Abstract
Background
The Apolipoprotein E (APOE) ε4 allele is a risk factor for late-onset Alzheimer’s disease (AD). However, no investigation has focused on racial differences in the longitudinal effect of APOE genotypes on CSF amyloid beta (Aβ42) and tau levels in AD.
Methods
This study used data from the Alzheimer’s Disease Neuroimaging Initiative (ADNI): 222 participants with AD, 264 with cognitive normal (CN), and 692 with mild cognitive impairment (MCI) at baseline and two years follow-up. We used a linear mixed model to investigate the effect of APOE-ε4-genotypes on longitudinal changes in the amyloid beta and tau levels.
Results
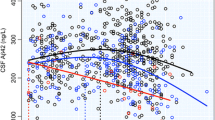
Individuals with 1 or 2 APOE ε4 alleles revealed significantly higher t-Tau and p-Tau, but lower amyloid beta Aβ42 compared with individuals without APOE ε4 alleles. Significantly higher levels of log-t-Tau, log-p-Tau, and low levels of log-Aβ42 were observed in the subjects with older age, being female, and the two diagnostic groups (AD and MCI). The higher p-Tau and Aβ42 values are associated with poor Mini-Mental State Examination (MMSE) performance. Non-Hispanic Africa American (AA) and Hispanic participants were associated with decreased log-t-Tau levels (β = − 0.154, p = 0.0112; β = − 0.207, and p = 0.0016, respectively) as compared to those observed in Whites. Furthermore, Hispanic participants were associated with a decreased log-p-Tau level (β = − 0.224, p = 0.0023) compared to those observed in Whites. There were no differences in Aβ42 level for non-Hispanic AA and Hispanic participants compared with White participants.
Conclusion
Our study, for the first time, showed that the APOE ε4 allele was associated with these biomarkers, however with differing degrees among racial groups.



Similar content being viewed by others
Data availability
Data used in the preparation of this article was obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu).
References
Association A. s (2021) Alzheimer’s disease facts and figures 2021. Alzheimer’s Dement 17:327–406
Association A. s (2016) 2016 Alzheimer's disease facts and figures. Alzheimers Dement 12:459–509. https://doi.org/10.1016/j.jalz.2016.03.001. https://alz-journals.onlinelibrary.wiley.com/doi/abs/ https://doi.org/10.1016/j.jalz.2016.03.001
Association A. s (2022) 2022 Alzheimer's disease facts and figures. Alzheimers Dement 18:700–89. https://doi.org/10.1002/alz.12638. https://www.ncbi.nlm.nih.gov/pubmed/35289055
Lozano S, Padilla V, Avila ML, Gil M, Maestre G, Wang K, Xu C (2021) APOE gene associated with cholesterol-related traits in the Hispanic population. Genes (Basel) 12. https://doi.org/10.3390/genes12111768. https://www.ncbi.nlm.nih.gov/pubmed/34828374
Reitz C, Mayeux R (2014) Genetics of Alzheimer’s disease in Caribbean Hispanic and African American populations. Biol Psychiat 75:534–541. https://doi.org/10.1016/j.biopsych.2013.06.003.10.1016/j.biopsych.2013.06.003
Rodriguez-Vieitez E, Nielsen HM (2019) Associations between APOE variants, tau and α-synuclein. Adv Exp Med Biol 1184:177–186. https://doi.org/10.1007/978-981-32-9358-8_15
Pang C, Yang H, Hu B, Wang S, Chen M, Cohen DS, Chen HS, Jarrell JT, Carpenter KA, Rosin ER et al (2019) Identification and analysis of Alzheimer's candidate genes by an amplitude deviation algorithm. J Alzheimers Dis Parkinsonism 9. https://doi.org/10.4172/2161-0460.1000460
Hebert LE, Weuve J, Scherr PA, Evans DA (2013) Alzheimer disease in the united states (2010-2050) estimated using the 2010 census. Neurology 80:1778–1783. https://doi.org/10.1212/wnl.0b013e31828726f5
Nebel RA, Aggarwal NT, Barnes LL, Gallagher A, Goldstein JM, Kantarci K, Mallampalli MP, Mormino EC, Scott L, Yu WH et al (2018) Understanding the impact of sex and gender in Alzheimer’s disease: a call to action. Alzheimers Dement 14:1171–1183. https://doi.org/10.1016/j.jalz.2018.04.008.10.1016/j.jalz.2018.04.008
Yamazaki Y, Zhao N, Caulfield TR, Liu C-C, Bu G (2019) Apolipoprotein e and Alzheimer disease: pathobiology and targeting strategies. Nat Rev Neurol 15:501–518. https://doi.org/10.1038/s41582-019-0228-7.10.1038/s41582-019-0228-7
Burnham SC, Laws SM, Budgeon CA, Dore V, Porter T, Bourgeat P, Buckley RF, Murray K, Ellis KA, Turlach BA et al (2020) "Impact of APOE-epsilon4 carriage on the onset and rates of neocortical Abeta-amyloid deposition. Neurobiol Aging 95:46–55. https://doi.org/10.1016/j.neurobiolaging.2020.06.001. https://www.ncbi.nlm.nih.gov/pubmed/32750666
Frisoni GB, Altomare D, Thal DR, Ribaldi F, van der Kant R, Ossenkoppele R, Blennow K, Cummings J, van Duijn C, Nilsson PM et al (2022) The probabilistic model of Alzheimer disease: the amyloid hypothesis revised. Nat Rev Neurosci 23:53–66. https://doi.org/10.1038/s41583-021-00533-w. https://www.ncbi.nlm.nih.gov/pubmed/34815562
Saddiki H, Fayosse A, Cognat E, Sabia S, Engelborghs S, Wallon D, Alexopoulos P, Blennow K, Zetterberg H, Parnetti L et al (2020) Age and the association between apolipoprotein e genotype and Alzheimer disease: a cerebrospinal fluid biomarker–based case–control study. PLOS Med 17:e1003289. https://doi.org/10.1371/journal.pmed.1003289
Schindler SE, Karikari TK, Ashton NJ, Henson RL, Yarasheski KE, West T, Meyer MR, Kirmess KM, Li Y, Saef B et al (2022) Effect of race on prediction of brain amyloidosis by plasma abeta42/abeta40, phosphorylated tau, and neurofilament light. Neurology 99:e245-e57. https://doi.org/10.1212/WNL.0000000000200358. https://www.ncbi.nlm.nih.gov/pubmed/35450967
Mahaman YAR, Embaye KS, Huang F, Li L, Zhu F, Wang JZ, Liu R, Feng J, Wang X (2022) Biomarkers used in Alzheimer's disease diagnosis, treatment, and prevention. Ageing Res Rev 74:101544. https://doi.org/10.1016/j.arr.2021.101544. https://www.ncbi.nlm.nih.gov/pubmed/34933129
Ferreira D, Rivero-Santana A, Perestelo-Pérez L, Westman E, Wahlund LO, Sarría A, Serrano-Aguilar P (2014) Improving CSF biomarkers’ performance for predicting progression from mild cognitive impairment to Alzheimer’s disease by considering different confounding factors: a meta-analysis. Front Aging Neurosci 6:287. https://doi.org/10.3389/fnagi.2014.00287
Dubois B, Feldman HH, Jacova C, Cummings JL, Dekosky ST, Barberger-Gateau P, Delacourte A, Frisoni G, Fox NC, Galasko D et al (2010) Revising the definition of Alzheimer’s disease: a new lexicon. Lancet Neurol 9:1118–1127. https://doi.org/10.1016/s1474-4422(10)70223-4
Gendron TF, Petrucelli L (2009) The role of tau in neurodegeneration. Mol Neurodegener 4:13. https://doi.org/10.1186/1750-1326-4-13
Konijnenberg E, Tomassen J, den Braber A, Ten Kate M, Yaqub M, Mulder SD, Nivard MG, Vanderstichele H, Lammertsma AA, Teunissen CE et al (2021) Onset of preclinical Alzheimer disease in monozygotic twins. Ann Neurol 89:987–1000. https://doi.org/10.1002/ana.26048. https://www.ncbi.nlm.nih.gov/pubmed/33583080
Jellinger KA (2020) Pathobiological subtypes of Alzheimer disease. Dement Geriatr Cogn Disord 49:321–33. https://doi.org/10.1159/000508625
Andreasen N, Minthon L, Vanmechelen E, Vanderstichele H, Davidsson P, Winblad B, Blennow K (1999) Cerebrospinal fluid tau and abeta42 as predictors of development of Alzheimer’s disease in patients with mild cognitive impairment. Neurosci Lett 273:5–8. https://doi.org/10.1016/s0304-3940(99)00617-5
Blennow K, Zetterberg H (2018) Biomarkers for Alzheimer’s disease: current status and prospects for the future. J Intern Med 284:643–663. https://doi.org/10.1111/joim.12816.10.1111/joim.12816
Husain MA, Laurent B, Plourde M (2021) APOE and Alzheimer's disease: from lipid transport to physiopathology and therapeutics. Front Neurosci 15:630502. https://doi.org/10.3389/fnins.2021.630502. https://www.ncbi.nlm.nih.gov/pubmed/33679311
Cockrell JR, Folstein MF (1988) Mini-mental state examination (MMSE). Psychopharmacol Bull 24:689–692
Faul F, Erdfelder E, Lang AG, Buchner A (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39:175–91. https://doi.org/10.3758/bf03193146. https://www.ncbi.nlm.nih.gov/pubmed/17695343
Faul F, Erdfelder E, Buchner A, Lang AG (2009) Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41:1149–60. https://doi.org/10.3758/BRM.41.4.1149. https://www.ncbi.nlm.nih.gov/pubmed/19897823
Gu L, Shu H, Wang Y, Wang P (2023) Blood neurofilament light chain in different types of dementia. Curr Alzheimer Res. https://doi.org/10.2174/1567205020666230601123123. https://www.ncbi.nlm.nih.gov/pubmed/37264656
Lautner R, Palmqvist S, Mattsson N, Andreasson U, Wallin A, Palsson E, Jakobsson J, Herukka SK, Owenius R, Olsson B et al (2014) Apolipoprotein e genotype and the diagnostic accuracy of cerebrospinal fluid biomarkers for Alzheimer disease. JAMA Psychiatry 71:1183–91. https://doi.org/10.1001/jamapsychiatry.2014.1060. https://www.ncbi.nlm.nih.gov/pubmed/25162367
Konijnenberg E, Tijms BM, Gobom J, Dobricic V, Bos I, Vos S, Tsolaki M, Verhey F, Popp J, Martinez-Lage P et al (2020) APOE epsilon4 genotype-dependent cerebrospinal fluid proteomic signatures in Alzheimer's disease. Alzheimers Res Ther 12:65. https://doi.org/10.1186/s13195-020-00628-z. https://www.ncbi.nlm.nih.gov/pubmed/32460813
Morris JC, Roe CM, Xiong C, Fagan AM, Goate AM, Holtzman DM, Mintun MA (2010) APOE predicts amyloid-beta but not tau Alzheimer pathology in cognitively normal aging. Ann Neurol 67:122–31. https://doi.org/10.1002/ana.21843. https://www.ncbi.nlm.nih.gov/pubmed/20186853
Risacher SL, Kim S, Shen L, Nho K, Foroud T, Green RC, Petersen RC, Jack CR Jr, Aisen PS, Koeppe RA et al (2013) The role of apolipoprotein e (APOE) genotype in early mild cognitive impairment (E-MCI). Front Aging Neurosci 5:11. https://doi.org/10.3389/fnagi.2013.00011. https://www.ncbi.nlm.nih.gov/pubmed/23554593
Benson GS, Bauer C, Hausner L, Couturier S, Lewczuk P, Peters O, Hull M, Jahn H, Jessen F, Pantel J et al (2022) Don't forget about tau: the effects of ApoE4 genotype on Alzheimer's disease cerebrospinal fluid biomarkers in subjects with mild cognitive impairment-data from the dementia competence network. J Neural Transm (Vienna) 129:477–86. https://doi.org/10.1007/s00702-022-02461-0. https://www.ncbi.nlm.nih.gov/pubmed/35061102
Schwartzentruber J, Cooper S, Liu JZ, Barrio-Hernandez I, Bello E, Kumasaka N, Young AMH, Franklin RJM, Johnson T, Estrada K et al (2021) Genome-wide meta-analysis, fine-mapping and integrative prioritization implicate new Alzheimer’s disease risk genes. Nat Genet 53:392–402. https://doi.org/10.1038/s41588-020-00776-w
Suri S, Heise V, Trachtenberg AJ, Mackay CE (2013) The forgotten APOE allele: a review of the evidence and suggested mechanisms for the protective effect of APOE ɛ2. Neurosci Biobehav Rev 37:2878–2886. https://doi.org/10.1016/j.neubiorev.2013.10.010
Oikonomidi A, Tautvydaite D, Gholamrezaee MM, Henry H, Bacher M, Popp J (2017) Macrophage migration inhibitory factor is associated with biomarkers of Alzheimer's disease pathology and predicts cognitive decline in mild cognitive impairment and mild dementia. J Alzheimers Dis 60:273–81. https://doi.org/10.3233/JAD-170335. https://www.ncbi.nlm.nih.gov/pubmed/28826184
Grewal R, Haghighi M, Huang S, Smith AG, Cao C, Lin X, Lee DC, Teten N, Hill AM, Selenica MB (2016) Identifying biomarkers of dementia prevalent among amnestic mild cognitively impaired ethnic female patients. Alzheimers Res Ther 8:43. https://doi.org/10.1186/s13195-016-0211-0. https://www.ncbi.nlm.nih.gov/pubmed/27756387
Morris JC, Schindler SE, McCue LM, Moulder KL, Benzinger TLS, Cruchaga C, Fagan AM, Grant E, Gordon BA, Holtzman DM et al (2019) Assessment of racial disparities in biomarkers for Alzheimer disease. JAMA Neurol 76:264–73. https://doi.org/10.1001/jamaneurol.2018.4249. https://www.ncbi.nlm.nih.gov/pubmed/30615028
Moon S, Kim S, Mankhong S, Choi SH, Vandijck M, Kostanjevecki V, Jeong JH, Yoon SJ, Park KW, Kim E-J et al (2021) Alzheimer’s cerebrospinal biomarkers from Lumipulse fully automated immunoassay: concordance with amyloid-beta pet and manual immunoassay in Koreans. Alzheimers Res Ther 13:22. https://doi.org/10.1186/s13195-020-00767-3.10.1186/s13195-020-00767-3
Manly JJ, Touradji P, Tang MX, Stern Y (2003) Literacy and memory decline among ethnically diverse elders. J Clin Exp Neuropsychol 25:680–690. https://doi.org/10.1076/jcen.25.5.680.14579
Yaffe K, Falvey C, Harris TB, Newman A, Satterfield S, Koster A, Ayonayon H, Simonsick E (2013) Effect of socioeconomic disparities on incidence of dementia among biracial older adults: prospective study. Bmj 347:f7051. https://doi.org/10.1136/bmj.f7051
Barnes LL, Bennett DA (2014) Alzheimer’s disease in African Americans: risk factors and challenges for the future. Health Aff (Millwood) 33:580–586. https://doi.org/10.1377/hlthaff.2013.1353
Bellenguez C, Kucukali F, Jansen IE, Kleineidam L, Moreno-Grau S, Amin N, Naj AC, Campos-Martin R, Grenier-Boley B, Andrade V et al (2022) New insights into the genetic etiology of Alzheimer's disease and related dementias. Nat Genet 54:412–36. https://doi.org/10.1038/s41588-022-01024-z. https://www.ncbi.nlm.nih.gov/pubmed/35379992
Misiura MB, Howell JC, Wu J, Qiu D, Parker MW, Turner JA, Hu WT (2020) Race modifies default mode connectivity in Alzheimer's disease. Transl Neurodegener 9:8. https://doi.org/10.1186/s40035-020-0186-4. https://www.ncbi.nlm.nih.gov/pubmed/32099645
Acknowledgements
The present study is a secondary data analysis. The original study and ADNI were funded by the Alzheimer’s Disease Neuroimaging Initiative (ADNI) (National Institutes of Health Grant U01 AG024904) and DOD ADNI (Department of Defense award number W81XWH-12-2-0012). ADNI is funded by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and through generous contributions from the following: AbbVie, Alzheimer’s Association; Alzheimer’s Drug Discovery Foundation; Araclon Biotech; BioClinica, Inc.; Biogen; Bristol-Myers Squibb Company; CereSpir, Inc.; Cogstate; Eisai Inc.; Elan Pharmaceuticals, Inc.; Eli Lilly and Company; EuroImmun; F. Hoffmann-La Roche Ltd. and its affiliated company Genentech, Inc.; Fujirebio; GE Healthcare; IXICO Ltd.; Janssen Alzheimer Immunotherapy Research & Development, LLC.; Johnson & Johnson Pharmaceutical Research & Development LLC.; Lumosity; Lundbeck; Merck & Co., Inc.; Meso Scale Diagnostics, LLC.; NeuroRx Research; Neurotrack Technologies; Novartis Pharmaceuticals Corporation; Pfizer Inc.; Piramal Imaging; Servier; Takeda Pharmaceutical Company; and Transition Therapeutics. The Canadian Institutes of Health Research is providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health (www.fnih.org). The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer’s Therapeutic Research Institute at the University of Southern California. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California. Data used in preparation of this article were obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu). As such, the investigators within the ADNI contributed to the design and implementation of ADNI and/or provided data but did not participate in analysis or writing of this report. A complete listing of ADNI investigators can be found at: http://adni.loni.usc.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization, C.X. and K.W.; methodology, C.X., D.X., B.B.S., and K.W.; data analysis and interpretation, C.X., D.X., N.W., D.A.A., and K.W.; investigation, C.X., D.X., and K.W.; writing—original draft preparation, C.X., D.X., J.M.S., D.G., U.R., and K.W.; writing—review and editing, D.X., B.B.S., O.R.N., N.W., and D.A.A.; supervision, C.X. and K.W.; all authors read and agreed to the published version of the manuscript. The Alzheimer’s Disease Neuroimaging Initiative—data used in the preparation of this article were obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu).
Corresponding author
Ethics declarations
Ethical approval
There was an Institutional Review Board exemption for the current study due to secondary data analysis. Data used in the preparation of this article was obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu).
Informed consent
Informed consent was obtained from all subjects involved in the original study. Data used in the preparation of this article was obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, C., Xiao, D., Su, B.B. et al. Association of APOE gene with longitudinal changes of CSF amyloid beta and tau levels in Alzheimer’s disease: racial differences. Neurol Sci 45, 1041–1050 (2024). https://doi.org/10.1007/s10072-023-07076-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-07076-1