Abstract
The clinical utility of fluoroquinolones (FQs) for the treatment of Pseudomonas aeruginosa (PA) and other serious Gram-negative infections is currently decreasing due to the rapid emergence of resistance. Because previous studies have shown that efflux is a common mechanism contributing to FQ resistance in PA, one suggested approach to extend the longevity of this class of drugs is combination therapy with an efflux pump inhibitor (EPI). In order to determine the viability of this approach, it is necessary to understand the relative contribution of efflux- vs. target-mediated mechanisms of FQ resistance in the clinic. A set of 26 recent PA clinical isolates were characterized for antibiotic resistance profiles, efflux pump expression, topoisomerase mutations, and FQ susceptibility with and without an EPI. The contribution of OprM to the overall antibiotic resistance was assessed in a subset of these strains. Our results suggest that the co-administration of an EPI with FQs or other antibiotics currently in use would not be sufficient to combat the complexity of resistance mechanisms now present in many clinical isolates.


Similar content being viewed by others
References
Bonomo RA, Szabo D (2006) Mechanisms of multidrug resistance in Acinetobacter species and Pseudomonas aeruginosa. Clin Infect Dis 43:S49–S56
Hancock REW, Speert DP (2000) Antibiotic resistance in Pseudomonas aeruginosa: mechanisms and impact on treatment. Drug Resist Updat 3:247–255
Mesaros N, Nordmann P, Plésiat P et al (2007) Pseudomonas aeruginosa: resistance and therapeutic options at the turn of the new millennium. Clin Microbiol Infect 13:560–578
Rahal JJ (2006) Novel antibiotic combinations against infections with almost completely resistant Pseudomonas aeruginosa and Acinetobacter species. Clin Infect Dis 43:S95–S99
Rice LB (2006) Challenges in identifying new antimicrobial agents effective for treating infections with Acinetobacter baumannii and Pseudomonas aeruginosa. Clin Infect Dis 43:S100–S105
Rossolini GM, Mantengoli E (2005) Treatment and control of severe infections caused by multiresistant Pseudomonas aeruginosa. Clin Microbiol Infect 11(Suppl 4):17–32
Bratu S, Quale J, Cebular S et al (2005) Multidrug-resistant Pseudomonas aeruginosa in Brooklyn, New York: molecular epidemiology and in vitro activity of polymyxin B. Eur J Clin Microbiol Infect Dis 24:196–201
Henrichfreise B, Wiegand I, Pfister W et al (2007) Resistance mechanisms of multiresistant Pseudomonas aeruginosa strains from Germany and correlation with hypermutation. Antimicrob Agents Chemother 51:4062–4070
Obritsch MD, Fish DN, MacLaren R et al (2005) Nosocomial infections due to multidrug-resistant Pseudomonas aeruginosa: epidemiology and treatment options. Pharmacotherapy 25:1353–1364
Polk RE, Johnson CK, McClish D et al (2004) Predicting hospital rates of fluoroquinolone-resistant Pseudomonas aeruginosa from fluoroquinolone use in US hospitals and their surrounding communities. Clin Infect Dis 39:497–503
Mouneimné H, Robert J, Jarlier V et al (1999) Type II topoisomerase mutations in ciprofloxacin-resistant strains of Pseudomonas aeruginosa. Antimicrob Agents Chemother 43:62–66
Wolfson JS, Hooper DC (1989) Bacterial resistance to quinolones: mechanisms and clinical importance. Rev Infect Dis 11:S906–S968
Oh H, Stenhoff J, Jalal S et al (2003) Role of efflux pumps and mutations in genes for topoisomerases II and IV in fluoroquinolone-resistant Pseudomonas aeruginosa strains. Microb Drug Resist 9:323–328
Aeschlimann JR (2003) The role of multidrug efflux pumps in the antibiotic resistance of Pseudomonas aeruginosa and other gram-negative bacteria. Insights from the Society of Infectious Diseases Pharmacists. Pharmacotherapy 23:916–924
Kriengkauykiat J, Porter E, Lomovskaya O et al (2005) Use of an efflux pump inhibitor to determine the prevalence of efflux pump-mediated fluoroquinolone resistance and multidrug resistance in Pseudomonas aeruginosa. Antimicrob Agents Chemother 49:565–570
Köhler T, Michéa-Hamzehpour M, Plésiat P et al (1997) Differential selection of multidrug efflux systems by quinolones in Pseudomonas aeruginosa. Antimicrob Agents Chemother 41:2540–2543
Masuda N, Sakagawa E, Ohya S et al (2000) Substrate specificities of MexAB-OprM, MexCD-OprJ, and MexXY-OprM efflux pumps in Pseudomonas aeruginosa. Antimicrob Agents Chemother 44:3322–3327
Poole K, Gotoh N, Tsujimoto H et al (1996) Overexpression of the mexC-mexD-oprJ efflux operon in nfxB-type multidrug-resistant strains of Pseudomonas aeruginosa. Mol Microbiol 21:713–724
Poole K, Srikumar R (2001) Multidrug efflux in Pseudomonas aeruginosa: components, mechanisms and clinical significance. Curr Top Med Chem 1:59–71
Dumas J-L, van Delden C, Perron K et al (2006) Analysis of antibiotic resistance gene expression in Pseudomonas aeruginosa by quantitative real-time-PCR. FEMS Microbiol Lett 254:217–225
Fukuda H, Hosaka M, Iyobe S et al (1995) NfxC-type quinolone resistance in a clinical isolate of Pseudomonas aeruginosa. Antimicrob Agents Chemother 39:790–792
Higgins PG, Fluit AC, Milatovic D et al (2003) Mutations in GyrA, ParC, MexR and NfxB in clinical isolates of Pseudomonas aeruginosa. Int J Antimicrob Agents 21:409–413
Jalal S, Wretlind B (1998) Mechanisms of quinolone resistance in clinical strains of Pseudomonas aeruginosa. Microb Drug Resist 4:257–261
Sobel ML, Hocquet D, Cao L et al (2005) Mutations in PA3574 (nalD) lead to increased mexab-oprm expression and multidrug resistance in laboratory and clinical isolates of Pseudomonas aeruginosa. Antimicrob Agents Chemother 49:1782–1786
Hocquet D, Roussel-Delvallez M, Cavallo J-D et al (2007) MexAB-OprM- and MexXY-overproducing mutants are very prevalent among clinical strains of Pseudomonas aeruginosa with reduced susceptibility to ticarcillin. Antimicrob Agents Chemother 51:1582–1583
Nakajima A, Sugimoto Y, Yoneyama H et al (2002) High-level fluoroquinolone resistance in Pseudomonas aeruginosa due to interplay of the MexAB-OprM efflux pump and the DNA gyrase mutation. Microbiol Immunol 46:391–395
Amaral L, Pagès J-M (2008) Control and regulation of permeability of MDR bacterial pathogens to antibiotics. Curr Drug Targets 9:718
Barrett JF (2001) MC-207110 Daiichi Seiyaku/Microcide Pharmaceuticals. Curr Opin Investig Drugs 2:212–215
Kaatz GW (2002) Inhibition of bacterial efflux pumps: a new strategy to combat increasing antimicrobial agent resistance. Expert Opin Emerg Drugs 7:223–233
Lomovskaya O, Warren MS, Lee A et al (2001) Identification and characterization of inhibitors of multidrug resistance efflux pumps in Pseudomonas aeruginosa: novel agents for combination therapy. Antimicrob Agents Chemother 45:105–116
Lomovskaya O, Bostian KA (2006) Practical applications and feasibility of efflux pump inhibitors in the clinic—a vision for applied use. Biochem Pharmacol 71:910–918
Lomovskaya O, Zgurskaya HI, Totrov M et al (2007) Waltzing transporters and ‘the dance macabre’ between humans and bacteria. Nat Rev Drug Discov 6:56–65
Griffith D, Lomovskaya O, Lee V et al (2000) Potentiation of levofloxacin by MC-02595, a broad-spectrum efflux pump inhibitor (EPI) in mouse models of infection due to Pseudomonas aeruginosa with combinations of different Mex pump expression and gyrA mutation. In: Interscience Conference on Antimicrobial Agents in Chemotherapy, Toronto, Ontario, Canada, September 2000
Lomovskaya O, Lee A, Hoshino K et al (1999) Use of a genetic approach to evaluate the consequences of inhibition of efflux pumps in Pseudomonas aeruginosa. Antimicrob Agents Chemother 43:1340–1346
Jung R, Fish DN, Obritsch MD et al (2004) Surveillance of multi-drug resistant Pseudomonas aeruginosa in an urban tertiary-care teaching hospital. J Hosp Infect 57:105–111
Pournaras S, Maniati M, Spanakis N et al (2005) Spread of efflux pump-overexpressing, non-metallo-beta-lactamase-producing, meropenem-resistant but ceftazidime-susceptible Pseudomonas aeruginosa in a region with blaVIM endemicity. J Antimicrob Chemother 56:761–764
Yoshida K, Nakayama K, Ohtsuka M et al (2007) MexAB-OprM specific efflux pump inhibitors in Pseudomonas aeruginosa. Part 7: highly soluble and in vivo active quaternary ammonium analogue D13-9001, a potential preclinical candidate. Bioorg Med Chem 15:7087–7097
Stover CK, Pham XQ, Erwin AL et al (2000) Complete genome sequence of Pseudomonas aeruginosa PAO1, an opportunistic pathogen. Nature 406:959–964
Simon R, Priefer U, Pühler A (1983) A broad host range mobilization system for in vivo genetic engineering: transposon mutagenesis in Gram negative bacteria. Biotechnology 1:784–791
Approved Standard M7-A2 (1990) In: Standards. NCfCL, ed. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. NCCLS, Villanova
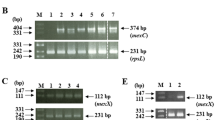
Mesaros N, Glupczynski Y, Avrain L et al (2007) A combined phenotypic and genotypic method for the detection of Mex efflux pumps in Pseudomonas aeruginosa. J Antimicrob Chemother 59:378–386
Okamoto K, Gotoh N, Nishino T (2002) Extrusion of penem antibiotics by multicomponent efflux systems MexAB-OprM, MexCD-OprJ, and MexXY-OprM of Pseudomonas aeruginosa. Antimicrob Agents Chemother 46:2696–2699
Okamoto K, Gotoh N, Nishino T (2002) Alterations of susceptibility of Pseudomonas aeruginosa by overproduction of multidrug efflux systems, MexAB-OprM, MexCD-OprJ, and MexXY/OprM to carbapenems: substrate specificities of the efflux systems. J Infect Chemother 8:371–373
Masuda N, Gotoh N, Ohya S et al (1996) Quantitative correlation between susceptibility and OprJ production in NfxB mutants of Pseudomonas aeruginosa. Antimicrob Agents Chemother 40:909–913
Köhler T, Michéa-Hamzehpour M, Henze U et al (1997) Characterization of MexE-MexF-OprN, a positively regulated multidrug efflux system of Pseudomonas aeruginosa. Mol Microbiol 23:345–354
Wolter DJ, Hanson ND, Lister PD (2005) AmpC and OprD are not involved in the mechanism of imipenem hypersusceptibility among Pseudomonas aeruginosa isolates overexpressing the mexCD-oprJ efflux pump. Antimicrob Agents Chemother 49:4763–4766
Quale J, Bratu S, Gupta J et al (2006) Interplay of efflux system, ampC, and oprD expression in carbapenem resistance of Pseudomonas aeruginosa clinical isolates. Antimicrob Agents Chemother 50:1633–1641
Wolter DJ, Hanson ND, Lister PD (2004) Insertional inactivation of oprD in clinical isolates of Pseudomonas aeruginosa leading to carbapenem resistance. FEMS Microbiol Lett 236:137–143
Akasaka T, Tanaka M, Yamaguchi A et al (2001) Type II topoisomerase mutations in fluoroquinolone-resistant clinical strains of Pseudomonas aeruginosa isolated in 1998 and 1999: role of target enzyme in mechanism of fluoroquinolone resistance. Antimicrob Agents Chemother 45:2263–2268
DeRyke CA, Kuti JL, Nicolau DP (2007) Reevaluation of current susceptibility breakpoints for Gram-negative rods based on pharmacodynamic assessment. Diagn Microbiol Infect Dis 58:337–344
Frei CR, Wiederhold NP, Burgess DS (2008) Antimicrobial breakpoints for Gram-negative aerobic bacteria based on pharmacokinetic-pharmacodynamic models with Monte Carlo simulation. J Antimicrob Chemother 61:621–628
Ball P (2003) Adverse drug reactions: implications for the development of fluoroquinolones. J Antimicrob Chemother 51:21–27
Hocquet D, Nordmann P, El Garch F et al (2006) Involvement of the MexXY-OprM efflux system in emergence of cefepime resistance in clinical strains of Pseudomonas aeruginosa. Antimicrob Agents Chemother 50:1347–1351
Linares JF, López JA, Camafeita E et al (2005) Overexpression of the multidrug efflux pumps MexCD-OprJ and MexEF-OprN is associated with a reduction of type III secretion in Pseudomonas aeruginosa. J Bacteriol 187:1384–1391
Wolter DJ, Smith-Moland E, Goering RV et al (2004) Multidrug resistance associated with mexXY expression in clinical isolates of Pseudomonas aeruginosa from a Texas hospital. Diagn Microbiol Infect Dis 50:43–50
Mueller MR, Hayden MK, Fridkin SK et al (2008) Nosocomial acquisition of Pseudomonas aeruginosa resistant to both ciprofloxacin and imipenem: a risk factor and laboratory analysis. Eur J Clin Microbiol Infect Dis 27:565–570
Adams-Haduch JM, Paterson DL, Sidjabat HE et al (2008) Genetic basis of multidrug resistance in Acinetobacter baumannii clinical isolates at a tertiary medical center in Pennsylvania. Antimicrob Agents Chemother 52:3837–3843
Jones GL, Warren RE, Skidmore SJ et al (2008) Prevalence and distribution of plasmid-mediated quinolone resistance genes in clinical isolates of Escherichia coli lacking extended-spectrum beta-lactamases. J Antimicrob Chemother 62:1245–1251
Shin JH, Jung HJ, Lee JY et al (2008) High rates of plasmid-mediated quinolone resistance QnrB variants among ciprofloxacin-resistant Escherichia coli and Klebsiella pneumoniae from urinary tract infections in Korea. Microb Drug Resist 14:221–226
El Amin N, Giske CG, Jalal S et al (2005) Carbapenem resistance mechanisms in Pseudomonas aeruginosa: alterations of porin OprD and efflux proteins do not fully explain resistance patterns observed in clinical isolates. APMIS 113:187–196
Michéa-Hamzehpour M, Lucain C, Pechere JC (1991) Resistance to pefloxacin in Pseudomonas aeruginosa. Antimicrob Agents Chemother 35:512–518
Huang H, Hancock RE (1993) Genetic definition of the substrate selectivity of outer membrane porin protein OprD of Pseudomonas aeruginosa. J Bacteriol 175:7793–7800
Mahamoud A, Chevalier J, Alibert-Franco S et al (2007) Antibiotic efflux pumps in Gram-negative bacteria: the inhibitor response strategy. J Antimicrob Chemother 59:1223–1229
Hirakata Y, Srikumar R, Poole K et al (2002) Multidrug efflux systems play an important role in the invasiveness of Pseudomonas aeruginosa. J Exp Med 196:109–118
Piddock LJV (2006) Multidrug-resistance efflux pumps—not just for resistance. Nat Rev Micro 4:629–636
Tegos GP, Masago K, Aziz F et al (2008) Inhibitors of bacterial multidrug efflux pumps potentiate antimicrobial photoinactivation. Antimicrob Agents Chemother 52:3202–3209
Schweizer HP (1998) Intrinsic resistance to inhibitors of fatty acid biosynthesis in Pseudomonas aeruginosa is due to efflux: application of a novel technique for generation of unmarked chromosomal mutations for the study of efflux systems. Antimicrob Agents Chemother 42:394–398
Chuanchuen R, Beinlich K, Hoang TT et al (2001) Cross-resistance between triclosan and antibiotics in Pseudomonas aeruginosa is mediated by multidrug efflux pumps: exposure of a susceptible mutant strain to triclosan selects nfxB mutants overexpressing MexCD-OprJ. Antimicrob Agents Chemother 45:428–432
Acknowledgments
We wish to acknowledge Amy Tait-Kamradt for her help with the genomic sequencing and Andrew Tomaras and John Quinn for their critical reading of the manuscript. These studies were conducted at and funded by Pfizer Global Research and Development.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dunham, S.A., McPherson, C.J. & Miller, A.A. The relative contribution of efflux and target gene mutations to fluoroquinolone resistance in recent clinical isolates of Pseudomonas aeruginosa . Eur J Clin Microbiol Infect Dis 29, 279–288 (2010). https://doi.org/10.1007/s10096-009-0852-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-009-0852-z