implementation and assessment of a resident curriculum in evidence-based transfusion medicine. Arch Pathol Lab Med 134(7):1054–1059
Acknowledgement
We are grateful to all of the patients, physicians and nursing staff from the centers who participated in this survey.
Conflict of Interest
Drs Albrich, Schuetz, and Mueller have received support from BRAHMS AG to attend meetings and fulfill speaking engagements. Dr Amin has received speaking honoraria from bioMérieux. Drs Albrich and Mueller have received support from bioMérieux to attend meetings. Dr Mueller has served as a consultant to and received research support from BRAHMS AG and bioMérieux.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
F. Dusemund, B. Bucher and S. Meyer are equally contributing first authors. B. Müller and W. C. Albrich are equally contributing senior authors.
Rights and permissions
About this article
Cite this article
Dusemund, F., Bucher, B., Meyer, S. et al. Influence of procalcitonin on decision to start antibiotic treatment in patients with a lower respiratory tract infection: insight from the observational multicentric ProREAL surveillance. Eur J Clin Microbiol Infect Dis 32, 51–60 (2013). https://doi.org/10.1007/s10096-012-1713-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-012-1713-8