Abstract
Introduction
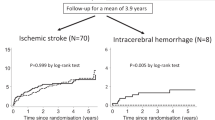
This study is to explore the long-term functional outcome of antihypertensive medication-naïve, untreated hypertension (HTN) patients with acute ischemic stroke compared to those with no prior HTN and those with treated HTN.
Patients and methods
We analyzed a prospectively collected stroke registry of all patients with acute ischemic stroke consecutively admitted to Incheon St. Mary’s Hospital. Patients who received reperfusion therapy were excluded. Long-term functional outcomes were assessed at a 3-month follow-up visit using the modified Rankin Scale.
Results
A total of 1044 patients was enrolled. Compared to patients with no or treated HTN, those with untreated HTN had higher odds for more favorable outcomes (adjusted odds ratio (OR): 1.7 [95% CI: 1.0–2.7, p = 0.050*] and 1.7 [95% CI: 1.0–2.8, p = 0.047*], respectively) when the stroke was large vessel atherosclerosis (LAA)/cardioembolic (CE) with large vessel occlusion/stenosis. However, no such association was observed when there was no large vessel occlusion or stenosis, in total patients, or if the index stroke was related to SVO.
In untreated HTN patients with LAA/CE and large vessel occlusion/stenosis compared to patients in the lowest mean arterial pressure quartile (< 96.7 mmHg), patients in the second and third highest quartiles had higher odds of favorable outcomes.
Conclusions
Patients with untreated HTN had significantly more favorable outcomes at 3 months after ischemic stroke compared to those with no or treated HTN when the stroke was LAA/CE with large vessel occlusion/stenosis. Untreated HTN patients also showed an association between higher MAP and favorable outcomes.



Similar content being viewed by others
Data availability
The de-identified data supporting the findings of this study are available upon reasonable request to the corresponding author.
References
Gaciong Z, Siński M, Lewandowski J (2013) Blood pressure control and primary prevention of stroke: summary of the recent clinical trial data and meta-analyses. Curr Hypertens Rep 15(6):559–574. https://doi.org/10.1007/s11906-013-0401-0
Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, Stoyanovsky V, Antikainen RL, Nikitin Y, Anderson C, Belhani A, Forette F, Rajkumar C, Thijs L, Banya W, Bulpitt CJ (2008) Treatment of hypertension in patients 80 years of age or older. N Engl J Med 358(18):1887–1898. https://doi.org/10.1056/NEJMoa0801369
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, Chalmers J, Rodgers A, Rahimi K (2016) Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 387(10022):957–967. https://doi.org/10.1016/s0140-6736(15)01225-8
World Health Organization (2003) Adherence to long-term therapies : evidence for action / [edited by Eduardo Sabaté]. World Health Organization, Geneva
Ham OK, Yang SJ (2011) Lifestyle factors associated with blood pressure control among those taking antihypertensive medication. Asia Pac J Public Health 23(4):485–495. https://doi.org/10.1177/1010539509347941
Morris AB, Li J, Kroenke K, Bruner-England TE, Young JM, Murray MD (2006) Factors associated with drug adherence and blood pressure control in patients with hypertension. Pharmacotherapy 26(4):483–492. https://doi.org/10.1592/phco.26.4.483
O'Connor PJ (2003) Overcome clinical inertia to control systolic blood pressure. Arch Intern Med 163(22):2677–2678. https://doi.org/10.1001/archinte.163.22.2677
Leonardi-Bee J, Bath PM, Phillips SJ, Sandercock PA (2002) Blood pressure and clinical outcomes in the International Stroke Trial. Stroke 33(5):1315–1320. https://doi.org/10.1161/01.str.0000014509.11540.66
Hong L, Cheng X, Lin L, Bivard A, Ling Y, Butcher K, Dong Q, Parsons M (2019) The blood pressure paradox in acute ischemic stroke. Ann Neurol 85(3):331–339. https://doi.org/10.1002/ana.25428
Zheng L, Sun Z, Li J, Zhang R, Zhang X, Liu S, Li J, Xu C, Hu D, Sun Y (2008) Pulse pressure and mean arterial pressure in relation to ischemic stroke among patients with uncontrolled hypertension in rural areas of China. Stroke 39(7):1932–1937. https://doi.org/10.1161/strokeaha.107.510677
Ahmed N, Wahlgren N, Brainin M, Castillo J, Ford GA, Kaste M, Lees KR, Toni D (2009) Relationship of blood pressure, antihypertensive therapy, and outcome in ischemic stroke treated with intravenous thrombolysis: retrospective analysis from Safe Implementation of Thrombolysis in Stroke-International Stroke Thrombolysis Register (SITS-ISTR). Stroke 40(7):2442–2449. https://doi.org/10.1161/strokeaha.109.548602
Berge E, Cohen G, Lindley RI, Sandercock P, Wardlaw JM, Sandset EC, Whiteley W (2015) Effects of blood pressure and blood pressure-lowering treatment during the first 24 hours among patients in the Third International Stroke Trial of Thrombolytic Treatment for Acute Ischemic Stroke. Stroke 46(12):3362–3369. https://doi.org/10.1161/strokeaha.115.010319
Castillo J, Leira R, García MM, Serena J, Blanco M, Dávalos A (2004) Blood pressure decrease during the acute phase of ischemic stroke is associated with brain injury and poor stroke outcome. Stroke 35(2):520–526. https://doi.org/10.1161/01.Str.0000109769.22917.B0
Ishitsuka K, Kamouchi M, Hata J, Fukuda K, Matsuo R, Kuroda J, Ago T, Kuwashiro T, Sugimori H, Nakane H, Kitazono T (2014) High blood pressure after acute ischemic stroke is associated with poor clinical outcomes: Fukuoka Stroke Registry. Hypertension 63(1):54–60. https://doi.org/10.1161/hypertensionaha.113.02189
Shin JA, Lee KJ, Lee JS, Kang J, Kim BJ, Han MK, Kim JY, Jang MS, Yang MH, Lee J, Gorelick PB, Bae HJ (2020) Relationship between blood pressure and outcome changes over time in acute ischemic stroke. Neurology 95(10):e1362–e1371. https://doi.org/10.1212/wnl.0000000000010203
Tziomalos K, Giampatzis V, Bouziana SD, Spanou M, Papadopoulou M, Kostaki S, Dourliou V, Papagianni M, Savopoulos C, Hatzitolios AI (2015) Elevated diastolic but not systolic blood pressure increases mortality risk in hypertensive but not normotensive patients with acute ischemic stroke. Am J Hypertens 28(6):765–771. https://doi.org/10.1093/ajh/hpu234
Wohlfahrt P, Krajcoviechova A, Jozifova M, Mayer O, Vanek J, Filipovsky J, Cifkova R (2015) Low blood pressure during the acute period of ischemic stroke is associated with decreased survival. J Hypertens 33(2):339–345. https://doi.org/10.1097/hjh.0000000000000414
Bager JE, Hjalmarsson C, Manhem K, Andersson B (2018) Acute blood pressure levels and long-term outcome in ischemic stroke. Brain Behav 8(6):e00992. https://doi.org/10.1002/brb3.992
Qureshi AI (2008) Acute hypertensive response in patients with stroke: pathophysiology and management. Circulation 118(2):176–187. https://doi.org/10.1161/circulationaha.107.723874
Bath PM, Song L, Silva GS, Mistry E, Petersen N, Tsivgoulis G, Mazighi M, Bang OY, Sandset EC (2022) Blood pressure management for ischemic stroke in the first 24 hours. Stroke 53(4):1074–1084. https://doi.org/10.1161/strokeaha.121.036143
Hankey GJ (2003) Angiotensin-converting enzyme inhibitors for stroke prevention: is there HOPE for PROGRESS After LIFE? Stroke 34(2):354–356. https://doi.org/10.1161/01.str.0000054261.97525.4b
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EE 3rd (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24(1):35–41. https://doi.org/10.1161/01.str.24.1.35
Kang DW, Chalela JA, Ezzeddine MA, Warach S (2003) Association of ischemic lesion patterns on early diffusion-weighted imaging with TOAST stroke subtypes. Arch Neurol 60(12):1730–1734. https://doi.org/10.1001/archneur.60.12.1730
Woodhouse LJ, Manning L, Potter JF, Berge E, Sprigg N, Wardlaw J, Lees KR, Bath PM, Robinson TG (2017) Continuing or temporarily stopping prestroke antihypertensive medication in acute stroke: an individual patient data meta-analysis. Hypertension 69(5):933–941. https://doi.org/10.1161/hypertensionaha.116.07982
Helleberg BH, Ellekjær H, Rohweder G, Indredavik B (2014) Mechanisms, predictors and clinical impact of early neurological deterioration: the protocol of the Trondheim early neurological deterioration study. BMC Neurol 14(1):201. https://doi.org/10.1186/s12883-014-0201-4
Martins AI, Sargento-Freitas J, Silva F, Jesus-Ribeiro J, Correia I, Gomes JP, Aguiar-Gonçalves M, Cardoso L, Machado C, Rodrigues B, Santo GC, Cunha L (2016) Recanalization modulates association between blood pressure and functional outcome in acute ischemic stroke. Stroke 47(6):1571–1576. https://doi.org/10.1161/strokeaha.115.012544
Hong KS, Bang OY, Kang DW, Yu KH, Bae HJ, Lee JS, Heo JH, Kwon SU, Oh CW, Lee BC, Kim JS, Yoon BW (2013) Stroke statistics in Korea: part I. Epidemiology and risk factors: a report from the korean stroke society and clinical research center for stroke. J Stroke 15(1):2–20. https://doi.org/10.5853/jos.2013.15.1.2
Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, Chun C, Khang YH, Oh K (2014) Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol 43(1):69–77. https://doi.org/10.1093/ije/dyt228
Kim JS, Bonovich D (2014) Research on intracranial atherosclerosis from the East and west: why are the results different? J Stroke 16(3):105–113. https://doi.org/10.5853/jos.2014.16.3.105
Author information
Authors and Affiliations
Contributions
TK, HC, and JK contributed to conception and design of the study. YDK, SN, YHC, IU, and JWP contributed to the analysis of the data. TK contributed to drafting the text and preparing the tables and figure.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional committee and the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cho, H., Kim, T., Koo, J. et al. Untreated hypertension and prognosis paradox in acute ischemic stroke. Neurol Sci 44, 2087–2095 (2023). https://doi.org/10.1007/s10072-023-06653-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-06653-8