Abstract
Background
Trunk stabilization, which is a factor that directly affects the performance of affected upper-limb movements in stroke patients, is of critical importance in the performance of selective motor control.
Aims
This study aimed to investigate the effects on upper-limb motor function of the addition of robotic rehabilitation (RR) and conventional rehabilitation (CR) to intensive trunk rehabilitation (ITR).
Methods
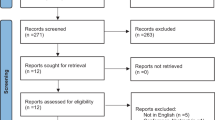
A total of 41 subacute stroke patients were randomly allocated to two groups: RR and CR. Both groups received the same ITR procedure. Following ITR, a robot-assisted rehabilitation program of 60 min, 5 days a week, for 6 weeks, was applied to the RR group, and an individualized upper-limb rehabilitation to the CR group. Assessments were made at baseline and after 6 weeks using the Trunk Impairment Scale (TIS), Fugl-Meyer Upper Extremity Motor Evaluation Scale (FMA-UE), and Wolf Motor Function Test (WMFT).
Results
Improvements were obtained in the TIS, FMA-UE, and WMFT scores for both groups (p < 0.001), with no superiority detected between the groups (p > 0.05). The RR group scores were relatively high, but not to a statistically significant.
Conclusions
When added to intensive trunk rehabilitation, the robot-assisted systems, which are recommended as a stand-alone therapy method, produced similar results to conventional therapies. This technology can be used as an alternative to conventional methods under appropriate conditions of clinical opportunity, access, time management, and staff limitations. However, when RR is combined with traditional interventions such as intensive trunk rehabilitation, it is essential to investigate if the real effect is due to the robotic rehabilitation or the accumulation of positive effects of excessive movement or force spread associated with trained muscles.
Registration
This trial was retrospectively registered in the ClinicalTrials.gov with NCT05559385 registration number (25/09/2022).

Similar content being viewed by others
References
Cho KH, Song WK (2015) Robot-assisted reach training for improving upper extremity function of chronic stroke. Tohoku J Exp Med 237:149–155. https://doi.org/10.1620/tjem.237.149
Feigin VL, Norrving B, Mensah GA (2017) Global burden of stroke. Circ Res 120:439–448
Ünal A, Altuğ F, Duray M, Cavlak U (2018) Impact of stroke on balance ability and postural sway: a comparative study. Neurorehabil Neural Repair 32:407–408
Patten C, Lexell J, Brown HE (2004) Weakness and strength training in persons with poststroke hemiplegia: rationale, method, and efficacy. J Rehabil Res Dev 41:293–312
Tyson SF, Hanley M, Chillala J et al (2008) Sensory loss in hospital-admitted people with stroke: characteristics, associated factors, and relationship with function. Neurorehabil Neural Repair 22:166–172. https://doi.org/10.1177/1545968307305523
Sampaio-Baptista C, Sanders ZB, Johansen-Berg H (2018) Structural plasticity in adulthood with motor learning and stroke rehabilitation. Annu Rev Neurosci 41:25–40
Carmichael ST (2006) Cellular and molecular mechanisms of neural repair after stroke: making waves. Ann Neurol 59:735–742
Dancause N, Barbay S, Frost SB et al (2005) Extensive cortical rewiring after brain injury. J Neurosci 25:10167–10179. https://doi.org/10.1523/JNEUROSCI.3256-05.2005
Levin MF, Demers M (2021) Motor learning in neurological rehabilitation. Disabil Rehabil 43:3445–3453
Masiero S, Armani M, Ferlini G et al (2014) Randomized trial of a robotic assistive device for the upper extremity during early inpatient stroke rehabilitation. Neurorehabil Neural Repair 28:377–386. https://doi.org/10.1177/1545968313513073
Langan J, Van Donkelaar P (2008) The influence of hand dominance on the response to a constraint-induced therapy program following stroke. Neurorehabil Neural Repair 22:298–304. https://doi.org/10.1177/1545968307307123
Arslan SA, Uğurlu K, Demirci C, Keskin D (2021) Investigating the relation between upper extremity function and trunk control, balance and functional mobility in individuals with stroke. J Heal Sci Med 4:127–131. https://doi.org/10.32322/jhsm.830398
Kang MG, Yun SJ, Lee SY, et al (2020) Effects of upper-extremity rehabilitation using smart glove in patients with subacute stroke: results of a prematurely terminated multicenter randomized controlled trial. Front Neurol 11:. https://doi.org/10.3389/fneur.2020.580393
Park JH, Park G, Kim HY, et al (2020) A comparison of the effects and usability of two exoskeletal robots with and without robotic actuation for upper extremity rehabilitation among patients with stroke: a single-blinded randomised controlled pilot study. J Neuroeng Rehabil 17:. https://doi.org/10.1186/s12984-020-00763-6
Yildiz A, Mustafaoglu R, Caglayan F, Kesiktas FN (2019) Investigation of the effect of upper extremity robotic rehabilitation approach on respiratory muscle strength in stroke. Eur Respir J 54:. https://doi.org/10.1183/13993003.congress-2019.pa3960
Liao WW, Wu CY, Hsieh YW et al (2012) Effects of robot-assisted upper limb rehabilitation on daily function and real-world arm activity in patients with chronic stroke: a randomized controlled trial. Clin Rehabil 26:111–120. https://doi.org/10.1177/0269215511416383
Lee MJ, Lee JH, Lee SM (2018) Effects of robot-assisted therapy on upper extremity function and activities of daily living in hemiplegic patients: a single-blinded, randomized, controlled trial. Technol Heal Care 26:659–666. https://doi.org/10.3233/THC-181336
Gladstone DJ, Danells CJ, Black SE (2002) The Fugl-Meyer assessment of motor recovery after stroke: a critical review of ıts measurement properties. Neurorehabil Neural Repair 16:232–240
Wolf SL, Lecraw DE, Barton LA, Jann BB (1989) Forced use of hemiplegic upper extremities to reverse the effect of learned nonuse among chronic stroke and head-injured patients. Exp Neurol 104:125–132. https://doi.org/10.1016/S0014-4886(89)80005-6
Morris DM, Uswatte G, Crago JE et al (2001) The reliability of the wolf motor function test for assessing upper extremity function after stroke. Arch Phys Med Rehabil 82:750–755. https://doi.org/10.1053/apmr.2001.23183
Verheyden G, Nieuwboer A, Mertin J et al (2004) The Trunk Impairment Scale: a new tool to measure motor impairment of the trunk after stroke. Clin Rehabil 18:326–334. https://doi.org/10.1191/0269215504cr733oa
Chung EJ, Kim JH, Lee BH (2013) The effects of core stabilization exercise on dynamic balance and gait function in stroke patients. J Phys Ther Sci 25:803–806. https://doi.org/10.1589/jpts.25.803
Haruyama K, Kawakami M, Otsuka T (2017) Effect of core stability training on trunk function, standing balance, and mobility in stroke patients: a randomized controlled trial. Neurorehabil Neural Repair 31:240–249. https://doi.org/10.1177/1545968316675431
Çapık C (2014) İstatistiksel Güç Analizi ve Hemşirelik Araştırmalarında Kullanımı: Temel Bilgiler. J Anatolia Nurs Heal Sci 17:268–274
Wee SK, Hughes AM, Warner MB et al (2015) Effect of trunk support on upper extremity function in people with chronic stroke and people who are healthy. Phys Ther 95:1163–1171. https://doi.org/10.2522/ptj.20140487
Wee SK, Hughes AM, Warner M, Burridge JH (2014) Trunk restraint to promote upper extremity recovery in stroke patients: a systematic review and meta-analysis. Neurorehabil Neural Repair 28:660–677. https://doi.org/10.1177/1545968314521011
Rosenblum S, Josman N (2003) The relationship between postural control and fine manual dexterity. Phys Occup Ther Pediatr 23:47–60. https://doi.org/10.1300/J006v23n04_04
Yang SH, Chung EJ, Lee J, et al (2021) The effect of trunk stability training based on visual feedback on trunk stability, balance, and upper limb function in stroke patients: a randomized control trial. Healthcare 9:. https://doi.org/10.3390/healthcare9050532
Olczak A, Truszczyńska-Baszak A (2021) Influence of the passive stabilization of the trunk and upper limb on selected parameters of the hand motor coordination, grip strength and muscle tension, in post-stroke patients. J Clin Med 10:. https://doi.org/10.3390/jcm10112402
Woodbury ML, Howland DR, McGuirk TE et al (2009) Effects of trunk restraint combined with intensive task practice on poststroke upper extremity reach and function: a pilot study. Neurorehabil Neural Repair 23:78–91. https://doi.org/10.1177/1545968308318836
Kim J-W, Kim J-H, Lee B-H (2020) Effects of virtual reality-based core stabilization exercise on upper extremity function, postural control, and depression in persons with stroke. Phys Ther Rehabil Sci 9:131–139. https://doi.org/10.14474/ptrs.2020.9.3.131
Ejraei N, Ozer AY (2022) Trunk stabilization and ıts rehabilitative effects in children with cerebral palsy. Abant Med J 11:123–131
Lee PY, Huang JC, Tseng HY et al (2020) Effects of trunk exercise on unstable surfaces in persons with stroke: a randomized controlled trial. Int J Environ Res Public Health 17:1–12. https://doi.org/10.3390/ijerph17239135
Michaelsen SM, Dannenbaum R, Levin MF (2006) Task-specific training with trunk restraint on arm recovery in stroke: randomized control trial. Stroke 37:186–192. https://doi.org/10.1161/01.STR.0000196940.20446.c9
Jakob I, Kollreider A, Germanotta M et al (2018) Robotic and sensor technology for upper limb rehabilitation. PM R 10:S189–S197
Riener R, Nef T, Colombo G (2005) Robot-aided neurorehabilitation of the upper extremities. Med Biol Eng Comput 43:2–10
Hsu HY, Yang KC, Yeh CH et al (2021) A Tenodesis-Induced-Grip exoskeleton robot (TIGER) for assisting upper extremity functions in stroke patients: a randomized control study. Disabil Rehabil 44:7078–7086. https://doi.org/10.1080/09638288.2021.1980915
Di Marco R, Rubega M, Lennon O, et al (2021) Experimental protocol to assess neuromuscular plasticity induced by an exoskeleton training session. Methods Protoc 4:. https://doi.org/10.3390/mps4030048
Aprile I, Germanotta M, Cruciani A et al (2020) Upper limb robotic rehabilitation after stroke: a multicenter, randomized clinical trial. J Neurol Phys Ther 44:3–14. https://doi.org/10.1097/NPT.0000000000000295
Taravati S, Capaci K, Uzumcugil H, Tanigor G (2022) Evaluation of an upper limb robotic rehabilitation program on motor functions, quality of life, cognition, and emotional status in patients with stroke: a randomized controlled study. Neurol Sci 43:1177–1188. https://doi.org/10.1007/s10072-021-05431-8
Lo AC, Guarino PD, Richards LG et al (2010) Robot-assisted therapy for long-term upper-limb ımpairment after stroke. N Engl J Med 362:1772–1783. https://doi.org/10.1056/nejmoa0911341
Daunoraviciene K, Adomaviciene A, Grigonyte A et al (2018) Effects of robot-assisted training on upper limb functional recovery during the rehabilitation of poststroke patients. Technol Health Care 26(S2):533–542. https://doi.org/10.3233/THC-182500
Brackenridge J, Bradnam LV, Lennon S et al (2016) A review of rehabilitation devices to promote upper limb function following stroke. Neurosci Biomed Eng 4:25–42. https://doi.org/10.2174/2213385204666160303220102
Min JH, Seong HY, Ko SH et al (2020) Effects of trunk stabilization training robot on postural control and gait in patients with chronic stroke: a randomized controlled trial. Int J Rehabil Res 43:159–166. https://doi.org/10.1097/MRR.0000000000000399
Adomavičienė A, Daunoravičienė K, Kubilius R, et al (2019) Influence of new technologies on post-stroke rehabilitation: a comparison of Armeo spring to the kinect system. Medicina 55:. https://doi.org/10.3390/medicina55040098
Roman NA, Miclaus RS, Nicolau C, Sechel G (2022) Customized manual muscle testing for post-stroke upper extremity assessment. Brain Sci 12:. https://doi.org/10.3390/brainsci12040457
Eng JJ, Kim CM, MacIntyre DL (2002) Reliability of lower extremity strength measures in persons with chronic stroke. Arch Phys Med Rehabil 83:322–328. https://doi.org/10.1053/apmr.2002.29622
Lodha N, Patel P, Casamento-Moran A et al (2019) Strength or motor control: what matters in high-functioning stroke? Front Neurol 9:1160. https://doi.org/10.3389/fneur.2018.01160
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Marmara University Clinical Research Ethics Committee approved this study with protocol ID: 168 at 06.09.2021.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Şenocak, E., Korkut, E., Aktürk, A. et al. Is the robotic rehabilitation that is added to intensive body rehabilitation effective for maximization of upper extremity motor recovery following a stroke? A randomized controlled study. Neurol Sci 44, 2835–2843 (2023). https://doi.org/10.1007/s10072-023-06739-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-06739-3