Abstract
Objective
Dysphagia is a common and serious clinical symptom of amyotrophic lateral sclerosis (ALS). The study aimed to evaluate the diagnostic utility of four dysphagia screening tools in ALS, including the ALS Functional Rating Scale-Revised (ALSFRS-R) bulbar subscale, water-swallowing test (WST), Eating Assessment Tool-10 (EAT-10) and Sydney Swallow Questionnaire (SSQ).
Methods
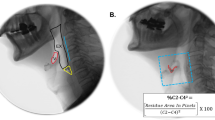
A total of 68 individuals from First Hospital, Shanxi medical university, were recruited in the study. The ALSFRS-R, WST, EAT-10, SSQ and the gold standard video fluoroscopic swallowing study (VFSS) were performed. The Penetration Aspiration Scale (PAS) during VFSS was assessed to identify unsafe swallowing (PAS ≥ 3) and aspiration (PAS ≥ 6). Receiver operator characteristic curve (ROC) analyses were performed to evaluate the accuracy of the 4 tools. Youden index was used to determine the ideal cut-off value for each tool.
Results
Of the patients, 20.59% (14/68) presented unsafety swallowing and 16.18% (11/68) had aspiration. The four tools could effectively identify patients with unsafe swallowing and aspiration. The EAT-10 had the maximum AUC (0.873 and 0.963, respectively) among the tools in the diagnosis of unsafe swallowing and aspiration. To detect unsafe swallowing and aspiration, an EAT-10 score of 6 (sensitivity: 78.6%, specificity: 87.0%) and an EAT-10 score of 8 (sensitivity: 90.9%, specificity: 91.2%), were the most appropriate cut-off points, respectively.
Conclusions
The ALSFRS-R bulbar subscale, WST, EAT-10, and SSQ could effectively identify unsafe swallowing and aspiration in patients with ALS. Of the four tools, the EAT-10 was relatively accurate, safe, and convenient. Further studies including more patients should be conducted to verify the conclusions.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author.
References
Hardiman O, Al-Chalabi A, Chio A, Corr E, Logroscino G, Robberecht W, Shaw P, Simmons Z, van den Berg L (2017) Amyotrophic lateral sclerosis. Nat Rev Dis Primers 3:17071. https://doi.org/10.1038/nrdp.2017.71
van Es M, Hardiman O, Chio A, Al-Chalabi A, Pasterkamp R, Veldink J, van den Berg L (2017) Amyotrophic lateral sclerosis. Lancet 390(10107):2084–2098. https://doi.org/10.1016/s0140-6736(17)31287-4
Aydogdu I, Tanriverdi Z, Ertekin C (2011) Dysfunction of bulbar central pattern generator in ALS patients with dysphagia during sequential deglutition. Clin Neurophysiol 122(6):1219–1228. https://doi.org/10.1016/j.clinph.2010.11.002
Lisiecka D, Kelly H, Jackson J (2021) How do people with Motor Neurone Disease experience dysphagia? A qualitative investigation of personal experiences. Disabil Rehabil 43(4):479–488. https://doi.org/10.1080/09638288.2019.1630487
Andersen P, Abrahams S, Borasio G, de Carvalho M, Chio A, Van Damme P, Hardiman O, Kollewe K, Morrison K, Petri S et al (2012) EFNS guidelines on the clinical management of amyotrophic lateral sclerosis (MALS)–revised report of an EFNS task force. Eur J Neurol 19(3):360–375. https://doi.org/10.1111/j.1468-1331.2011.03501.x
Winterholler C (2008) Diagnosis and treatment of dysphagia in patients with neuromuscular disease. Pneumologie 62(1):S35-38. https://doi.org/10.1055/s-2007-1038100
Schaen-Heacock N, Jones C, McCulloch T (2021) Pharyngeal Swallowing Pressures in Patients with Radiation-Associated Dysphagia. Dysphagia 36(2):242–249. https://doi.org/10.1007/s00455-020-10128-9
Chapin JL, Gray LT, Vasilopoulos T, Anderson A, DiBiase L, York JD, Robison R, Wymer J, Plowman EK (2020) Diagnostic utility of the amyotrophic lateral sclerosis Functional Rating Scale-Revised to detect pharyngeal dysphagia in individuals with amyotrophic lateral sclerosis. PloS One 15(8):e0236804. https://doi.org/10.1371/journal.pone.0236804
Rooney J, Burke T, Vajda A, Heverin M, Hardiman O (2017) What does the ALSFRS-R really measure? A longitudinal and survival analysis of functional dimension subscores in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry 88(5):381–385. https://doi.org/10.1136/jnnp-2016-314661
Osawa A, Maeshima S, Tanahashi N (2013) Water-swallowing test: screening for aspiration in stroke patients. Cerebrovascular Diseases 35(3):276–281. https://doi.org/10.1159/000348683
Park K, Kim T, Lee S (2020) The Gugging Swallowing Screen in dysphagia screening for patients with stroke: A systematic review. Int J Nurs Stud 107:103588. https://doi.org/10.1016/j.ijnurstu.2020.103588
Bartlett RS, Kenz MK, Wayment HA, Thibeault SL (2022) Correlation Between EAT-10 and Aspiration Risk Differs by Dysphagia Etiology. Dysphagia 37(1):11–20. https://doi.org/10.1007/s00455-021-10244-0
Raginis-Zborowska A, Mekli K, Payton A, Ollier W, Hamdy S, Pendleton N (2015) Genetic determinants of swallowing impairments among community dwelling older population. Exp Gerontol 69:196–201. https://doi.org/10.1016/j.exger.2015.06.014
Teramoto S, Fukuchi Y (2000) Detection of aspiration and swallowing disorder in older stroke patients: simple swallowing provocation test versus water swallowing test. Arch Phys Med Rehabil 81(11):1517–1519. https://doi.org/10.1053/apmr.2000.9171
Belafsky P, Mouadeb D, Rees C, Pryor J, Postma G, Allen J, Leonard R (2008) Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol 117(12):919–924. https://doi.org/10.1177/000348940811701210
Dwivedi R, St Rose S, Roe J, Khan A, Pepper C, Nutting C, Clarke P, Kerawala C, Rhys-Evans P, Harrington K, Kazi R (2010) Validation of the Sydney Swallow Questionnaire (SSQ) in a cohort of head and neck cancer patients. Oral Oncol 46(4):e10-14. https://doi.org/10.1016/j.oraloncology.2010.02.004
Cedarbaum JM, Stambler N, Malta E, Fuller C, Hilt D, Thurmond B, Nakanishi A (1999) The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. BDNF ALS Study Group (Phase III). J Neurol Sci 169(1–2):13–21. https://doi.org/10.1016/s0022-510x(99)00210-5
Wu W, Bi X, Song L, Liu Z (2016) Value of applying water swallowing test for patients with dysphagia after acute stroke. J Shanghai Jiao Tong Univ 36:1049–1053. https://doi.org/10.3969/j.issn.1674-8115.2016.07.018
Wilmskoetter J, Bonilha H, Hong I, Hazelwood R, Martin-Harris B, Velozo C (2019) Construct validity of the Eating Assessment Tool (EAT-10). Disabil Rehabil 41(5):549–559. https://doi.org/10.1080/09638288.2017.1398787
Wallace KL, Middleton S, Cook IJ (2000) Development and validation of a self-report symptom inventory to assess the severity of oral-pharyngeal dysphagia. Gastroenterology 118(4):678–687. https://doi.org/10.1016/s0016-5085(00)70137-5
Dwivedi RC, St Rose S, Chisholm EJ, Georgalas C, Bisase B, Amen F, Kerawala CJ, Clarke PM, Nutting CM, Rhys-Evans PH et al (2012) Evaluation of swallowing by Sydney Swallow Questionnaire (SSQ) in oral and oropharyngeal cancer patients treated with primary surgery. Dysphagia 27(4):491–497. https://doi.org/10.1007/s00455-012-9395-z
Audag N, Liistro G, Goubau C, Vandervelde L, Poncin W, Toussaint M, Van den Bergh P, Reychler G (2021) Screening for oropharyngeal dysphagia in adult patients with neuromuscular diseases using the Sydney Swallow Questionnaire. Muscle Nerve 64(3):277–284. https://doi.org/10.1002/mus.27254
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL (1996) A penetration-aspiration scale. Dysphagia 11(2):93–98. https://doi.org/10.1007/bf00417897
Cheney DM, Siddiqui MT, Litts JK, Kuhn MA, Belafsky PC (2015) The Ability of the 10-Item Eating Assessment Tool (EAT-10) to Predict Aspiration Risk in Persons With Dysphagia. Ann Otol Rhinol Laryngol 124(5):351–354. https://doi.org/10.1177/0003489414558107
Rofes L, Arreola V, Mukherjee R, Clavé P (2014) Sensitivity and specificity of the Eating Assessment Tool and the Volume-Viscosity Swallow Test for clinical evaluation of oropharyngeal dysphagia. Neurogastroenterol Motil : Off J Eur Gastrointest Motil Soc 26(9):1256–1265. https://doi.org/10.1111/nmo.12382
Donohue C, Tabor Gray L, Anderson A, DiBiase L, Chapin J, Wymer JP, Plowman EK (2022) Discriminant Ability of the Eating Assessment Tool-10 to Detect Swallowing Safety and Efficiency Impairments. The Laryngoscope. https://doi.org/10.1002/lary.30043
Donohue C, Tabor Gray L, Chapin J, Anderson A, DiBiase L, Wymer JP, Plowman EK (2022) Discriminant ability of the 3-ounce water swallow test to detect aspiration in amyotrophic lateral sclerosis. Neurogastroenterol Motil : Off J Eur Gastrointest Motil Soc 34(7):e14310. https://doi.org/10.1111/nmo.14310
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3(1):32–35. https://doi.org/10.1002/1097-0142(1950)3:1%3c32::aid-cncr2820030106%3e3.0.co;2-3
Plowman EK, Tabor LC, Robison R, Gaziano J, Dion C, Watts SA, Vu T, Gooch C (2016) Discriminant ability of the Eating Assessment Tool-10 to detect aspiration in individuals with amyotrophic lateral sclerosis. Neurogastroenterol Motil : Off J Eur Gastrointest Motil Soc 28(1):85–90. https://doi.org/10.1111/nmo.12700
Chen P, Chuang C, Leong C, Guo S, Hsin Y (2016) Systematic review and meta-analysis of the diagnostic accuracy of the water swallow test for screening aspiration in stroke patients. J Adv Nurs 72(11):2575–2586. https://doi.org/10.1111/jan.13013
Atar S, Atar Y, Ilgin C, Uygan U, Demirhan E, Anarat MEA, Tutar B, Sari H, Berkiten G, Kuru Ö (2022) Validity and Reliability of the Turkish Version of the Sydney Swallow Questionnaire. Am J Speech Lang Pathol 31(4):1726–1735. https://doi.org/10.1044/2022_ajslp-21-00268
Audag N, Goubau C, Danse E, Vandervelde L, Liistro G, Toussaint M, Reychler G (2019) Validation and Reliability of the French Version of the Sydney Swallow Questionnaire. Dysphagia 34(4):556–566. https://doi.org/10.1007/s00455-019-09978-9
Bohlender J, Frick S, Colotto U, Hotzenköcherle S, Brockmann-Bauser M (2021) The German Sydney Swallow Questionnaire : Reliability and validity in patients with oropharyngeal dysphagia. HNO 69(12):969–977. https://doi.org/10.1007/s00106-021-01000-9
Adamske D, Heyduck A, Weidenmüller M, Göricke B, Frank T, Olthoff A (2021) Dysphagia in amyotrophic lateral sclerosis: Quantification of bulbar motor dysfunction. J Oral Rehabil 48(9):1044–1049. https://doi.org/10.1111/joor.13220
Gosselt IK, Nijboer TCW, Van Es MA (2020) An overview of screening instruments for cognition and behavior in patients with ALS: selecting the appropriate tool for clinical practice. Amyotroph Lateral Scler Frontotemporal Degener 21(5–6):324–336. https://doi.org/10.1080/21678421.2020.1732424
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
We confirm that we have read the journal’s position on issues involved in ethical publication and affirm that this study is consistent with those guidelines.
Informed consent
Informed consent was preliminarily obtained from all patients and controls before their inclusion in the study.
Financial disclosure and conflict of interest
None of the authors has any financial and conflict of interest to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xia, X., Zhang, W., Guo, J. et al. Diagnostic utility of different dysphagia screening tools to detect dysphagia in individuals with amyotrophic lateral sclerosis. Neurol Sci 44, 3919–3927 (2023). https://doi.org/10.1007/s10072-023-06918-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-06918-2