Abstract
Background
Brain tumor patients undergoing craniotomy are significantly associated with the development of venous thromboembolism (VTE), while the contributing factors remains controversial. Our study aimed to investigate the prevalence and risk factors for VTE in postoperational brain tumor patients.
Methods
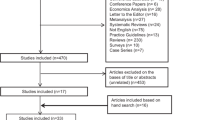
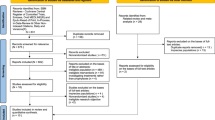
We searched the PubMed, Embase, Web of Science, Medline, and Cochrane Library databases from their inception to July 2023. Article selection, data extraction, and study quality assessment were performed independently by two reviewers. Publication bias was assessed using Egger’s and Begg’s tests. Stata 15.0 software was used for data analysis.
Results
A total of 25 studies were considered, with a total of 49,620 brain tumor individuals. The pooled prevalence of VTE during hospitalization in postoperational brain tumor patients was 9% [95% CI: (0.08, 0.10)]. Moreover, our results demonstrated that patients with VTE were older than those without VTE [mean difference [MD] = 8.14, 95% CI: (4.97, 11.30)]. The following variables were significantly associated with VTE: prior history of VTE [OR = 7.81, 95% CI: (3.62, 16.88)], congestive heart failure [OR = 2.33, 95% CI: (1.08–5.05)], diabetes [OR = 1.87, 95% CI: (1.12–3.10)], hypertension [OR = 1.27, 95% CI: (1.07–1.50)], steroid use [OR = 1.63, 95% CI: (1.41, 1.88)], high white blood cells counts [MD = 0.32, 95% CI: (0.01, 0.63)], and high fibrinogen levels [MD = 0.19, 95% CI: (0.08, 0.30)].
Conclusion
This meta-analysis identified risk factors for postoperational VTE in patients with brain tumor, which can serve as a theoretical foundation for medical staff to manage and treat VTE.
Trial registration
CRD42023357459




Similar content being viewed by others
References
Sauro KM, Soo A, Kramer A, Couillard P, Kromm J, Zygun D, Niven DJ, Bagshaw SM, Stelfox HT (2019) Venous Thromboembolism prophylaxis in neurocritical care patients: are current practices, best practices? Neurocrit Care 30:355–363. https://doi.org/10.1007/s12028-018-0614-9
Semrad TJ, O'Donnell R, Wun T, Chew H, Harvey D, Zhou H, White RH (2007) Epidemiology of venous thromboembolism in 9489 patients with malignant glioma. J Neurosurg 106:601–608. https://doi.org/10.3171/jns.2007.106.4.601
Silvani A, Gaviani P, Lamperti E, Botturi A, Ferrari D, Simonetti G, Fariselli L, Salmaggi A (2011) Metabolic, electrolytes disorders and tromboembolic risk in malignant glioma patients. Neurol Sci Official J Italian Neurol Soc Italian Society Clin Neurophysiol 32(Suppl 2):S229–S231. https://doi.org/10.1007/s10072-011-0793-z
Beckman MG, Hooper WC, Critchley SE, Ortel TL (2010) Venous thromboembolism: a public health concern. Am J Prev Med 38:S495–S501. https://doi.org/10.1016/j.amepre.2009.12.017
Raskob GE, Silverstein R, Bratzler DW, Heit JA, White RH (2010) Surveillance for deep vein thrombosis and pulmonary embolism: recommendations from a national workshop. Am J Prev Med 38:S502–S509. https://doi.org/10.1016/j.amepre.2010.01.010
Rinaldo L, Brown DA, Bhargav AG, Rusheen AE, Naylor RM, Gilder HE, Monie DD, Youssef SJ, Parney IF (2019) Venous thromboembolic events in patients undergoing craniotomy for tumor resection: incidence, predictors, and review of literature. J Neurosurg 132:10–21. https://doi.org/10.3171/2018.7.Jns181175
Turpie AGG, Farjat AE, Haas S, Ageno W, Weitz JI, Goldhaber SZ, Goto S, Angchaisuksiri P, Kayani G, Lopes RD et al (2023) 36-month clinical outcomes of patients with venous thromboembolism: GARFIELD-VTE. Thromb Res 222:31–39. https://doi.org/10.1016/j.thromres.2022.11.016
Sørensen HT, Mellemkjaer L, Olsen JH, Baron JA (2000) Prognosis of cancers associated with venous thromboembolism. N Engl J Med 343:1846–1850. https://doi.org/10.1056/nejm200012213432504
Hoefnagel D, Kwee LE, van Putten EH, Kros JM, Dirven CM, Dammers R (2014) The incidence of postoperative thromboembolic complications following surgical resection of intracranial meningioma. A retrospective study of a large single center patient cohort. Clin Neurol Neurosurg 123:150–154. https://doi.org/10.1016/j.clineuro.2014.06.001
Kim AS, Khorana AA, McCrae KR (2020) Mechanisms and biomarkers of cancer-associated thrombosis. Trans Res J Lab Clin Med 225:33–53. https://doi.org/10.1016/j.trsl.2020.06.012
Smith TR, Nanney AD 3rd, Lall RR, Graham RB, McClendon J Jr, Lall RR, Adel JG, Zakarija A, Cote DJ, Chandler JP (2015) Development of venous thromboembolism (VTE) in patients undergoing surgery for brain tumors: results from a single center over a 10 year period. J Clin Neurosci 22:519–525. https://doi.org/10.1016/j.jocn.2014.10.003
Senders JT, Goldhaber NH, Cote DJ, Muskens IS, Dawood HY, De Vos F, Gormley WB, Smith TR, Broekman MLD (2018) Venous thromboembolism and intracranial hemorrhage after craniotomy for primary malignant brain tumors: a National Surgical Quality Improvement Program analysis. J Neuro-Oncol 136:135–145. https://doi.org/10.1007/s11060-017-2631-5
Cote DJ, Dubois HM, Karhade AV, Smith TR (2016) Venous thromboembolism in patients undergoing craniotomy for brain tumors: a U.S. nationwide analysis. Semin Thromb Hemost 42:870–876. https://doi.org/10.1055/s-0036-1592306
Chaichana KL, Pendleton C, Jackson C, Martinez-Gutierrez JC, Diaz-Stransky A, Aguayo J, Olivi A, Weingart J, Gallia G, Lim M et al (2013) Deep venous thrombosis and pulmonary embolisms in adult patients undergoing craniotomy for brain tumors. Neurol Res 35:206–211. https://doi.org/10.1179/1743132812y.0000000126
Moher D, Liberati A, Tetzlaff J, Altman DG (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Intl J Surg (London, England) 8:336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Wells GA, Wells G, Shea B, Shea B, O'Connell D, Peterson J, Welch, Losos M, Tugwell P, Ga SW et al (2014) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ (Clinical research ed) 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558. https://doi.org/10.1002/sim.1186
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical research ed) 315:629–634. https://doi.org/10.1136/bmj.315.7109.629
Algattas H, Talentino SE, Eichar B, Williams AA, Murphy JM, Zhang X, Garcia RM, Newhouse D, Jaman E, Safonova A et al (2021) Venous thromboembolism anticoagulation prophylaxis timing in patients undergoing craniotomy for tumor. Neurosurgery Open 2. https://doi.org/10.1093/neuopn/okaa018
Ambulkar R, Parab SY, Vignesh B, Nagargoje V, Janu A, Parikh P, Moiyadi A (2023) A prospective study to evaluate the use of surveillance venous ultrasonography to detect incidence of deep venous thrombosis following neurosurgical excision of brain tumors. J Neurosci Rural Pract 14:252-257. 10.25259/JNRP_26_2022
Bervitskiy AV, Moisak GI, Guzhin VE, Amelina EV, Kalinovskiy AV, Rzaev DA (2021) [Incidence and risk factors of venous thromboembolic events after resection of various brain tumors]. Zh Vopr Neirokhir Im N N Burdenko 85:63-75. 10.17116/neiro20218503163
Brandes AA, Scelzi E, Salmistraro G, Ermani M, Carollo C, Berti F, Zampieri P, Baiocchi C, Fiorentino MV (1997) Incidence of risk of thromboembolism during treatment high-grade gliomas: a prospective study. Eur J Cancer 33:1592–1596. https://doi.org/10.1016/s0959-8049(97)00167-6
Carrabba G, Riva M, Conte V, Di Cristofori A, Caroli M, Locatelli M, Castellani M, Bucciarelli P, Artoni A, Stocchetti N et al (2018) Risk of post-operative venous thromboembolism in patients with meningioma. J Neuro-Oncol 138:401–406. https://doi.org/10.1007/s11060-018-2810-z
Gerber DE, Segal JB, Salhotra A, Olivi A, Grossman SA, Streiff MB (2007) Venous thromboembolism occurs infrequently in meningioma patients receiving combined modality prophylaxis. Cancer 109:300–305. https://doi.org/10.1002/cncr.22405
Gok H, Baskurt O, Sarigul B, Gurbuz D, Celik SE (2023) Silent pulmonary thromboembolism in patients undergoing craniotomy for brain tumor. Turk Neurosurg 33:87–93. https://doi.org/10.5137/1019-5149.JTN.36806-21.2
Kaewborisutsakul A, Tunthanathip T, Yuwakosol P, Inkate S, Pattharachayakul S (2020) Incidence and risk factors for venous thromboembolism following craniotomy for intracranial tumors: a cohort study. Asian J Neurosurg 15:31–38. https://doi.org/10.4103/ajns.AJNS_351_19
Lasica N, Djilvesi D, Papic V, Karan M, Jelaca B, Golubovic J, Pajicic F, Medic-Stojanoska M, Vulekovic P, Rasulic L (2022) Venous thromboembolic and hemorrhagic events after meningioma surgery: a single-center retrospective cohort study of risk factors. PLoS One 17:e0273189. https://doi.org/10.1371/journal.pone.0273189
Liu X, Zhang X, Ma T, Li M, Zhang L, Li S, Zeng M, Kass IS, Peng Y (2023) Risk factors for postoperative thrombosis-related complications in patients undergoing malignant brain tumor resection: a retrospective cohort study. Front Neurol 14:1108596. https://doi.org/10.3389/fneur.2023.1108596
Nakano F, Matsubara T, Ishigaki T, Hatazaki S, Mouri G, Nakatsuka Y, Suzuki H (2018) Incidence and risk factor of deep venous thrombosis in patients undergoing craniotomy for brain tumors: a Japanese single-center, retrospective study. Thromb Res 165:95–100. https://doi.org/10.1016/j.thromres.2018.03.016
Nunno A, Li Y, Pieters TA, Towner JE, Schmidt T, Shi M, Walter K, Li YM (2019) Risk factors and associated complications of symptomatic venous thromboembolism in patients with craniotomy for meningioma. World Neurosurg 122:e1505–e1510. https://doi.org/10.1016/j.wneu.2018.11.091
Okamoto E, Ishikawa E, Kino H, Kohzuki H, Sugii N, Naito H, Hara T, Homma S, Matsuda M, Tsurubuchi T et al (2022) Perioperative deep vein thrombosis and d-dimer measurement in patients with brain tumor. Neurol Med Chir (Tokyo) 62:186-194. 10.2176/jns-nmc.2021-0339
Qiao N, Zhang Q, Chen L, He W, Ma Z, Ye Z, He M, Zhang Z, Zhou X, Shen M et al (2023) Machine learning prediction of venous thromboembolism after surgeries of major sellar region tumors. Thromb Res 226:1–8. https://doi.org/10.1016/j.thromres.2023.04.007
Safaee M, Sun MZ, Oh T, Aghi MK, Berger MS, McDermott MW, Parsa AT, Bloch O (2014) Use of thrombin-based hemostatic matrix during meningioma resection: a potential risk factor for perioperative thromboembolic events. Clin Neurol Neurosurg 119:116–120. https://doi.org/10.1016/j.clineuro.2014.01.021
Shi S, Cheng J, Chen H, Zhang Y, Zhao Y, Wang B (2020) Preoperative and intraoperative predictors of deep venous thrombosis in adult patients undergoing craniotomy for brain tumors: a Chinese single-center, retrospective study. Thromb Res 196:245–250. https://doi.org/10.1016/j.thromres.2020.09.005
Shi S, Cheng J, Zhao Y, Chen W (2021) Incidence, and preoperative and intraoperative prognostic factors of deep venous thrombosis in patients with glioma following craniotomy. Clin Neurol Neurosurg 210:106998. https://doi.org/10.1016/j.clineuro.2021.106998
Smith TR, Lall RR, Graham RB, McClendon J Jr, Lall RR, Nanney AD, Adel JG, Zakarija A, Chandler JP (2014) Venous thromboembolism in high grade glioma among surgical patients: results from a single center over a 10 year period. J Neuro-Oncol 120:347–352. https://doi.org/10.1007/s11060-014-1557-4
Zhang C, Deng Z, Yang Z, Xie J, Hou Z (2023) A nomogram model to predict the acute venous thromboembolism risk after surgery in patients with glioma. Thromb Res 224:21–31. https://doi.org/10.1016/j.thromres.2023.02.002
Pandey A, Thakur B, Hogg F, Brogna C, Logan J, Arya R, Gullan R, Bhangoo R, Ashkan K (2018) The role of preoperative deep vein thrombosis screening in neurooncology. J Neurosurg 130:38–43. https://doi.org/10.3171/2017.9.Jns17176
Alshehri N, Cote DJ, Hulou MM, Alghamdi A, Alshahrani A, Mekary RA, Smith TR (2016) Venous thromboembolism prophylaxis in brain tumor patients undergoing craniotomy: a meta-analysis. J Neuro-Oncol 130:561–570. https://doi.org/10.1007/s11060-016-2259-x
Qian C, Yan H, Hu X, Zhang W, Liu H (2016) Increased risk of venous thromboembolism in patients with brain tumors: a systematic review and meta-analysis. Thromb Res 137:58–63. https://doi.org/10.1016/j.thromres.2015.11.018
Anderson BP, Sioshansi PC, Conway RM, Minutello K, Bojrab DI, Hong RS, Sargent EW, Schutt CA, Bojrab DI 2nd, Zappia JJ et al (2022) Rate of development of venous thromboembolism in lateral skull base surgery. Laryngoscope 132:662–667. https://doi.org/10.1002/lary.29889
Hong KC, Kim H, Kim JY, Kwak KS, Cho OM, Cha HY, Lim SH, Song YJ (2012) Risk factors and incidence of deep vein thrombosis in lower extremities among critically ill patients. J Clin Nurs 21:1840–1846. https://doi.org/10.1111/j.1365-2702.2012.04112.x
Hill J, Treasure T (2007) Reducing the risk of venous thromboembolism (deep vein thrombosis and pulmonary embolism) in inpatients having surgery: summary of NICE guidance. BMJ (Clinical research ed) 334:1053–1054. https://doi.org/10.1136/bmj.39174.678032.AD
Schrag D, Uno H, Rosovsky R, Rutherford C, Sanfilippo K, Villano JL, Drescher M, Jayaram N, Holmes C, Feldman L et al (2023) Direct oral anticoagulants vs low-molecular-weight heparin and recurrent VTE in patients with cancer: a randomized clinical trial. Jama 329:1924–1933. https://doi.org/10.1001/jama.2023.7843
Kaptein FHJ, Stals MAM, Kapteijn MY, Cannegieter SC, Dirven L, van Duinen SG, van Eijk R, Huisman MV, Klaase EE, Taphoorn MJB et al (2022) Incidence and determinants of thrombotic and bleeding complications in patients with glioblastoma. J Thrombosis Haemostasis : JTH 20:1665–1673. https://doi.org/10.1111/jth.15739
Jo J, Diaz M, Horbinski C, Mackman N, Bagley S, Broekman M, Rak J, Perry J, Pabinger I, Key NS et al (2023) Epidemiology, biology, and management of venous thromboembolism in gliomas: an interdisciplinary review. Neuro-Oncology 25:1381–1394. https://doi.org/10.1093/neuonc/noad059
Simanek R, Vormittag R, Hassler M, Roessler K, Schwarz M, Zielinski C, Pabinger I, Marosi C (2007) Venous thromboembolism and survival in patients with high-grade glioma. Neuro-Oncology 9:89–95. https://doi.org/10.1215/15228517-2006-035
Riedl J, Ay C (2019) Venous thromboembolism in brain tumors: risk factors, molecular mechanisms, and clinical challenges. Semin Thromb Hemost 45:334–341. https://doi.org/10.1055/s-0039-1688493
Khalil J, Bensaid B, Elkacemi H, Afif M, Bensaid Y, Kebdani T, Benjaafar N (2015) Venous thromboembolism in cancer patients: an underestimated major health problem. World J Surg Oncol 13:204. https://doi.org/10.1186/s12957-015-0592-8
Suh JH, Kotecha R, Chao ST, Ahluwalia MS, Sahgal A, Chang EL (2020) Current approaches to the management of brain metastases. Nat Rev Clin Oncol 17:279–299. https://doi.org/10.1038/s41571-019-0320-3
Pinzi V, Orsi C, Marchetti M, Milanesi IM, Bianchi LC, DiMeco F, Cuccarini V, Farinotti M, Ferroli P, Finocchiaro G et al (2015) Radiosurgery reirradiation for high-grade glioma recurrence: a retrospective analysis. Neurol Sci Official J Italian Neurol Soc Italian Society Clin Neurophysiol 36:1431–1440. https://doi.org/10.1007/s10072-015-2172-7
Lyman GH, Kuderer NM (2020) Clinical practice guidelines for the treatment and prevention of cancer-associated thrombosis. Thromb Res 191(Suppl 1):S79–s84. https://doi.org/10.1016/s0049-3848(20)30402-3
Practice American Diabetes Association Professional, C, (2022) 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2022. Diabetes care 45:S17–S38. https://doi.org/10.2337/dc22-S002
Bell EJ, Folsom AR, Lutsey PL, Selvin E, Zakai NA, Cushman M, Alonso A (2016) Diabetes mellitus and venous thromboembolism: a systematic review and meta-analysis. Diabetes Res Clin Pract 111:10–18. https://doi.org/10.1016/j.diabres.2015.10.019
Palermo NE, Gianchandani RY, McDonnell ME, Alexanian SM (2016) Stress hyperglycemia during surgery and anesthesia: pathogenesis and clinical implications. Current Diabetes Reports 16:33. https://doi.org/10.1007/s11892-016-0721-y
Clarke RS (1970) The hyperglycaemic response to different types of surgery and anaesthesia. Br J Anaesth 42:45–53. https://doi.org/10.1093/bja/42.1.45
Dąbrowska E, Narkiewicz K (2023) Hypertension and dyslipidemia: the two partners in endothelium-related crime. Curr Atheroscler Rep 25:605–612. https://doi.org/10.1007/s11883-023-01132-z
Gonzalez Della Valle A, Shanaghan KA, Nguyen J, Liu J, Memtsoudis S, Sharrock NE, Salvati EA (2020) Multimodal prophylaxis in patients with a history of venous thromboembolism undergoing primary elective hip arthroplasty. The bone & joint journal 102-b:71-77. 10.1302/0301-620x.102b7.Bjj-2019-1559.R1
Kakkar VV, Howe CT, Nicolaides AN, Renney JT, Clarke MB (1970) Deep vein thrombosis of the leg. Is there a “high risk” group? Am J Surg 120:527–530. https://doi.org/10.1016/s0002-9610(70)80023-x
White RH, Henderson MC (2002) Risk factors for venous thromboembolism after total hip and knee replacement surgery. Curr Opin Pulm Med 8:365–371. https://doi.org/10.1097/00063198-200209000-00004
White RH, Zhou H, Gage BF (2004) Effect of age on the incidence of venous thromboembolism after major surgery. J Thrombosis Haemostasis : JTH 2:1327–1333. https://doi.org/10.1046/j.1538-7836.2004.00848.x
Lieber BA, Han J, Appelboom G, Taylor BE, Han B, Agarwal N, Connolly ES Jr (2016) Association of steroid use with deep venous thrombosis and pulmonary embolism in neurosurgical patients: a national database analysis. World Neurosurg 89:126–132. https://doi.org/10.1016/j.wneu.2016.01.033
Sarlos P, Szemes K, Hegyi P, Garami A, Szabo I, Illes A, Solymar M, Petervari E, Vincze A, Par G et al (2018) Steroid but not biological therapy elevates the risk of venous thromboembolic events in inflammatory bowel disease: a meta-analysis. J Crohn's & Colitis 12:489–498. https://doi.org/10.1093/ecco-jcc/jjx162
Børvik T, Evensen LH, Morelli VM, Melbye H, Brækkan SK, Hansen JB (2020) Impact of respiratory symptoms and oxygen saturation on the risk of incident venous thromboembolism-the Tromsø study. Res Practice Thrombosis Haemostasis 4:255–262. https://doi.org/10.1002/rth2.12299
Funding
This study was funded by the Open Project Program of Key Laboratory of Big Data Analysis and Knowledge Services of Yangzhou University (YBK202202), the National Natural Science Foundation of China (No. 72374178, No. 71904165, No. 82172603), the Natural Science Foundation of Jiangsu Province (BK20221280), the Special Fund for Social Key Research and Development Plan of Yangzhou City (YZ2022097), the Chinese Postdoctoral Science Foundation (2022M711426), the Jiangsu Provincial Health Commission New Technology Introduction and Evaluation Project (M2022044).
Author information
Authors and Affiliations
Contributions
All authors played a part in the planning of the meta-analysis. The first two authors (GYL and QPZ) undertook the literature search and obtained the data from published literature. The data were analyzed by QPZ, and the initial draft of the manuscript was undertaken by GYL, QPZ, and YPL. All authors reviewed the initial draft of the manuscript and helped prepare the final draft for submission. All authors have critically read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval
None.
Consent to participate
No informed consents were required for the purpose of the current study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Qingping Zeng, Guangyu Lu, and Jing Yuan should be considered joint first author.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zeng, Q., Lu, G., Yuan, J. et al. Prevalence, characteristics, and risk factors of venous thromboembolism in patients with brain tumor undergoing craniotomy: a meta-analysis. Neurol Sci 45, 1565–1580 (2024). https://doi.org/10.1007/s10072-023-07160-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-07160-6