Abstract
Background
Neuromyelitis optica spectrum disorder (NMOSD) is a progressive demyelinating disease of the central nervous system that has overlapping symptoms with multiple sclerosis (MS) but differs from it in a variety of ways. Previous studies have reported conflicting results trying to estimate the number of individuals affected by them which is why we designed this systematic review and meta-analysis to estimate the worldwide prevalence and incidence of NMOSD/NMO based on current evidence.
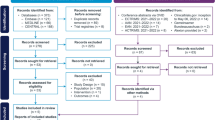
Methods
We searched PubMed, Scopus, EMBASE, Web of Science, and gray literature including references from the identified studies, review studies, and conference abstracts which were published up to February 1, 2022. We used all MeSH terms pertaining to “NMOSD,” “NMO,” and all the terms on “prevalence,” “incidence,” and “epidemiology” to identify the search components. Pooled effect sizes were measured using random-effect model by DerSimonian-Laird.
Results
The prevalence and incidence rates of NMOSD/NMO ranged from 0.07 to 10 and 0.029 to 0.880 per 100,000 population, respectively. The overall pooled prevalence of NMO per 100,000 population was 1.54 (I2: 98.4%, 95% CI: 1.13–1.96, P< 0.001) based on the 2006 criteria, 1.51 (I2: 99.4%, 95% CI: 1.21–1.81, P < 0.001) based on the 2015 criteria and 2.16 (I2: 89.4%, 95% CI: 1.46–2.86, P < 0.001) based on the 2006/2015 criteria. The overall annual incidence of NMO per 100,000 population was 0.155 (I2: 95%, 95% CI: 0.115–0.195, P < 0.001) based on the 2006 criteria and 0.278 (I2: 100%, 95% CI: 0.135–0.420, P < 0.001) based on the 2015 criteria. The prevalence rates were highest in French West Indies and South Korea, and lowest in Cuba and Australia, based on the 2006 and 2015 criteria, respectively. Also, the highest annual incidence rates were obtained for Sweden and Slovak republic and the lowest for Cuba and Australia based on the 2006 and 2015 criteria, respectively. All estimated rates were higher among females compared to males.
Conclusion
Although rare, NMOSD/NMO impact affected individuals in devastating ways. Several large-scale prospective studies are required to reach a comprehension of the epidemiological aspects of these notorious demyelinating conditions.





Similar content being viewed by others
Data availability
All of the data will be available for secondary analysis in necessary cases from the corresponding author through an email address.
References
Pandit L, Asgari N, Apiwattanakul M et al (2015) Demographic and clinical features of neuromyelitis optica: a review. Mult Scler 21:845–853
Pandit L, Shetty R, Misri Z et al (2012) Optic neuritis: experience from a south Indian demyelinating disease registry. Neurol India 60:470–475
Papp V, Iljicsov A, Rajda C et al (2018) The Hungarian population-based prevalence and incidence study of neuromyelitis optica spectrum disorder. Mult Scler J 24:75–76
Papp V, Illes Z, Magyari M et al (2018) Nationwide prevalence and incidence study of neuromyelitis optica spectrum disorder in Denmark. Neurology 91:e2265–e2275
Park MS, Kim MK, Kim BJ et al (2011) Benign course in neuromyelitis optica. Mult Scler 17:S63–S64
Peng J-t, Cong H-r, Yan R et al (2015) Neurological outcome and predictive factors of idiopathic optic neuritis in China. J Neurol Sci 349:94–98
Radaelli M, Martinelli V, Moiola L, Da P (2011) Neuromyelitis optica spectrum disorder: the importance of NMO-IgG in clinical practice. J Neurol 258:S101
Rezaeimanesh N, Sahraian MA, Moghadasi AN, Eskandarieh S (2020) Epidemiology of neuromyelitis optica spectrum disorder in Tehran. Iran: the prevalence, baseline characteristics, and clinical aspects:2647–2648
Holroyd KB, Manzano GS, Levy M (2020) Update on neuromyelitis optica spectrum disorder. Curr Opin Ophthalmol 31:462–468
Asgari N, Flanagan EP (2019) Reader response: nationwide prevalence and incidence study of neuromyelitis optica spectrum disorder in Denmark. Neurology 93:722–723
Etemadifar M, Nasr Z, Khalili B, Taherioun M, Vosoughi R (2015) Epidemiology of neuromyelitis optica in the world: a systematic review and meta-analysis. Mult Scler Int 2015:174720
Marrie RA, Gryba C (2013) The incidence and prevalence of neuromyelitis optica: a systematic review. Int J MS Care 15:113–118
Papp V, Magyari M, Aktas O et al (2021) Worldwide incidence and prevalence of neuromyelitis optica. Neurology 96:59
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605
Aboul-Enein F, Seifert-Held T, Mader S et al (2013) Neuromyelitis optica in Austria in 2011: to bridge the gap between neuroepidemiological research and practice in a study population of 8.4 million people. PloS one 8:e79649
Cook LJ, Rose JW, Alvey J et al (2016) A comparison of seropositive and seronegative patients in the Collaborative International Research in Clinical and Longitudinal Experience for NMOSD Studies (CIRCLES) registry. Mult Scler 22:852–853
Asgari N, Lillevang ST, Skejoe HPB, Falah M, Stenager E, Kyvik KO (2011) A population-based study of neuromyelitis optica in Caucasians. Neurology 76:1589–1595
Cabre P, Gonzalez-Quevedo A, Lannuzel A et al (2009) Descriptive epidemiology of neuromyelitis optica in the Caribbean basin. Rev Neurol 165:676–683
Cabre P, Heinzlef O, Merle H et al (2001) MS and neuromyelitis optica in Martinique (French West Indies). Neurology 56:507–514
Lekha P (2008) Neuromyelitis optica antibody (NMO-IgG) status in Indian patients with multiple sclerosis and allied demyelinating disorders. Neurology Asia 13:175–178
Kashipazha D, Mohammadianinejad SE, Majdinasab N, Azizi M, Jafari M (2015) A descriptive study of prevalence, clinical features and other findings of neuromyelitis optica and neuromyelitis optica spectrum disorder in Khuzestan Province. Iran J Neurol 14:204–210
Etemadifar M, Dashti M, Vosoughi R, Abtahi SH, Ramagopalan SV, Nasr Z (2014) An epidemiological study of neuromyelitis optica in Isfahan. Mult Scler:1920–1922
Houzen H, Kondo K, Niino M et al (2017) Prevalence and clinical features of neuromyelitis optica spectrum disorders in northern Japan. Neurology 89:1995–2001
Rivera JF, Kurtzke JF, Booth VJ (2008) Characteristics of Devic’s disease (neuromyelitis optica) in Mexico. J Neurol 255:710–715
Jonsson DI, Sveinsson O, Hakim R, Brundin L (2019) Epidemiology of NMOSD in Sweden from 1987 to 2013: a nationwide population-based study. Neurology 93:e181–e189
Jacob A, Panicker J, Lythgoe D et al (2013) The epidemiology of neuromyelitis optica amongst adults in the Merseyside county of United Kingdom. J Neurol 260:2134–2137
Cossburn M, Tackley G, Baker K et al (2012) The prevalence of neuromyelitis optica in South East Wales. Eur J Neurol 19:655–659
Cabrera-Gmez JA, Kurtzke JF, Gonzlez-Quevedo A, Lara-Rodrguez R (2009) An epidemiological study of neuromyelitis optica in Cuba. J Neurol 256:35–44
Fang C-W, Wang H-P, Chen H-M, Lin J-W, Lin W-S (2020) Epidemiology and comorbidities of adult multiple sclerosis and neuromyelitis optica in Taiwan, 2001-2015. Mult Scler Relat Disord 45:102425
Jarius S, Ruprecht K, Wildemann B et al (2012) Contrasting disease patterns in seropositive and seronegative neuromyelitis optica: a multicentre study of 175 patients. J Neuroinflammation 9:14
Mejdoub S, Feki S, Dammak M et al (2020) Neuromyelitis optica spectrum disorders in South of Tunisia: a rare entity with low seroprevalence of anti-aquaporin 4 autoantibodies. Rev Neurol 176:261–267
Absoud M, Lim MJ, Appleton R et al (2015) Paediatric neuromyelitis optica: clinical. MRI of the brain and prognostic features:470–472
Bukhari W, Prain KM, Waters P et al (2017) Incidence and prevalence of NMOSD in Australia and New Zealand. J Neurol Neurosurg Psychiatry 88:632–638
Bukhari W, Khalilidehkordi E, Mason DF et al (2021) NMOSD and MS prevalence in the Indigenous populations of Australia and New Zealand. J Neurol
Lana-Peixoto MA, Pedrosa D, Talim N, Amaral JMSS, Horta A, Kleinpaul R (2018) Neuromyelitis optica spectrum disorder associated with dengue virus infection. J Neuroimmunol 318:53–55
Lana-Peixoto MA, Talim NC, Pedrosa D, Macedo JM, Santiago-Amaral J (2021) Prevalence of neuromyelitis optica spectrum disorder in Belo Horizonte, Southeast Brazil. Mult Scler Relat Disord 50:102807
Tian D-C, Li Z, Yuan M et al (2021) Incidence of neuromyelitis optica spectrum disorder (NMOSD) in China: a national population-based study (vol 2, 100021, 2020). Lancet Regional Health-Western Pacific 8
Papp V, Illes Z, Magyari M et al The Danish National Epidemiology of Neuromyelitis Optica Spectrum Disorders Based On the 2015 International Panel for NMO Diagnosis (IPND) Criteria. Neurology 2018:90
Papp V, Iljicsov A, Rajda C et al (2020) A population-based epidemiological study of neuromyelitis optica spectrum disorder in Hungary. Eur J Neurol 27:308–317
Papp V, Magyari M, Koch-Henriksen NJ et al (2020) Population-based comparative studies of the epidemiology of neuromyelitis optica spectrum disorder (NMOSD) in Europe. Eur J Neurol 27:461–462
Eskandarieh S, Nedjat S, Abdollahpour I, Moghadasi AN, Azimi AR, Sahraian MA (2017) Comparing epidemiology and baseline characteristic of multiple sclerosis and neuromyelitis optica: a case-control study. Mult Scler Relat Disord 12:39–43
Eskandarieh S, Nedjat S, Azimi AR, Moghadasi AN, Sahraian MA (2017) Neuromyelitis optica spectrum disorders in Iran. Mult Scler Relat Disord 18:209–212
Eskandarieh S, Nedjat S, Azimi AR, Moghadasi AN, Sahraian MA (2018) The prevalence and characteristics of neuromyelitis optica spectrum disorder in Tehran. Iran Multiple Sclerosis Journal 24:NP15–NP16
Seplveda M, Armangu. (2016) Neuromyelitis optica spectrum disorders: Comparison according to the phenotype and serostatus. Neuro:3
Szilasiov. (2021) Incidence and prevalence of neuromyelitis optica spectrum disorders in Slovakia. Neurol Res
Hor JY, Wong CK, Ew JV, Idris S, Tan HJ, Wong DYJ (2021) Neuromyelitis optica spectrum disorder in Asia: epidemiology and risk factors. Neurol Clin Neurosci 9:274–281
Viswanathan S, Wah LM (2019) A nationwide epidemiological study on the prevalence of multiple sclerosis and neuromyelitis optica spectrum disorder with important multi-ethnic differences in Malaysia. Multiple sclerosis 25:1452–1461
Miyamoto K, Fujihara K, Kira J-I et al (2018) Nationwide epidemiological study of neuromyelitis optica in Japan:667–668
Dale GHa. Response to Epidemiology of neuromyelitis optica spectrum disorder”. 2018: 628–629
Miyamoto K, Fujihara K, Kira JI et al (2017) The prevalence and characteristics of neuromyelitis optica in Japan: a nationwide epidemiological study. J Neurol Sci 381:787
Kim J, Seok JM, Lee HJ, Kim BJ, Min JH (2019) Epidemiology of multiple sclerosis and neuromyelitis optica spectrum disorder in South Korea. Mult Scler J 25:610
Aa B (2018) Characteristics of neuromyelitis optica spectrum disorder in a Moroccan population. Mult Scler Relat Disord 26:235
Wingerchuk DM, Banwell B, Bennett JL et al (2015) International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology 85:177–189
Tian D-C, Li Z, Yuan M et al (2020) Incidence of neuromyelitis optica spectrum disorder (NMOSD) in China: a national population-based study. Lancet Regional Health-Western Pacific:2
Viswanathan S (2020) Regional and global perspectives on the incidence of multiple sclerosis and neuromyelitis optica and its spectrum disorders from Asia with emphasis on China. The Lancet regional health Western Pacific 3:100039
Viswanathan S, Rose N, Arip M et al (2018) Multiple sclerosis and neuromyelitis optica spectrum disorders in Malaysia: a comparison in different ethnic groups. Mult Scler Relat Disord 25:300–308
Wang Y, Zhang L, Zhang B et al (2014) Comparative clinical characteristics of neuromyelitis optica spectrum disorders with and without medulla oblongata lesions. J Neurol 261:954–962
Tengsirikomol T, Siritho S, Prayoonwiwat N (2016) How long does it take to diagnose patients with neuromyelitis optica (NMO) using the 2006 diagnostic criteria? Mult Scler Relat Disord 9:14–16
Yanyu C (2020) Familial neuromyelitis optica spectrum disorder in Chinese population: a clinical profile and whole exome sequencing study. Mult Scler J 26:NP73
Yin J, Long Y, Shan F et al (2015) Clinical manifestations of neuromyelitis optica in male and female patients. Neurol Res 37:967–973
Thiel S, Leypoldt F, Roepke L et al (2018) Neuroimmunological Registries in Germany Aktuelle Neurologie 45:7–23
Code availability
Not applicable.
Author information
Authors and Affiliations
Contributions
Conceptualization: O. M.
Data curation: O. M., A. A. S.
Formal analysis: O. M., A. A. S.
Funding acquisition: Not applicable.
Investigation: S. V., M. K., S. B.
Methodology: O. M., S. V., M. K., M. B., S. B.
Project administration: O. M.
Supervision: O. M.
Validation: O. M., A. A. S, VSh.
Visualization: O. M., A. A. S.
Writing—original draft: S. B.
Writing—review and editing: O. M., S. V., EMGh, A. Z., M. B., S. B.
We declare that all co-authors have read and approved the submission.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bagherieh, S., Afshari-Safavi, A., Vaheb, S. et al. Worldwide prevalence of neuromyelitis optica spectrum disorder (NMOSD) and neuromyelitis optica (NMO): a systematic review and meta-analysis. Neurol Sci 44, 1905–1915 (2023). https://doi.org/10.1007/s10072-023-06617-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-06617-y