Abstract
Background
Parkinson’s disease (PD) is one of the common causes of disability in the elderly. This study aims to estimate the prevalence of hallucinations in Parkinson’s patients in the world.
Methods
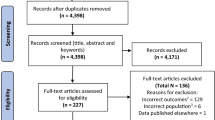
A systematic review of PubMed/Medline, ISI Web of Knowledge, and Google Scholar was conducted from 2017 to 2022. This study investigated the prevalence of hallucinations in Parkinson’s patients. Point prevalence was analyzed with a 95% confidence interval. The variances of each study were calculated using the binomial distribution formula The researcher used Cochrane Q-test with a significance level of less than 0.1 to check the heterogeneity between studies and the change index assigned to heterogeneity I2. Due to the heterogeneity between the studies, the random effects model was used to combine the results of the studies. All statistical analyses were performed by STATA version 14 software using meta-analysis commands.
Results
Reports indicated that the prevalence of hallucinations in Parkinson’s patients in 32 studies was 28% (0.22–0.34 = 95%CI). The highest prevalence was 34% and 95% CI = 0.07– 0.61 in developing countries and 27% with CI = 0.33–0.21 in developed countries. Reports showed the prevalence in men was 30% (CI = 0.22–0.38) and in women 23% (95% CI = 0.14–0.31).
Conclusions
Considering the relatively high prevalence of hallucinations in these patients, checking up for the presence of hallucinations on every visit of Parkinson’s patients is recommended, and providing appropriate treatment for that is necessary.


Similar content being viewed by others
References
Hosseinabadi R, Sheibanizadeh A, Shahidi M (2009) Comparison of equilibrium deficits in idiopathic Parkinson’s disease with normal subjects using videonystagmography. J Babol Univ Med Sci 11(1):36–40
Hely MA, Reid WG, Adena MA, Halliday GM, Morris JG (2008) The Sydney multicenter study of Parkinson’s disease: the inevitability of dementia at 20 years. Mov Disord 23(6):837–844
De Rijk Md, Launer L, Berger K, Breteler M, Dartigues J, Baldereschi M et al (2000) Prevalence of Parkinson’s disease in Europe: a collaborative study of population-based cohorts Neurologic Diseases in the Elderly Research Group. Neurology 54(11 Suppl 5):21–3
Fénelon G (2008) Psychosis in Parkinson’s disease: phenomenology, frequency, risk factors, and current understanding of pathophysiologic mechanisms. CNS Spectr 13(S4):18–25
Omoto S, Murakami H, Shiraishi T, Bono K, Umehara T, Iguchi Y (2021) Risk factors for minor hallucinations in Parkinson’s disease. Acta Neurol Scand 143(5):538–544
Ravina B, Marder K, Fernandez HH, Friedman JH, McDonald W, Murphy D et al (2007) Diagnostic criteria for psychosis in Parkinson’s disease: report of an NINDS, NIMH work group. Mov Disord 22(8):1061–1068
Lenka A, Pagonabarraga J, Pal PK, Bejr-Kasem H, Kulisvesky J (2019) Minor hallucinations in Parkinson disease: a subtle symptom with major clinical implications. Neurology 93(6):259–266
Fénelon G, Soulas T, De Langavant LC, Trinkler I, Bachoud-Lévi A-C (2011) Feeling of presence in Parkinson’s disease. J Neurol Neurosurg Psychiatry 82(11):1219–1224
Marinus J, Zhu K, Marras C, Aarsland D, van Hilten JJ (2018) Risk factors for non-motor symptoms in Parkinson’s disease. The Lancet Neurology 17(6):559–568
Vayr F, Martin-Blondel G, Savall F, Soulat J-M, Deffontaines G, Herin F (2018) Occupational exposure to human Mycobacterium bovis infection: a systematic review. PLoS Negl Trop Dis 12(1):e0006208
Radojević B, Dragašević-Mišković NT, Marjanović A, Branković M, Dobričić V, Milovanović A, et al. Clinical and genetic analysis of psychosis in Parkinson’s disease. J Parkinson's Dis 2021;(1):1–8
Schwertner E, Pereira JB, Xu H, Secnik J, Winblad B, Eriksdotter M, et al. Behavioral and psychological symptoms of dementia in different dementia disorders: a large-scale study of 10,000 individuals. J Alzheimer's Dis 2022;(Preprint):1–12
Merola A, Romagnolo A, Dwivedi AK, Padovani A, Berg D, Garcia-Ruiz PJ et al (2020) Benign versus malignant Parkinson disease: the unexpected silver lining of motor complications. J Neurol 267(10):2949–2960
Panisset M, Stril J-L, Bélanger M, Lehoux G, Coffin D, Chouinard S (2016) Open-label study of sleep disturbances in patients with Parkinson’s disease treated with Rasagiline. Can J Neurol Sci 43(6):809–814
Tarolli CG, Zimmerman GA, Auinger P, McIntosh S, Horowitz RK, Kluger BM et al (2020) Symptom burden among individuals with Parkinson disease: a national survey. Neurol: Clin Pract 10(1):65–72
Russillo MC, Andreozzi V, Erro R, Picillo M, Amboni M, Cuoco S et al (2022) Sex differences in Parkinson’s disease: from bench to bedside. Brain Sci 12(7):917
Martinez-Ramirez D, Okun MS, Jaffee MS (2016) Parkinson’s disease psychosis: therapy tips and the importance of communication between neurologists and psychiatrists. Neurodegener Dis Manag 6(4):319–330
Weil RS, Reeves S (2020) Hallucinations in Parkinson’s disease: new insights into mechanisms and treatments. Adv Clin Neurosci Rehabil: ACNR 19(4):ONNS5189
Banerjee AK, Falkai PG, Savidge M (1989) Visual hallucinations in the elderly associated with the use of levodopa. Postgrad Med J 65(764):358–361
Funakawa I, Jinnai K (2005) Tactile hallucinations induced by trihexyphenidyl in a patient with Parkinson’s disease. Rinsho Shinkeigaku = Clin Neurol 45(2):125–7
Postma J, Van Tilburg W (1975) Visual hallucinations and delirium during treatment with amantadine (Symmetrel). J Am Geriatr Soc 23(5):212–215
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the Ethics Committee of Kashan University of Medical Sciences, Kashan, Iran, and conducted under number (IR.KAUMS.NUHEPM.REC.1402.001).
Conflict of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ravandi, S.N., Kouchaki, E. & Asgarian, F.S. Prevalence of hallucinations in Parkinson’s patients: meta-analysis of International studies. Neurol Sci 44, 3389–3394 (2023). https://doi.org/10.1007/s10072-023-06831-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-06831-8