Abstract
Background
The objectives of this review and meta-analysis of polysomnographic data are those to focus on the clinical use of clonazepam for the management of sleep disorders by re-analyzing clinical trials and randomized clinical trials which have been published in peer-reviewed journals.
Methods
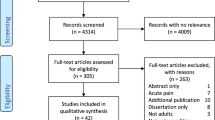
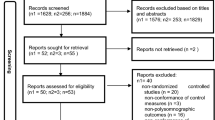
A review of the literature including clinical trials and randomized controlled trials was performed in PubMed®, in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement protocol. A random effects model meta-analysis was then carried out for the four more frequently reported polysomnographic measures: total sleep time, sleep latency, sleep efficiency, and periodic leg movement during sleep (PLMS) index.
Results
A total of 33 articles were retrieved and screened in full text, of which 18 met the criteria for review; among the latter, nine met the criteria for meta-analysis. The studies included in the review involved patients with insomnia, REM sleep behavior disorder, sleep bruxism, and restless leg syndrome or PLMS which reported, most often, an increase in total sleep time with clonazepam. A clear sleep-promoting effect of clonazepam was found also by meta-analysis.
Discussion and conclusions
Our results indicate that the pharmacological treatment of sleep disorders with clonazepam must always be personalized according to the type of patient, the risk of addiction and the concomitant presence of respiratory disorders are key factors to take into account. However, in light of the clinical evidence of the few studies in the literature on the different types of disorders, more studies on the use of clonazepam (also in association with first choice treatments) are definitely needed.


Similar content being viewed by others
References
Fazio C, Manfredi M, Piccinelli A (1975) Treatment of epileptic seizures with clonazepam. A reappraisal. Arch Neurol 32(5):304–307. https://doi.org/10.1001/archneur.1975.00490470048006
Basit H, Kahwaji CI (2021) Clonazepam. In: StatPearls. Treasure Island (FL),
Pinder RM, Brogden RN, Speight TM, Avery GS (1976) Clonazepam: a review of its pharmacological properties and therapeutic efficacy in epilepsy. Drugs 12(5):321–361. https://doi.org/10.2165/00003495-197612050-00001
Marchesi C (2008) Pharmacological management of panic disorder. Neuropsychiatr Dis Treat 4(1):93–106. https://doi.org/10.2147/ndt.s1557
Salem H, Nagpal C, Pigott T, Teixeira AL (2017) Revisiting antipsychotic-induced akathisia: current issues and prospective challenges. Curr Neuropharmacol 15(5):789–798. https://doi.org/10.2174/1570159X14666161208153644
Griffin CE 3rd, Kaye AM, Bueno FR, Kaye AD (2013) Benzodiazepine pharmacology and central nervous system-mediated effects. Ochsner J 13(2):214–223
Battistin L, Varotto M, Berlese G, Roman G (1984) Effects of some anticonvulsant drugs on brain GABA level and GAD and GABA-T activities. Neurochem Res 9(2):225–231. https://doi.org/10.1007/BF00964170
Jenner P, Pratt JA, Marsden CD (1986) Mechanism of action of clonazepam in myoclonus in relation to effects on GABA and 5-HT. Adv Neurol 43:629–643
Petkov V, Georgiev VP, Getova D, Petkov VV (1982) Effects of some benzodiazepines on the acetylcholine release in the anterior horn of the lateral cerebral ventricle of the cat. Acta Physiol Pharmacol Bulg 8(3):59–66
Taft WC, DeLorenzo RJ (1984) Micromolar-affinity benzodiazepine receptors regulate voltage-sensitive calcium channels in nerve terminal preparations. Proc Natl Acad Sci USA 81(10):3118–3122. https://doi.org/10.1073/pnas.81.10.3118
Paulson OB, Gyory A, Hertz MM (1982) Blood-brain barrier transfer and cerebral uptake of antiepileptic drugs. Clin Pharmacol Ther 32(4):466–477. https://doi.org/10.1038/clpt.1982.190
Nelson J, Chouinard G (1999) Guidelines for the clinical use of benzodiazepines: pharmacokinetics, dependency, rebound and withdrawal. Canadian Society for Clinical Pharmacology. Can J Clin Pharmacol = J Can Pharmacol Clin 6(2):69–83
DeVane CL, Ware MR, Lydiard RB (1991) Pharmacokinetics, pharmacodynamics, and treatment issues of benzodiazepines: alprazolam, adinazolam, and clonazepam. Psychopharmacol Bull 27(4):463–473
Dokkedal-Silva V, Berro LF, Galduroz JCF, Tufik S, Andersen ML (2019) Clonazepam: indications, side effects, and potential for nonmedical use. Harv Rev Psychiatry 27(5):279–289. https://doi.org/10.1097/HRP.0000000000000227
Preuss CV, Kalava A, King KC (2020) Prescription of controlled substances: benefits and risks. In: StatPearls. Treasure Island (FL),
Freeman S (1997) The realities of clonazepam discontinuation. Psychiatr Serv 48(7):881–882. https://doi.org/10.1176/ps.48.7.881
Kales A, Manfredi RL, Vgontzas AN, Baldassano CF, Kostakos K, Kales JD (1991) Clonazepam: sleep laboratory study of efficacy and withdrawal. J Clin Psychopharmacol 11(3):189–193
Brown M, Freeman S (2009) Clonazepam withdrawal-induced catatonia. Psychosomatics 50(3):289–292. https://doi.org/10.1176/appi.psy.50.3.289
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8(5):336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Hedges LV, Olkin I (1985) Statistical methods in meta-analysis. J Educ Stat 13(1):75–78
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558. https://doi.org/10.1002/sim.1186
Kontopantelis E, Reeves D (2012) Performance of statistical methods for meta-analysis when true study effects are non-normally distributed: a comparison between DerSimonian-Laird and restricted maximum likelihood. Stat Methods Med Res 21(6):657–659. https://doi.org/10.1177/0962280211413451
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (2019) Cochrane Handbook for Systematic Reviews of Interventions, 2nd edn. John Wiley & Sons, Chichester (UK)
Mowla A, Ahmadzadeh L, Razeghian Jahromi L, Dastgheib SA (2015) Comparing gabapentin with clonazepam for residual sleeping problems following antidepressant therapy in patients with major depressive disorder: a randomized clinical trial. Clin Drug Investig 35(8):513–517. https://doi.org/10.1007/s40261-015-0304-8
Ferri R, Marelli S, Ferini-Strambi L, Oldani A, Colli F, Schenck CH, Zucconi M (2013) An observational clinical and video-polysomnographic study of the effects of clonazepam in REM sleep behavior disorder. Sleep Med 14(1):24–29. https://doi.org/10.1016/j.sleep.2012.09.009
Shin C, Park H, Lee WW, Kim HJ, Kim HJ, Jeon B (2019) Clonazepam for probable REM sleep behavior disorder in Parkinson’s disease: a randomized placebo-controlled trial. J Neurol Sci 401:81–86. https://doi.org/10.1016/j.jns.2019.04.029
Saletu A, Parapatics S, Saletu B, Anderer P, Prause W, Putz H, Adelbauer J, Saletu-Zyhlarz GM (2005) On the pharmacotherapy of sleep bruxism: placebo-controlled polysomnographic and psychometric studies with clonazepam. Neuropsychobiology 51(4):214–225. https://doi.org/10.1159/000085917
Saletu A, Parapatics S, Anderer P, Matejka M, Saletu B (2010) Controlled clinical, polysomnographic and psychometric studies on differences between sleep bruxers and controls and acute effects of clonazepam as compared with placebo. Eur Arch Psychiatry Clin Neurosci 260(2):163–174. https://doi.org/10.1007/s00406-009-0034-0
Boghen D, Lamothe L, Elie R, Godbout R, Montplaisir J (1986) The treatment of the restless legs syndrome with clonazepam: a prospective controlled study. CanJNeurolSci 13(3):245–247
Edinger JD, Fins AI, Sullivan RJ, Marsh GR, Dailey DS, Young M (1996) Comparison of cognitive-behavioral therapy and clonazepam for treating periodic limb movement disorder. Sleep 19(5):442–444
Manconi M, Ferri R, Zucconi M, Bassetti C, Fulda S, Arico D, Ferini-Strambi L (2012) Dissociation of periodic leg movements from arousals in restless legs syndrome. AnnNeurol 71:834–844
Mitler MM, Browman CP, Menn SJ, Gujavarty K, Timms RM (1986) Nocturnal myoclonus: treatment efficacy of clonazepam and temazepam. Sleep 9(3):385–392. https://doi.org/10.1093/sleep/9.3.385
Montagna P, Sassoli DB, Zucconi M, Cirignotta F, Lugaresi E (1984) Clonazepam and vibration in restless legs syndrome. Acta NeurolScand 69(6):428–430
Inami Y, Horiguchi J, Nishimatsu O, Sasaki A, Sukegawa T, Katagiri H, Yamawaki S (1997) A polysomnographic study on periodic limb movements in patients with restless legs syndrome and neuroleptic-induced akathisia. Hiroshima JMedSci 46(4):133–141
Noseda A, Nouvelle M, Lanquart JR, Kempenaers C, De MV, Linkowski R, Kerkhofs M (2002) High leg motor activity in sleep apnea hypopnea patients: efficacy of clonazepam combined with nasal CPAP on polysomnographic variables. RespirMed 96(9):693–699
Peled R, Lavie P (1987) Double-blind evaluation of clonazepam on periodic leg movements in sleep. J Neurol Neurosurg Psychiatry 50(12):1679–1681. https://doi.org/10.1136/jnnp.50.12.1679
Saletu M, Anderer P, Saletu-Zyhlarz G, Prause W, Semler B, Zoghlami A, Gruber G, Hauer C, Saletu B (2001) Restless legs syndrome (RLS) and periodic limb movement disorder (PLMD): acute placebo-controlled sleep laboratory studies with clonazepam. Eur Neuropsychopharmacol: J Eur Coll Neuropsychopharmacol 11(2):153–161
Schenck CH, Mahowald MW (1996) Long-term, nightly benzodiazepine treatment of injurious parasomnias and other disorders of disrupted nocturnal sleep in 170 adults. Am J Med 100(3):333–337. https://doi.org/10.1016/S0002-9343(97)89493-4
Shinno H, Oka Y, Otsuki M, Tsuchiya S, Mizuno S, Kawada S, Innami T, Sasaki A, Hineno T, Sakamoto T, Inami Y, Nakamura Y, Horiguchi J (2010) Proposed dose equivalence between clonazepam and pramipexole in patients with restless legs syndrome. Prog Neuropsychopharmacol Biol Psychiatry 34(3):522–526. https://doi.org/10.1016/j.pnpbp.2010.02.011
Nishimatsu O, Horiguchi J, Inami Y, Sukegawa T, Sasaki A (1997) Periodic limb movement disorder in neuroleptic-induced akathisia. Kobe J Med Sci 43(5):169–177
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Erlbaum, Hillsdale, NJ
Schenck CH, Bundlie SR, Ettinger MG, Mahowald MW (1986) Chronic behavioral disorders of human REM sleep: a new category of parasomnia. Sleep 9(2):293–308. https://doi.org/10.1093/sleep/9.2.293
Raggi A, Ferri R (2010) Sleep disorders in neurodegenerative diseases. Eur J Neurol 17(11):1326–1338. https://doi.org/10.1111/j.1468-1331.2010.03034.x
Mahowald MW, Schenck CH, Cramer Bornemann MA (2005) Sleep-related violence. CurrNeurolNeurosciRep 5(2):153–158
Schenck CH, Lee SA, Bornemann MA, Mahowald MW (2009) Potentially lethal behaviors associated with rapid eye movement sleep behavior disorder: review of the literature and forensic implications. J Forensic Sci 54(6):1475–1484. https://doi.org/10.1111/j.1556-4029.2009.01163.x
Hendricks JC, Morrison AR, Mann GL (1982) Different behaviors during paradoxical sleep without atonia depend on pontine lesion site. Brain Res 239(1):81–105
Fuller PM, Saper CB, Lu J (2007) The pontine REM switch: past and present. J Physiol 584(Pt 3):735–741. https://doi.org/10.1113/jphysiol.2007.140160
Lu J, Sherman D, Devor M, Saper CB (2006) A putative flip-flop switch for control of REM sleep. Nature 441(7093):589–594. https://doi.org/10.1038/nature04767
Figorilli M, Lanza G, Congiu P, Lecca R, Casaglia E, Mogavero MP, Puligheddu M, Ferri R (2021) Neurophysiological aspects of REM sleep behavior disorder (RBD): a narrative review. Brain Sciences 11(12). https://doi.org/10.3390/brainsci11121588
Boeve BF, Silber MH, Saper CB, Ferman TJ, Dickson DW, Parisi JE, Benarroch EE, Ahlskog JE, Smith GE, Caselli RC, Tippman-Peikert M, Olson EJ, Lin SC, Young T, Wszolek Z, Schenck CH, Mahowald MW, Castillo PR, Del TK, Braak H (2007) Pathophysiology of REM sleep behaviour disorder and relevance to neurodegenerative disease. Brain 130(Pt 11):2770–2788
Ferini-Strambi L, Zucconi M (2000) REM sleep behavior disorder. Clin Neurophysiol: Off J Int Fed Clin Neurophysiol 111(Suppl 2):S136-140
Ferini-Strambi L, Fantini ML, Zucconi M, Castronovo V, Marelli S, Oldani A, Cappa S (2005) REM sleep behaviour disorder. Neurol Sci: Off J Italian Neurol Soc Italian Soc Clin Neurophysiol 26(Suppl 3):s186-192. https://doi.org/10.1007/s10072-005-0485-7
Dauvilliers Y, Schenck CH, Postuma RB, Iranzo A, Luppi PH, Plazzi G, Montplaisir J, Boeve B (2018) REM sleep behaviour disorder. Nat Rev Dis Primers 4(1):19. https://doi.org/10.1038/s41572-018-0016-5
Miglis MG, Adler CH, Antelmi E, Arnaldi D, Baldelli L, Boeve BF, Cesari M, Dall’Antonia I, Diederich NJ, Doppler K, Dusek P, Ferri R, Gagnon JF, Gan-Or Z, Hermann W, Hogl B, Hu MT, Iranzo A, Janzen A, Kuzkina A, Lee JY, Leenders KL, Lewis SJG, Liguori C, Liu J, Lo C, Ehgoetz Martens KA, Nepozitek J, Plazzi G, Provini F, Puligheddu M, Rolinski M, Rusz J, Stefani A, Summers RLS, Yoo D, Zitser J, Oertel WH (2021) Biomarkers of conversion to alpha-synucleinopathy in isolated rapid-eye-movement sleep behaviour disorder. Lancet Neurol 20(8):671–684. https://doi.org/10.1016/S1474-4422(21)00176-9
Raggi A, Bella R, Pennisi G, Neri W, Ferri R (2013) Sleep disorders in Parkinson’s disease: a narrative review of the literature. Rev Neurosci 24(3):279–291. https://doi.org/10.1515/revneuro-2013-0002
Giannini G, Provini F, Cortelli P, Calandra-Buonaura G (2021) REM sleep behaviour disorder in multiple system atrophy: from prodromal to progression of disease. Front Neurol 12:677213. https://doi.org/10.3389/fneur.2021.677213
Raggi A, Neri W, Ferri R (2015) Sleep-related behaviors in Alzheimer’s disease and dementia with Lewy bodies. Rev Neurosci 26(1):31–38. https://doi.org/10.1515/revneuro-2014-0050
Antelmi E, Pizza F, Franceschini C, Ferri R, Plazzi G (2020) REM sleep behavior disorder in narcolepsy: a secondary form or an intrinsic feature? Sleep Med Rev 50:101254. https://doi.org/10.1016/j.smrv.2019.101254
Schenck CH, Hurwitz TD, Mahowald MW (1993) Symposium: normal and abnormal REM sleep regulation: REM sleep behaviour disorder: an update on a series of 96 patients and a review of the world literature. J Sleep Res 2(4):224–231
McCarter SJ, St Louis EK, Boswell CL, Dueffert LG, Slocumb N, Boeve BF, Silber MH, Olson EJ, Morgenthaler TI, Tippmann-Peikert M (2014) Factors associated with injury in REM sleep behavior disorder. Sleep Med 15(11):1332–1338. https://doi.org/10.1016/j.sleep.2014.06.002
Antelmi E, Lippolis M, Biscarini F, Tinazzi M, Plazzi G (2021) REM sleep behavior disorder: Mimics and variants. Sleep Med Rev 60:101515. https://doi.org/10.1016/j.smrv.2021.101515
Schaefer C, Kunz D, Bes F (2017) Melatonin effects in REM sleep behavior disorder associated with obstructive sleep apnea syndrome: a case series. Curr Alzheimer Res 14(10):1084–1089. https://doi.org/10.2174/1567205014666170523094938
McGrane IR, Leung JG, St Louis EK, Boeve BF (2015) Melatonin therapy for REM sleep behavior disorder: a critical review of evidence. Sleep Med 16(1):19–26. https://doi.org/10.1016/j.sleep.2014.09.011
Gilat M, Coeytaux Jackson A, Marshall NS, Hammond D, Mullins AE, Hall JM, Fang BAM, Yee BJ, Wong KKH, Grunstein RR, Lewis SJG (2020) Melatonin for rapid eye movement sleep behavior disorder in Parkinson’s disease: a randomised controlled trial. Mov Disord: Off J Mov Disord Soc 35(2):344–349. https://doi.org/10.1002/mds.27886
Jun JS, Kim R, Byun JI, Kim TJ, Lim JA, Sunwoo JS, Lee ST, Jung KH, Park KI, Chu K, Kim M, Lee SK, Jung KY (2019) Prolonged-release melatonin in patients with idiopathic REM sleep behavior disorder. Ann Clin Transl Neurol 6(4):716–722. https://doi.org/10.1002/acn3.753
Kunz D, Mahlberg R (2010) A two-part, double-blind, placebo-controlled trial of exogenous melatonin in REM sleep behaviour disorder. J Sleep Res 19(4):591–596. https://doi.org/10.1111/j.1365-2869.2010.00848.x
St Louis EK, Boeve AR, Boeve BF (2017) REM sleep behavior disorder in Parkinson’s disease and other synucleinopathies. Mov Disord: Off J Mov Disord Soc 32(5):645–658. https://doi.org/10.1002/mds.27018
Jung Y, St Louis EK (2016) Treatment of REM sleep behavior disorder. Curr Treat Options Neurol 18(11):50. https://doi.org/10.1007/s11940-016-0433-2
During EH, Miglis MG (2019) Clinical trials in REM sleep behavior disorder: an urgent need for better evidence. Sleep Med 63:1–2. https://doi.org/10.1016/j.sleep.2019.06.001
Videnovic A, Ju YS, Arnulf I, Cochen-De Cock V, Hogl B, Kunz D, Provini F, Ratti PL, Schiess MC, Schenck CH, Trenkwalder C, Treatment, Trials Working Group of the International RBDSG (2020) Clinical trials in REM sleep behavioural disorder: challenges and opportunities. J Neurol Neurosurg Psychiatry 91(7):740–749. https://doi.org/10.1136/jnnp-2020-322875
Leung AKC, Leung AAM, Wong AHC, Hon KL (2020) Sleep Terrors: an updated review. Curr Pediatr Rev 16(3):176–182. https://doi.org/10.2174/1573396315666191014152136
Chiaro G, Caletti MT, Provini F (2015) Treatment of sleep-related eating disorder. Curr Treat Options Neurol 17(8):361. https://doi.org/10.1007/s11940-015-0361-6
Soca R, Keenan JC, Schenck CH (2016) Parasomnia overlap disorder with sexual behaviors during sleep in a patient with obstructive sleep apnea. J Clin Sleep Med: JCSM: Off Publ Am Acad Sleep Med 12(8):1189–1191. https://doi.org/10.5664/jcsm.6066
Morgenthaler TI, Auerbach S, Casey KR, Kristo D, Maganti R, Ramar K, Zak R, Kartje R (2018) Position paper for the treatment of nightmare disorder in adults: an American Academy of Sleep Medicine position paper. J Clin Sleep Med: JCSM: Off Publ Am Acad Sleep Med 14(6):1041–1055. https://doi.org/10.5664/jcsm.7178
Cochen De Cock V (2016) Sleepwalking. Curr Treat Options Neurol 18(2):6. https://doi.org/10.1007/s11940-015-0388-8
Beddis H, Pemberton M, Davies S (2018) Sleep bruxism: an overview for clinicians. Br Dent J 225(6):497–501. https://doi.org/10.1038/sj.bdj.2018.757
Kato T, Thie NM, Huynh N, Miyawaki S, Lavigne GJ (2003) Topical review: sleep bruxism and the role of peripheral sensory influences. J Orofac Pain 17(3):191–213
Espana A, Clotman F (2012) Onecut factors control development of the Locus Coeruleus and of the mesencephalic trigeminal nucleus. Mol Cell Neurosci 50(1):93–102. https://doi.org/10.1016/j.mcn.2012.04.002
Yoshida A, Moritani M, Nagase Y, Bae YC (2017) Projection and synaptic connectivity of trigeminal mesencephalic nucleus neurons controlling jaw reflexes. J Oral Sci 59(2):177–182. https://doi.org/10.2334/josnusd.16-0845
Fuller PM, Sherman D, Pedersen NP, Saper CB, Lu J (2011) Reassessment of the structural basis of the ascending arousal system. J Comp Neurol 519(5):933–956. https://doi.org/10.1002/cne.22559
Huynh N, Kato T, Rompre PH, Okura K, Saber M, Lanfranchi PA, Montplaisir JY, Lavigne GJ (2006) Sleep bruxism is associated to micro-arousals and an increase in cardiac sympathetic activity. J Sleep Res 15(3):339–346. https://doi.org/10.1111/j.1365-2869.2006.00536.x
Khoury S, Rouleau GA, Rompre PH, Mayer P, Montplaisir JY, Lavigne GJ (2008) A significant increase in breathing amplitude precedes sleep bruxism. Chest 134(2):332–337. https://doi.org/10.1378/chest.08-0115
Andrisani G, Andrisani G (2021) The neurophysiological basis of bruxism. Heliyon 7(7):e07477. https://doi.org/10.1016/j.heliyon.2021.e07477
Manfredini D, Ahlberg J, Winocur E, Lobbezoo F (2015) Management of sleep bruxism in adults: a qualitative systematic literature review. J Oral Rehabil 42(11):862–874. https://doi.org/10.1111/joor.12322
Sakai T, Kato T, Yoshizawa S, Suganuma T, Takaba M, Ono Y, Yoshizawa A, Yoshida Y, Kurihara T, Ishii M, Kawana F, Kiuchi Y, Baba K (2017) Effect of clonazepam and clonidine on primary sleep bruxism: a double-blind, crossover, placebo-controlled trial. J Sleep Res 26(1):73–83. https://doi.org/10.1111/jsr.12442
Melo G, Duarte J, Pauletto P, Porporatti AL, Stuginski-Barbosa J, Winocur E, Flores-Mir C, De Luca CG (2019) Bruxism: an umbrella review of systematic reviews. J Oral Rehabil 46(7):666–690. https://doi.org/10.1111/joor.12801
Manconi M, Garcia-Borreguero D, Schormair B, Videnovic A, Berger K, Ferri R, Dauvilliers Y (2021) Restless legs syndrome. Nat Rev Dis Primers 7(1):80. https://doi.org/10.1038/s41572-021-00311-z
Trenkwalder C, Allen R, Hogl B, Clemens S, Patton S, Schormair B, Winkelmann J (2018) Comorbidities, treatment, and pathophysiology in restless legs syndrome. Lancet Neurol 17(11):994–1005. https://doi.org/10.1016/S1474-4422(18)30311-9
Allen RP, Picchietti DL, Garcia-Borreguero D, Ondo WG, Walters AS, Winkelman JW, Zucconi M, Ferri R, Trenkwalder C, Lee HB, International Restless Legs Syndrome Study G (2014) Restless legs syndrome/Willis-Ekbom disease diagnostic criteria: updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria–history, rationale, description, and significance. Sleep Med 15(8):860–873. https://doi.org/10.1016/j.sleep.2014.03.025
American Academy of Sleep Medicine (2014) International classification of sleep disorders, 3rd ed. American Academy of Sleep Medicine., Darien, IL
Earley CJ, Connor J, Garcia-Borreguero D, Jenner P, Winkelman J, Zee PC, Allen R (2014) Altered brain iron homeostasis and dopaminergic function in restless legs syndrome (Willis-Ekbom Disease). Sleep Med 15(11):1288–1301. https://doi.org/10.1016/j.sleep.2014.05.009
Mogavero MP, Mezzapesa DM, Savarese M, DelRosso LM, Lanza G, Ferri R (2021) Morphological analysis of the brain subcortical gray structures in restless legs syndrome. Sleep Med 88:74–80. https://doi.org/10.1016/j.sleep.2021.10.025
Lanza G, Ferri R (2019) The neurophysiology of hyperarousal in restless legs syndrome: Hints for a role of glutamate/GABA. Adv Pharmacol 84:101–119. https://doi.org/10.1016/bs.apha.2018.12.002
Manconi M, Ferri R, Zucconi M, Oldani A, Fantini ML, Castronovo V, Ferini-Strambi L (2007) First night efficacy of pramipexole in restless legs syndrome and periodic leg movements. Sleep Med 8(5):491–497. https://doi.org/10.1016/j.sleep.2006.10.008
Manconi M, Ferri R, Zucconi M, Clemens S, Giarolli L, Bottasini V, Ferini-Strambi L (2011) Preferential D2 or preferential D3 dopamine agonists in restless legs syndrome. Neurology 77(2):110–117. https://doi.org/10.1212/WNL.0b013e3182242d91
Collado-Seidel V, Kazenwadel J, Wetter TC, Kohnen R, Winkelmann J, Selzer R, Oertel WH, Trenkwalder C (1999) A controlled study of additional sr-L-dopa in L-dopa-responsive restless legs syndrome with late-night symptoms. Neurology 52(2):285–290. https://doi.org/10.1212/wnl.52.2.285
Wetter TC, Stiasny K, Winkelmann J, Buhlinger A, Brandenburg U, Penzel T, Medori R, Rubin M, Oertel WH, Trenkwalder C (1999) A randomized controlled study of pergolide in patients with restless legs syndrome. Neurology 52(5):944–950. https://doi.org/10.1212/wnl.52.5.944
Satija P, Ondo WG (2008) Restless legs syndrome: pathophysiology, diagnosis and treatment. CNS Drugs 22(6):497–518. https://doi.org/10.2165/00023210-200822060-00004
Allen R (2004) Dopamine and iron in the pathophysiology of restless legs syndrome (RLS). Sleep Med 5(4):385–391
Allen RP, Earley CJ (2007) The role of iron in restless legs syndrome. Mov Disord 22 Suppl 18:S440–8.:S440-S448
Earley CJ, Connor JR, Beard JL, Malecki EA, Epstein DK, Allen RP (2000) Abnormalities in CSF concentrations of ferritin and transferrin in restless legs syndrome. Neurology 54(8):1698–1700
Allen RP, Barker PB, Wehrl F, Song HK, Earley CJ (2001) MRI measurement of brain iron in patients with restless legs syndrome. Neurology 56(2):263–265
Earley CJ, Heckler D, Allen RP (2004) The treatment of restless legs syndrome with intravenous iron dextran. Sleep Med 5(3):231–235. https://doi.org/10.1016/j.sleep.2004.03.002
Kemlink D, Sonka K, Pretl M, Benakova H (2007) Suggestive evidence of erythropoietin level abnormality in patients with sporadic and familial cases of the restless legs syndrome. NeuroEndocrinolLett 28(5):643–646
Allen RP (2002) Race, iron status and restless legs syndrome. Sleep Med 3(6):467–468
Winkelmann J, Allen RP, Hogl B, Inoue Y, Oertel W, Salminen AV, Winkelman JW, Trenkwalder C, Sampaio C (2018) Treatment of restless legs syndrome: evidence-based review and implications for clinical practice (Revised 2017)( section sign). Mov Disord: Off J Mov Disord Soc 33(7):1077–1091. https://doi.org/10.1002/mds.27260
DelRosso LM, Mogavero MP, Baroni A, Bruni O, Ferri R (2021) Restless legs syndrome in children and adolescents. Child Adolesc Psychiatr Clin N Am 30(1):143–157. https://doi.org/10.1016/j.chc.2020.08.010
Sateia MJ, Buysse DJ, Krystal AD, Neubauer DN, Heald JL (2017) Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med: JCSM : Off Publ Am Acad Sleep Med 13(2):307–349. https://doi.org/10.5664/jcsm.6470
Riemann D, Baglioni C, Bassetti C, Bjorvatn B, Dolenc Groselj L, Ellis JG, Espie CA, Garcia-Borreguero D, Gjerstad M, Goncalves M, Hertenstein E, Jansson-Frojmark M, Jennum PJ, Leger D, Nissen C, Parrino L, Paunio T, Pevernagie D, Verbraecken J, Weess HG, Wichniak A, Zavalko I, Arnardottir ES, Deleanu OC, Strazisar B, Zoetmulder M, Spiegelhalder K (2017) European guideline for the diagnosis and treatment of insomnia. J Sleep Res 26(6):675–700. https://doi.org/10.1111/jsr.12594
Contreras-Gonzalez N, Tellez-Alanis B, Haro R, Jimenez-Correa U, Poblano A (2015) Executive dysfunction in patients with chronic primary insomnia treated with clonazepam. Neurol Res 37(12):1047–1053. https://doi.org/10.1080/01616412.2015.1114740
Uguz F (2021) A New Safety Scoring System for the Use of Psychotropic drugs during lactation. Am J Ther 28(1):e118–e126. https://doi.org/10.1097/MJT.0000000000000909
Picchietti DL, Hensley JG, Bainbridge JL, Lee KA, Manconi M, McGregor JA, Silver RM, Trenkwalder C, Walters AS (2015) Consensus clinical practice guidelines for the diagnosis and treatment of restless legs syndrome/Willis-Ekbom disease during pregnancy and lactation. Sleep Med Rev 22:64–77. https://doi.org/10.1016/j.smrv.2014.10.009
Funding
Funding for this study was provided by the Italian Ministry of Health Grant RC n. 2773803; the Italian Ministry of Health had no further role in study design, in the collection, analysis and interpretation of data, in the writing of the report, and in the decision to submit the paper for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
None.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Raggi, A., Mogavero, M.P., DelRosso, L.M. et al. Clonazepam for the management of sleep disorders. Neurol Sci 44, 115–128 (2023). https://doi.org/10.1007/s10072-022-06397-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-06397-x