Abstract
Background
Annualized relapse rate (ARR) is used as an outcome measure in multiple sclerosis (MS) clinical trials. Previous studies demonstrated that ARR has reduced in placebo groups between 1990 and 2012. This study aimed to estimate real-world ARRs from contemporary MS clinics in the UK, in order to improve the feasibility estimations for clinical trials and facilitate MS service planning.
Methods
A multicentre observational, retrospective study of patients with MS from 5 tertiary neuroscience centres in the UK. We included all adult patients with a diagnosis of MS that had a relapse between 01/04/2020 and 30/06/2020.
Results
One hundred thirteen out of 8783 patients had a relapse during the 3-month study period. Seventy-nine percent of the patients with a relapse were female, the mean age was 39 years, and the median disease duration was 4.5 years; 36% of the patients that had a relapse were on disease-modifying treatment. The ARR from all study sites was estimated at 0.05. The ARR for relapsing remitting MS (RRMS) was estimated at 0.08, while the ARR for secondary progressive MS (SPMS) was 0.01.
Conclusions
We report a lower ARR compared to previously reported rates in MS.
Similar content being viewed by others
Introduction
Relapses are one of the clinical hallmarks of multiple sclerosis (MS) that can affect disability at least in the short term [1]. Although relapses are the cardinal feature of relapsing remitting MS (RRMS), they are also present in progressive MS. Understanding the role of MS relapses has been challenging, as they are not constant over time [2]; they tend to be more common at the early stages of the disease and in younger female patients [1, 3]. The most robust estimation of relapse incidence originates from clinical trials. In most of the clinical phase-3 placebo-controlled trials in MS, relapse incidence, measured by the annualized relapse rate (ARR), is used as the primary or secondary efficacy outcome measure [4,5,6,7,8,9,10]. ARR is a critical component in calculating sample size estimation, and hence feasibility of clinical trials [9, 10]. Between 1990 and 2012, a trend of lower ARR over time has been reported in previous studies [4,5,6,7, 9, 11].
The aim of this study was to estimate the real-world ARRs from contemporary MS clinics in the UK, in order to improve the feasibility estimations for clinical trials [7] and facilitate MS service planning [12].
Materials and methods
Patients and methods
This was a multicentre observational, retrospective study of patients with MS from 5 tertiary neuroscience centres in the UK; this provided a geographical spread of hospital clinics across England and Wales. The study received a favourable ethical opinion from the East Midland – Derby Research Ethics Committee (21/EM/0133).
We included patients with the following criteria: (i) diagnosis of clinically definite MS according to the revised McDonald criteria [13], (ii) age above 18 years. All relapses between 01/04/2020 and 30/06/2020 were included. In order to exclude any bias caused by the COVID-19 pandemic, we validated the results, by also recording all relapses occurring in the same quarter of 2019. A relapse was defined as a significant worsening of symptoms or the appearance of new neurological symptoms, lasting more than 24 h and occurring at least 30 days after the onset of a preceding event, in the absence of fever or infection [14, 15].
Data collection
Demographic details and clinical characteristics were obtained from hospital medical records. Data was collected for patient sex, age at the time of relapse, MS subtype, disease duration, and disease-modifying treatment (DMT) exposure. The methods of data collection for each study site are listed below. All possible relapses detected at each site were reviewed by a neurology consultant with expertise in MS to determine whether it was an actual relapse or not.
Nottingham University Hospitals NHS Trust
We screened by alphabetical order the first 850 out of total 3684 (25.12%) patients that were registered on the Nottingham University Hospitals MS clinic (using iMED MS database). For these patients, we reviewed all hospital medical records, emergency department visits, and MS nurse telephone records for any indication of a possible relapse during the study period. Medical records were screened from April 2019 until December 2020, to identify relapses which occurred during the study period, but were reported in later clinic appointments.
University Hospitals Coventry and Warwickshire NHS Trust
We screened the total MS population (2779 patients) that were registered on the dendrite MS database and extracted all the patients that had a “relapse assessment” entry on the database during the study period. We also screened nursing notes and identified patients that contacted the MS nurse with a “possible relapse”, marked as the reason for nursing contact.
Aneurin Bevan University Health Board (Newport)
We extracted all phone call encounters from the entire MS population (1316 patients) that were registered on the PatientCare database during the study period. Phone call records were searched using the terms “relapse”, “relapsing”, and “steroid”. Relapses already recorded on the database during the study period were also extracted. We reviewed the medical records of all patients picked up by this search, as well as patients that attended the relapse clinic.
Cardiff and Vale University Health Board
We extracted all phone call encounters from the entire MS population (1834 patients) that were registered on the PatientCare database during the study period. Phone call records were searched using the terms “relapse”, “relapsing”, “Rapid Access Clinic (RAC)”, and “steroid”. Relapses already recorded on the database during the study period were also extracted. We reviewed the medical records of all patients picked up by this search, as well as patients that attended the rapid access clinic (RAC).
Swansea Bay University Health Board
We reviewed the medical records from all relapse clinics during the study period for the entire MS population (2004 patients). Telephone logs, email trails, and multidisciplinary team discussions relating to possible relapses or hospital admissions were also reviewed.
Statistical analysis
MS populations across sites were reviewed for confirmed relapses within the same 3-month follow-up period. The estimated number of relapses per year was calculated by quadrupling the 3-month figures; crude ARRs were generated using the person-years method, by dividing the yearly number of relapses by the total MS population in each centre [16].
Summary statistics are reported as means or medians with standard deviation or range as appropriate. For statistical estimates, 95% confidence intervals are provided. Two-sided p-values < 0.05 were considered statistically significant. In order to explore the effect of (a) the study year, (b) the study site, and (c) the MS subtype on relapses, we performed a negative binomial regression analysis. We modelled ARRs using negative binomial regression and have reported the incidence (relapse) rate ratio for the groups: year, disease subtype, and location. We selected a negative binomial distribution model because data were over-dispersed when we applied a Poisson distribution [16]. All analysis was conducted in the software for statistics and data science, Stata 14 [17].
Results
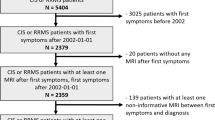
Table 1 shows the MS subtypes and number of patients on DMT for the entire population screened for this study.
We screened in total 8783 patients with MS from all sites. Twenty-seven percent of the total number of patients were on DMT (44% of RRMS, 9% of secondary progressive MS (SPMS), 4% of primary progressive MS (PPMS), and 1% of clinically isolated syndrome (CIS)). Between study sites, 70% of RRMS patients in Nottingham were on DMT, followed by 46% in Swansea, 42% in Cardiff, 40% in Coventry, and 29% in Newport. The relatively small percentage of RRMS patients on DMT can be (at least partly) explained by the strict DMT initiation criteria that apply in the UK (e.g. for first-line DMTs, patients should have 2 clinically significant relapses within a 2-year period).
We identified 113 patients that had a relapse during the 3 months study period in 2020.
Table 2 demonstrates the demographic and clinical characteristics of patients that had a relapse, with the estimated ARRs.
The total ARR from all study sites was estimated at 0.05, which was similar (0.06) to the 2019 group. The highest ARR was reported for Nottingham (0.14). Cardiff had an ARR of 0.06, followed by Newport (0.05), Coventry (0.04), and Swansea (0.03). While there appears to be a decreased number of relapses in 2020 compared to 2019, the regression analysis (Table 3) did not reveal any effect of the year to the relapses. Therefore, it seems unlikely that the reported relapses were increased during the COVID-19 pandemic. Using the same statistical model, we found that all study sites recorded significantly lower relapses compared to Nottingham (Table 3). Patients with RRMS had a significant higher risk of relapse compared to PPMS and SPMS, but not compared to CIS (Table 3).
Table 4 demonstrates the estimated ARRs for the total number of RRMS and SPMS patients, including patients on DMTs.
The ARR for all RRMS patients and for RRMS patients on DMT was 0.08; both results were comparable to 2019. The ARR for all SPMS patients was estimated at 0.01, while the ARR for SPMS patients on DMT was 0.16.
Discussion
In this observational real-world multicentre UK study, we found a lower ARR compared to current knowledge for ARRs in MS. Despite many MS clinical trials incorporating additional measures of disability progression into their study endpoints like MRI lesions, brain atrophy, disability progression, and cognitive decline, the ARR remains important for feasibility estimations of clinical trials. The overall ARR of 0.05 is much lower compared to the ARRs reported in two previous UK studies 7–8 years ago [12, 18]. Duddy et al. reported a rate of 0.36, but this relied on patient-reported questionnaires, rather than clinician-confirmed relapses [18]. Nevertheless, another UK study based on commissioning data from Cardiff and Vale population in Wales estimated a very similar ARR of 0.37 [12]. A further study based on a patient survey in 2017 across the USA revealed that 44.1% of MS patients had < 1 relapse per year, 35.5% had 1–2 relapses, and 20.2% had > 2 relapses per year [2].
The ARR for RRMS patients (0.08) as well as the ARR for RRMS patients on DMT (0.08) was also lower compared to previously reported ARRs from randomised controlled trials in RRMS [19]. It was first noted that the ARRs for the placebo group in the fingolimod and cladribine trials from 2010 were 0.4 and 0.33 respectively, which was significantly lower compared to the 0.9 and 1.28 that were found in interferon beta-1a trials in the 1990s [11]. This finding attracted further research; a comprehensive literature review by Inusah et al. found a mean ARR of 0.68 for the treatment group, while the mean ARR for the placebo group was 1.005 [6]. It also demonstrated a sustained reduction of the ARR by 0.36 relapses per year over a 10-year study period for the placebo group and 0.37 for the treatment group [6]. Similarly, Nicholas et al. found that the ARR for the placebo group decreased by 6.2% per year, translating to a reduction of almost 50% over 10 years [7]. Comparable results were found by Steinvorth et al., with a reduction in the ARR of the placebo group by 4.5% per year [9].
Higher ARRs compared to our findings were also reported in a recent meta-analysis of the efficacy and safety of monoclonal antibody therapies for RRMS; it showed an ARR of 0.45 for the patients that were on interferon beta-1a, which was the most common comparison treatment [20]; the ARRs for the preceding year varied from 1.2 to 3.0 [20]. Equally high ARR (> 1) was noted for RRMS patients in the year before enrolment to ofatumumab trials [21]. The ARRs in the ofatumumab and teriflunomide groups were 0.11 and 0.22 in trial 1 and 0.10 and 0.25 in trial 2 [21].
Our study findings suggest that the previously noted trend of reducing ARRs in RRMS [4, 6, 7, 9, 10] continues. It is plausible that the recent increased availability of higher efficacy DMTs can explain the reduced ARRs for the RRMS patients. Moreover, the ARR in all our RRMS patients versus RRMS patients on DMT was the same (0.08), supporting the findings from another study, which reported that prior DMT use did not influence on-trial ARRs [11]. Previous studies found that age, disease duration, pre-trial ARR, number of years used to calculate pre-trial ARR, and study duration were the main determinants of the on-study ARRs [4, 6, 9, 11]. Mean disease duration and age were comparable with previous studies [4, 6, 9, 11, 20]; hence, we do not feel that they have influenced the low ARRs in this cohort.
We found differences in the relapse rates between different study sites. Nottingham had a higher ARR compared to other sites. This is more likely to be due to our data extraction methodology. Nottingham was the only centre that screened all medical records from April 2019 until the end of December 2020 to capture all relapses, including the relapses that were reported retrospectively in future clinic appointments. All other sites extracted their data from databases/phone call encounters/relapse clinics from April to June 2020 and for the same period in 2019.
In contrast to RRMS [4, 6,7,8,9, 11], there have not been many studies reporting the relapse rates of SPMS patients; this is at least partly due to the small number of randomised controlled trials for DMTs in SPMS. The ARR reported in the Expand study for SPMS patients at baseline was 0.16 on the placebo group versus 0.07 on siponimod [22]; in the year before screening, the ARR was 0.2 for patients randomised for siponimod and 0.3 for placebo [22]. The previous European interferon beta-1b study in SPMS found an on-study ARR of 0.64 for the placebo group [23], while the US study reported an ARR of 0.28 [23]. A recent study from Switzerland analysing the cost-effectiveness of siponimod compared to interferon beta-1a in SPMS patients estimated that the annual relative risk of a relapse was 0.5 for siponimod versus placebo and 0.69 for interferon beta-1a versus placebo [24]. Another recent study of SPMS patients from France found that 10–15% of patients had at least one relapse in a year, during the first 5 years of progression [25].
Total ARR for our SPMS patients was estimated at 0.01, which is lower compared to previous studies [22,23,24,25]. However, the total ARR for SPMS patients on DMT was 0.16 with Nottingham reporting an ARR of 0.25, which are comparable with the ARRs reported in the Expand study [22].
This study has the limitations of a retrospective design and a relatively small sample, especially for the SPMS patients; this resulted in three of the study sites (Cardiff, Swansea, and Newport) not detecting any relapses in their SPMS patients on DMT during the 3-month study period. Unfortunately, due to the lack of availability across all centres, we were unable to report the type of DMTs that could have provided a possible explanation of the differences between centres. Moreover, there were differences in the data collection methodology between study sites. Our methodology would have captured all relapses reported to the MS clinics but would have missed any mild relapses which were unreported to secondary care. Finally, while we report the crude ARR, we a priori decided not to calculate the adjusted ARRs, due to unavailability of clinically meaningful data, although this would have been advantageous in order to directly assess additional factors influencing relapse frequencies. In conclusion, we report a multicentre UK study that estimated real-world ARRs from contemporary MS clinics and provided a broader and different perspective to current knowledge derived from clinical trials. We found that the previously reported trend of reducing ARRs in RRMS 10 years ago [4, 6, 7, 9, 11] continues to decline. Moreover, the recent UK approval of siponimod in SPMS [26] increased the need of obtaining a contemporary ARR for SPMS patients, which we tried to address in this study; we report a reduced ARR in SPMS compared to previous studies [22,23,24,25]. Further larger prospective studies are needed with real-world data, to improve the feasibility estimations of future clinical trials and facilitate MS service planning.
References
Tremlett H, Yousefi M, Devonshire V, Rieckmann P, Zhao Y (2009) Impact of multiple sclerosis relapses on progression diminishes with time. Neurology 73(20):1616–1623. https://doi.org/10.1212/WNL.0b013e3181c1e44f
Nazareth TA, Rava AR, Polyakov JL et al (2018) Relapse prevalence, symptoms, and health care engagement: patient insights from the Multiple Sclerosis in America 2017 survey. Mult Scler Relat Disord 26:219–234. https://doi.org/10.1016/j.msard.2018.09.002
Tremlett H, Zhao Y, Joseph J, Devonshire V, the UBCMS Clinic Neurologists. (2008) Relapses in multiple sclerosis are age-and time-dependent. J Neurol Neurosurg Psychiatry 79:1368–1375. https://doi.org/10.1136/jnnp.2008.145805
Nicholas R, Straube S, Schmidli H, Pfeiffer S, Friede T (2012) Time-patterns of annualized relapse rates in randomized placebo-controlled clinical trials in relapsing multiple sclerosis: a systematic review and meta-analysis. Mult Scler 18(9):1290–1296. https://doi.org/10.1177/1352458511435715
Lavery AM, Verhey LH, Waldman AT (2014) Outcome measures in relapsing-remitting multiple sclerosis: capturing disability and disease progression in clinical trials. Mult Scler Int 2014:262350. https://doi.org/10.1155/2014/262350
Inusah S, Sormani MP, Cofield SS et al (2010) Assessing changes in relapse rates in multiple sclerosis. Mult Scler 16(12):1414–1421. https://doi.org/10.1177/1352458510379246
Nicholas R, Straube S, Schmidli H, Schneider S, Friede T (2011) Trends in annualized relapse rates in relapsing-remitting multiple sclerosis and consequences for clinical trial design. Mult Scler 17(10):1211–1217. https://doi.org/10.1177/1352458511406309
Li H, Hu F, Zhang Y, Li K (2020) Comparative efficacy and acceptability of disease-modifying therapies in patients with relapsing–remitting multiple sclerosis: a systematic review and network meta-analysis. J Neurol 267(12):3489–3498. https://doi.org/10.1007/s00415-019-09395-w
Steinvorth SM, Röver C, Schneider S, Nicholas R, Straube S, Freide T (2013) Explaining temporal trends in annualised relapse rates in placebo groups of randomised con trolled trials in relapsing multiple sclerosis: systematic review and meta-regression. Mult Scler 19(12):1580–1586. https://doi.org/10.1177/1352458513481009
Poncet-Megemont L, Pereira B, Rollot F et al (2021 Oct) Estimation of sample size in randomized controlled trials in multiple sclerosis studying annualized relapse rates: a systematic review. Mult Scler 26:13524585211052400. https://doi.org/10.1177/13524585211052400
Stellmann J-P, Neuhaus A, Herich L et al (2012) Placebo cohorts in phase-3 MS treatment trials-predictors for on-trial disease activity 1990-2010 based on a meta-analysis and individual case data. PLoS One 7(11):e50347. https://doi.org/10.1371/journal.pone.0050347
Tallantyre EC, Wardle M, Robertson NP (2016) How to run a multiple sclerosis relapse clinic. Pract neurol 16:62–69. https://doi.org/10.1136/practneurol-2015-001214
Thompson AJ, Banwell BL, Barkhof F et al (2018) Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol 17:162–173. https://doi.org/10.1016/S1474-4422(17)30470-2
Poser CM, Paty DW, Scheinberg L et al (1983) New diagnostic criteria for multiple sclerosis: guidelines for research protocols. Ann Neurol 13:227–231. https://doi.org/10.1002/ana.410130302
Lublin FD, Reingold SC, Cohen JA et al (2014) Defining the clinical course of multiple sclerosis: the 2013 revisions. Neurology 83:278–286. https://doi.org/10.1212/WNL.0000000000000560
Akaishi T, Ishii T, Aoki M et al (2022) Calculating and comparing the annualized relapse rate and estimating the confidence interval in relapsing neurological diseases. Front Neurol 13:875456. https://doi.org/10.3389/fneur.2022.875456
StataCorp. (2015) Stata statistical software: release 14. StataCorp LP, College Station, TX
Duddy M, Lee M, Pearson O et al (2014) The UK experience of relapse in multiple sclerosis treated with first disease modifying therapies. Mult Scler Relat Disord 3(4):450–456. https://doi.org/10.1016/j.msard.2014.02.006
Kalincik T (2015) Multiple sclerosis relapses: epidemiology, outcomes and management. A Systematic Review. Neuroepidemiology 44:199–214. https://doi.org/10.1159/000382130
Xu X, Chi S, Wang Q et al (2018) Efficacy and safety of monoclonal antibody therapies for relapsing remitting multiple sclerosis: a network meta-analysis. Mult Scler Relat Disor 25:322–328. https://doi.org/10.1016/j.msard.2018.08.026
Hauser SL, Bar-Or A, Cohen JA et al (2020) Ofatumumab versus Teriflunomide in Multiple Sclerosis. N Engl J Med 383(6):546–557. https://doi.org/10.1056/NEJMoa1917246
Kappos L, Bar-Or A, Cree BAC et al (2018) Siponimod versus placebo in secondary progressive multiple sclerosis (EXPAND): a double-blind, randomised, phase 3 study. Lancet 391(10127):1263–1273. https://doi.org/10.1016/S0140-6736(18)30475-6
Kappos L, Weinshenker B, Pozzilli C et al (2004) Interferon beta-1b in secondary progressive MS: a combined analysis of the two trials. Neurology 63:1779–1787. https://doi.org/10.1212/01.WNL.0000145561.08973.4F
Schur N, Gudala K, Vudumula U et al (2021) Cost Effectiveness and budget impact of siponimod compared to interferon Beta-1a in the treatment of adult patients with secondary progressive multiple sclerosis with active disease in Switzerland. Pharmacoeconomics 39(5):563–577. https://doi.org/10.1007/s40273-021-01023-8
Mathey G, Ancel T, Garot T et al (2021) Clinical and radiological activity of secondary progressive multiple sclerosis in a population-based cohort. Eur J Neurol 28(7):2238–2248. https://doi.org/10.1111/ene.14861
NICE (2020). Siponimod for treating secondary progressive multiple sclerosis. Retrieved October 22, 2021, from NICE: https://www.nice.org.uk/guidance/ta656/resources/siponimod-for-treating-secondary-progressive-multiple-sclerosis-pdf-82609202014405
Funding
NE received educational support for this project from Roche Products Limited (donation #Jan2021-002).
Author information
Authors and Affiliations
Contributions
Conceptualization: NE
Methodology: AP, AH, ET, KH, TA, GI, GRL, NE
Formal analysis: GRL
Data curation: AP, AH, ET, KH, APS, MM, CQ, MT, TA, GI, GRL
Writing original draft: AP, AH, ET, KH, APS, TA, GI, GRL, NE
Writing—review and editing: AP, AH, ET, KH, APS, MM, CQ, MT, TA, GI, GRL, NE
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declared the following potential conflicts of interest with respect to the research, authorship and/or publication of this article. AP, AH, APS, MM, CQ, MT, and GRL have nothing to declare. KH reports speaker and personal fees from Roche, Merck, and Biogen, and travel grants to attend educational meetings from Roche, Novartis, Merck, and Biogen. ET reports speaker fees and honoraria from Biogen, Janssen, Merck, Novartis, and Takeda, Roche, and travel expenses to attend educational meetings from Biogen, Merck, and Roche. TA has received speaker fees, support for scientific meetings and honoraria for advisory work from Merck Serono, Novartis, Roche, and Genzyme. G.I has received honoraria and travel expenses from Biogen, Merck, Novartis, and Roche and has served on advisory boards/acted as a speaker for Biogen, Novartis, Merck, and Roche. NE reports speaker fees and honoraria from Biogen, Merck, Novartis, and Roche.
Ethical approval and informed consent
Informed consent was not recived for this study; a favourable ethical opinion was received from the East Midland–Derby Research Ethics Committee (21/EM/0133).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Papathanasiou, A., Hibbert, A., Tallantyre, E. et al. Real-world annualized relapse rates from contemporary multiple sclerosis clinics in the UK: a retrospective multicentre cohort study. Neurol Sci 44, 3629–3635 (2023). https://doi.org/10.1007/s10072-023-06838-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-06838-1